Essentials of Hysteroscopy
Definition
Hysteroscopy is a procedure used to view the inside of the uterus through a telescope-like device called a hysteroscope. The hysteroscope is placed in the vagina and introduced into the uterus.
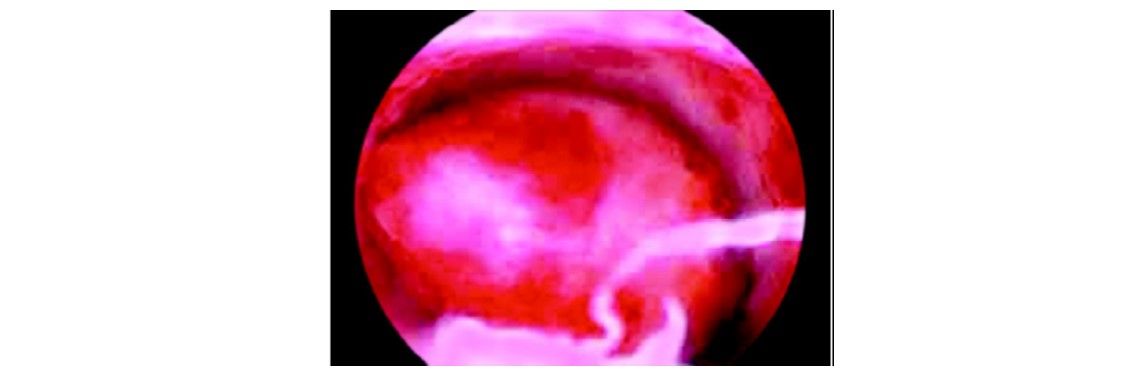
Submucous myoma
Indications
• Abnormal uterine bleeding
• Infertility
• Recurrent pregnancy loss
• Abnormal hysterosalpingogram revealing intrauterine adhesions, polyps, fibroids, septum
• Possible intrauterine foreign bodies.
Contraindications
• Pregnancy
• Heavy uterine bleeding
• Pelvic inflammatory disease
• Cervical malignancy
• Recent uterine perforation.
History
• First hysteroscope with cystoscope of Desormeaux by Pantaleoni 1869
• First hysteroscope with a built-in lens to magnify the image.
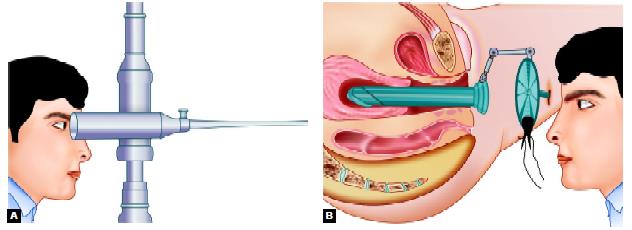
History of hysteroscopy: (A) First hysteroscope with cystoscope of Desormeaux by Pantaleoni; (B) First hysteroscope with built-in lens to magnify the image
Delivery Devices
• Maximum recommended intrauterine operating pressure is 150 mm Hg
• Intrauterine pressure is a function of inflow pressure and outflow pressure
• Inflow pressure may be produced by gravity, pressured cuffs with (pressure) gauges, or approved pumps.
Distending Media
• Group A: Isotonic ionic solutions (Normal saline, Ringer’s lactate)
• Group B: 5% Dextrose in water
• Group C: 1.5% Glycine, sorbitol, cytal
• Group D: Hyskon (32% dextran 70).
Fluid Monitoring
It is the role of the circulating nurse to maintain a flow sheet record of inflow and outflow of hysteroscopic media during the case.
For groups A, B, and C, the inflow and outflow must be estimated for every 500 cc of fluid used and measured at the conclusion of each bag of distending media. For group D, the inflow and outflow must be measured for every 100 cc of fluid used.
The operating surgeon will be informed of fluid balance status as it is recorded on the flow sheet. Spillage should be avoided. The use of a table drape to collect excess fluid for accurate recording of fluid output is required.
Excessive Fluid Absorption
The recommended volume of input to output discrepancy at which point the surgeon must assess serum electrolytes (especially sodium concentration) is:
Group A: 1 liter
Group B: 1 liter
Group C: 1 liter
Group D: 250 ml.
Once these volumes of discrepancy have been reached, serum electrolytes must be obtained and the operating surgeon has the option of:
- Terminating the case: Awaiting the results of the electrolyte levels and proceeding accordingly.
- Administering Lasix IV and judiciously proceeding with the case until the results are available.
Resectoscope
• The resectoscope has been used for male prostate surgery for over 50 years.
• The resectoscope with a built-in wire loop or other shape device uses high-frequency electrical current to cut or coagulate tissue.
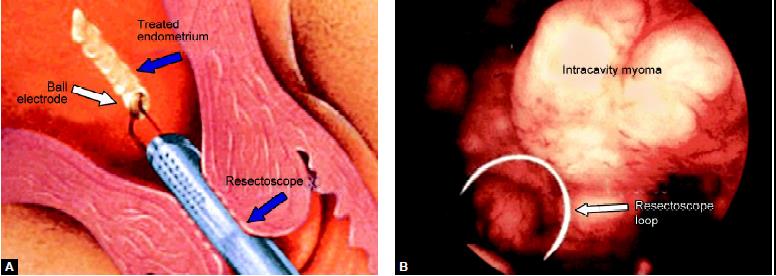
(A) Ball electrode; (B) Resectoscope loop
Procedure

Patient position in hysteroscopy
Inside of the uterus is a potential cavity, like a collapsed air-dome, it is necessary to fill (distend) it with either a liquid or a gas (carbon dioxide) in order to see. Diagnostic hysteroscopy and simple operative hysteroscopy can usually be done in an office setting. More complex operative hysteroscopy procedures are done in an operating room setting.
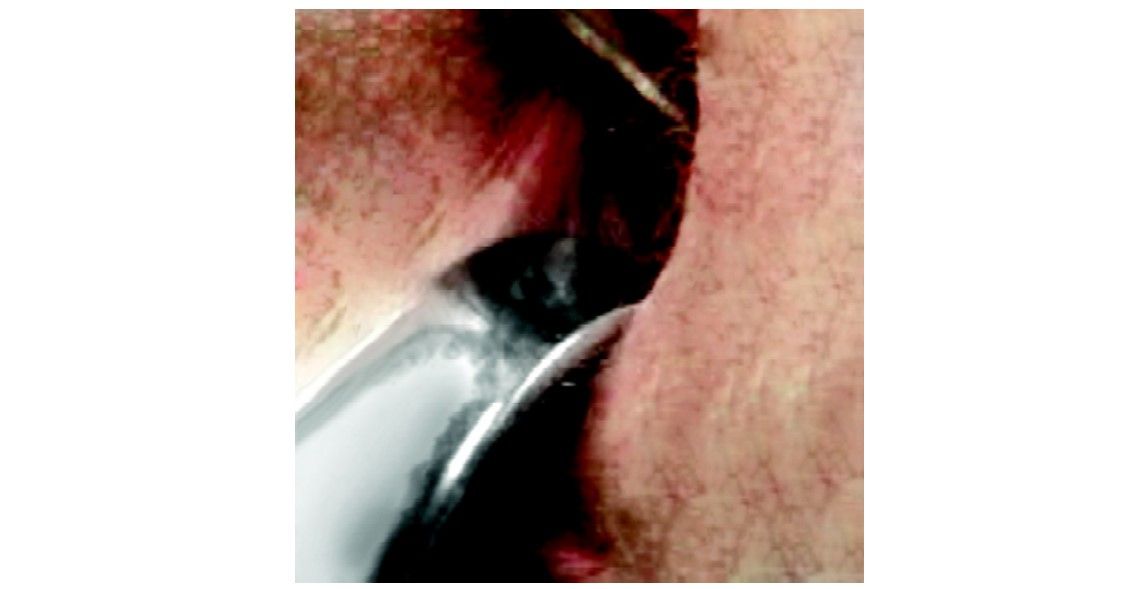
Vaginal speculum
The volumes that are recommended in this section are not based on established “standards of care” since such standards have not yet been clearly formalized. For example, many surgeons use 1 liter as a cut off for D5W while others use 3 liters. There is no established limit for the volume of D5W that can safely be given as an IV solution being directly infused into the circulation of a healthy person. No reports of major morbidity associated with the use of D5W have been reported in the literature.
Additional patient assessment following a large volume discrepancy between input and output may immediately involve the determination of serum electrolytes. If a significant time has passed since the (presumed) absorption of fluid, other clinical parameters (if available) may become more informative (evidence of tissue edema, an increase in cardiac output associated with volume overload, change in pulse oximetry or ventilation parameters, change in patient temperature if room temperature fluid is used.
Use a resectoscope with continuous flow and a loop electrode to perform most of the hysteroscopic surgery. Any of the irrigation system for distending media available today is not sufficiently accurate. They are not rapid in response (so as to maintain a constant pressure), affordable, and easy to use. At present, many gynecologists use a simple system of placing a blood pressure cuff around each one-liter bag of normal saline solution to be used and apply 150 mm Hg pressure as measured on a gauge attached to the cuff to the pressure cuff. This is connected to the inflow port on the resectoscope and flow is then adjustable using a stopcock on this port. Outflow from the resectoscope is via tubing that connects directly to a suction canister under full wall suction. The outflow port also has a stopcock that can be used to adjust the outflow.
The circulating nurse’s primary responsibility during the operative hysteroscopy is to maintain pressure on the pressure cuff and watch the inflow and outflow balance. The nurse might appropriately report this balance to the surgeon and anesthesiologist every 15 minutes or whenever there is a significant volume of use (500 cc).
The resectoscope’s monopolar electrocautery loop is attached to an electrical generator with variable power (wattage) settings. For any given power setting selected, there are also various blends of cutting or coagulation that can be chosen. Use blend 1 which applies current 80 percent of the time and gives just a little coagulation as compared to pure cutting. Most resectoscopes use 50 to 80 watts on blend 1 and coagulate bleeders (if not initially controlled with the blend 1 settings) using 50 watts at pure coagulation.
Once the hysteroscopic portion of the case is completed, a final tabulation of inflow and outflow volumes for the distending media is done. Direct your attention to the laparoscopy once the hysteroscopy is complete. A uterine manipulator is placed through the cervix.
A laparoscope should be inserted now. For this Veress needle is introduced. Insufflation of the abdomen with CO2 gas so as to create a pneumoperitoneum is accomplished after “confirming the proper placement” of the Veress needle. Once the pneumoperitoneum is created, the Veress needle is replaced by a trocar and sleeve. The diameter of the umbilical (main) trocar is 10 to 12 mm so that this instrument can cause considerable injury if not placed properly and atraumatically into the abdominal cavity. The presence of adhesions (scar) that elevates the bowel to the anterior abdominal wall is a consistent source of concern for laparoscopic surgeons.
If abundant adhesions are anticipated such that the surgeon believes that the complication rate with the blind Veress needle and trocar insertion is unacceptably high, then “open laparoscopy” may be chosen. Hasson introduced this technique in which the direct insertion of the trocar without the creation of a prior pneumoperitoneum is accomplished by performing a cut down under direct observation of the layers of the abdominal wall. Suture holds the layers of the inner abdominal wall (fascia and peritoneum) to the trocar sleeve to prevent the release of gas through the incision site during the case. Extreme care must be exercised in making the peritoneal incision since bowel injury to adherent bowel may occur under direct observation as well.
Accessory trocar sites are usually required during the laparoscopic case. Typically, use two additional sites for placement of 5 mm (or uncommonly 10 mm) trocars in the suprapubic midline and left lower quadrant. All accessory trocars have the advantage of being able to be inserted under direct observation so injury is less common. One injury associated with placement of the accessory trocars is laceration of the deep inferior epigastric vessels (which may be difficult to see either directly or via transillumination). Injury to the inferior epigastric vessels can be consistently avoided by the placement of the additional trocars either lateral to the internal inguinal ring or medial to the umbilical ligaments (two structures that are usually easy to identify under direct laparoscopic observation).
Tools that are selected for the performance of the laparoscopic surgery should allow the surgeon to minimize postoperative adhesion formation. The surgical principles as discussed above are very important in terms of achieving the desired outcome. Gentle tissue handling during laparoscopy takes a great deal of time to develop. Avoidance of bleeding with gentle tissue handling is important and so is careful hemostasis using (selective) bipolar cautery. Continuous irrigation and aspiration of the tissues to remove char and minimize drying should be second nature to the laparoscopic infertility surgeon. The use of cutting instruments that minimize lateral tissue damage is also a primary concern.
Once the case has been completed, the instruments are removed from the abdomen allowing for the efflux of CO2 gas. Usually, take an additional 5 or so minutes to move the abdominal wall and contents about with only one remaining trocar sleeve in place to try to allow any trapped gas to escape. Incisions are closed with subcuticular stitches so as to avoid cosmetically unpleasant “railroad” type skin scars. The fascia is closed on any incision in the fascia greater than 5 mm. In the immediate postoperative recovery time period, common problems include nausea and vomiting, most likely related to the CO2 gas or the narcotic pain medications used perioperatively. Zofran is often the most effective antiemetic agent for post laparoscopic vomiting. Nausea and vomiting do not typically persist for more than 12 hours postoperatively.
Shoulder pain due to retained CO2 gas, which is trapped under the diaphragm (at base of the lungs) causes irritation of the phrenic nerve to cause the sensation of shoulder pain. Lying on one’s abdomen with a pillow under the hips and lower abdomen (or the knee-chest position) may allow the CO2 gas to recollect in the pelvis rather than under the lungs and reduce this discomfort. Subcutaneous crepitance (crackling) under the skin over the abdomen and extending superiorly to the chest and neck or inferiorly to the buttocks and thighs is typically a minor complication due to the escape of the gas into the abdominal wall. A rare patient develops a very low blood pressure (not related to blood loss) and usually responds immediately to a bolus of IV solution. Incisional pain is usually mild but the internal (visceral) pain after surgery can be intense and may require narcotics or anti-inflammatory agents. Reportedly a heating pad applied to the abdomen may also be helpful. If a large volume of fluid is left in the abdomen at the conclusion of the case then leakage through the incision sites is common for up to 2 days. The surgeon should be called if there is fever (greater than 100 degrees) or chills, heavy or prolonged vaginal bleeding, heat or swelling of the incision sites, frequency or burning on urination, severe pelvic pain, persistent nausea or vomiting, faintness or dizziness, inability to spontaneously urinate.
Postoperative urinary retention occurs more often in cases that last longer than 2 hours. If the patient is not able to void within 4 to 5 hours postoperative (and after removal of the Foley’s catheter) then she should be straight catheterized for the residual volume of urine and she should try to void spontaneously once again. Do not allow patients to go home until either they can void spontaneously or they have an indwelling Foley catheter placed (for about 1 day).
Definition
Hysteroscopy is a procedure used to view the inside of the uterus through a telescope-like device called a hysteroscope. The hysteroscope is placed in the vagina and introduced into the uterus.
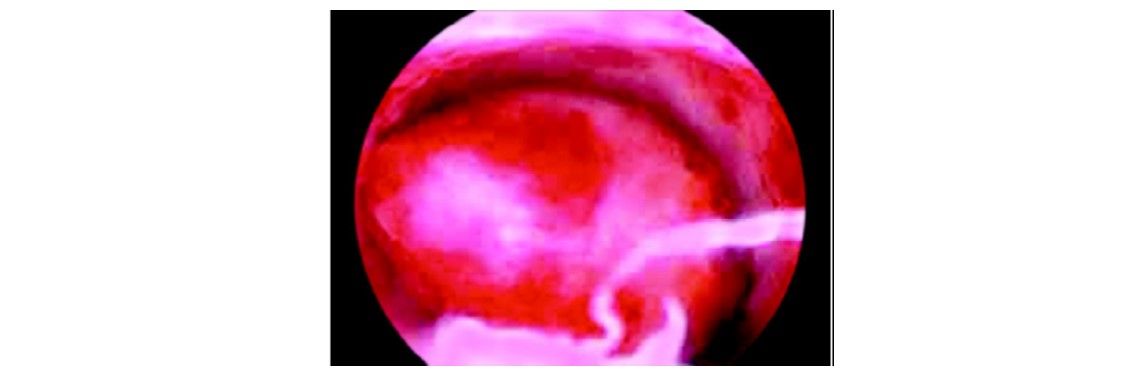
Submucous myoma
Indications
• Abnormal uterine bleeding
• Infertility
• Recurrent pregnancy loss
• Abnormal hysterosalpingogram revealing intrauterine adhesions, polyps, fibroids, septum
• Possible intrauterine foreign bodies.
Contraindications
• Pregnancy
• Heavy uterine bleeding
• Pelvic inflammatory disease
• Cervical malignancy
• Recent uterine perforation.
History
• First hysteroscope with cystoscope of Desormeaux by Pantaleoni 1869
• First hysteroscope with a built-in lens to magnify the image.
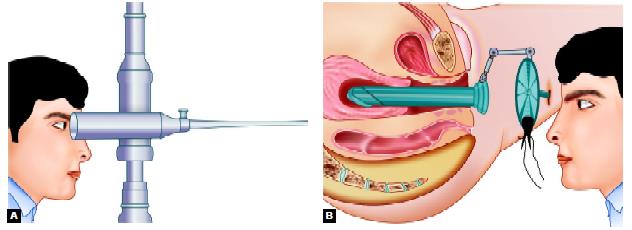
History of hysteroscopy: (A) First hysteroscope with cystoscope of Desormeaux by Pantaleoni; (B) First hysteroscope with built-in lens to magnify the image
Delivery Devices
• Maximum recommended intrauterine operating pressure is 150 mm Hg
• Intrauterine pressure is a function of inflow pressure and outflow pressure
• Inflow pressure may be produced by gravity, pressured cuffs with (pressure) gauges, or approved pumps.
Distending Media
• Group A: Isotonic ionic solutions (Normal saline, Ringer’s lactate)
• Group B: 5% Dextrose in water
• Group C: 1.5% Glycine, sorbitol, cytal
• Group D: Hyskon (32% dextran 70).
Fluid Monitoring
It is the role of the circulating nurse to maintain a flow sheet record of inflow and outflow of hysteroscopic media during the case.
For groups A, B, and C, the inflow and outflow must be estimated for every 500 cc of fluid used and measured at the conclusion of each bag of distending media. For group D, the inflow and outflow must be measured for every 100 cc of fluid used.
The operating surgeon will be informed of fluid balance status as it is recorded on the flow sheet. Spillage should be avoided. The use of a table drape to collect excess fluid for accurate recording of fluid output is required.
Excessive Fluid Absorption
The recommended volume of input to output discrepancy at which point the surgeon must assess serum electrolytes (especially sodium concentration) is:
Group A: 1 liter
Group B: 1 liter
Group C: 1 liter
Group D: 250 ml.
Once these volumes of discrepancy have been reached, serum electrolytes must be obtained and the operating surgeon has the option of:
- Terminating the case: Awaiting the results of the electrolyte levels and proceeding accordingly.
- Administering Lasix IV and judiciously proceeding with the case until the results are available.
Resectoscope
• The resectoscope has been used for male prostate surgery for over 50 years.
• The resectoscope with a built-in wire loop or other shape device uses high-frequency electrical current to cut or coagulate tissue.
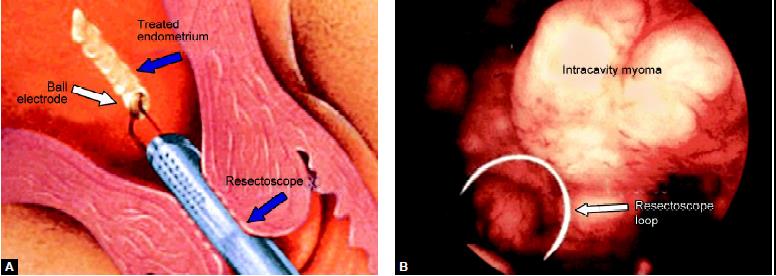
(A) Ball electrode; (B) Resectoscope loop
Procedure

Patient position in hysteroscopy
Inside of the uterus is a potential cavity, like a collapsed air-dome, it is necessary to fill (distend) it with either a liquid or a gas (carbon dioxide) in order to see. Diagnostic hysteroscopy and simple operative hysteroscopy can usually be done in an office setting. More complex operative hysteroscopy procedures are done in an operating room setting.
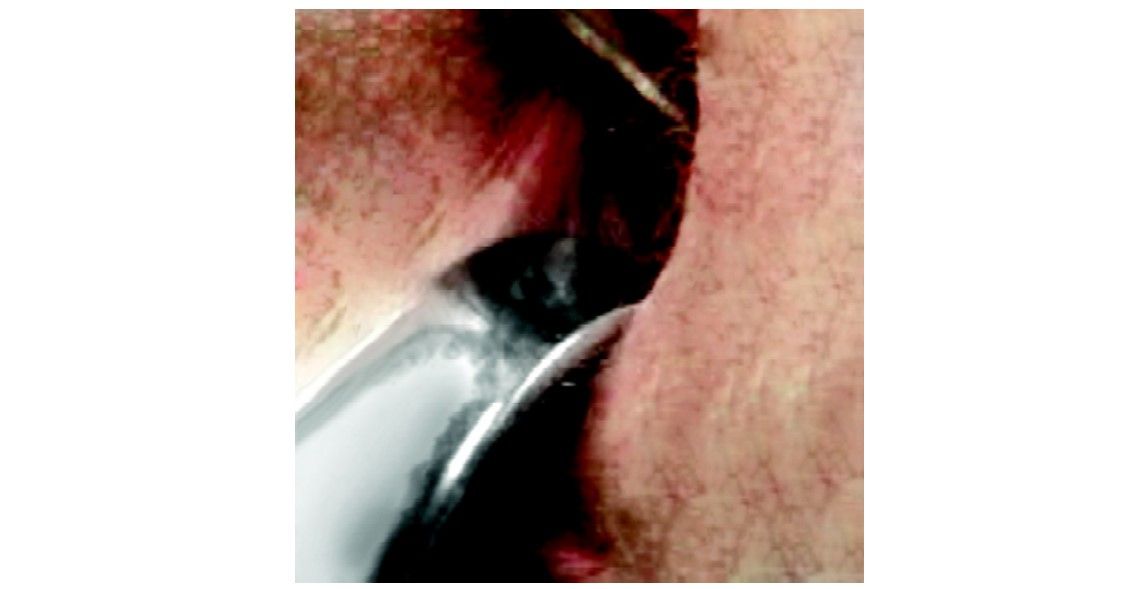
Vaginal speculum
The volumes that are recommended in this section are not based on established “standards of care” since such standards have not yet been clearly formalized. For example, many surgeons use 1 liter as a cut off for D5W while others use 3 liters. There is no established limit for the volume of D5W that can safely be given as an IV solution being directly infused into the circulation of a healthy person. No reports of major morbidity associated with the use of D5W have been reported in the literature.
Additional patient assessment following a large volume discrepancy between input and output may immediately involve the determination of serum electrolytes. If a significant time has passed since the (presumed) absorption of fluid, other clinical parameters (if available) may become more informative (evidence of tissue edema, an increase in cardiac output associated with volume overload, change in pulse oximetry or ventilation parameters, change in patient temperature if room temperature fluid is used.
Use a resectoscope with continuous flow and a loop electrode to perform most of the hysteroscopic surgery. Any of the irrigation system for distending media available today is not sufficiently accurate. They are not rapid in response (so as to maintain a constant pressure), affordable, and easy to use. At present, many gynecologists use a simple system of placing a blood pressure cuff around each one-liter bag of normal saline solution to be used and apply 150 mm Hg pressure as measured on a gauge attached to the cuff to the pressure cuff. This is connected to the inflow port on the resectoscope and flow is then adjustable using a stopcock on this port. Outflow from the resectoscope is via tubing that connects directly to a suction canister under full wall suction. The outflow port also has a stopcock that can be used to adjust the outflow.
The circulating nurse’s primary responsibility during the operative hysteroscopy is to maintain pressure on the pressure cuff and watch the inflow and outflow balance. The nurse might appropriately report this balance to the surgeon and anesthesiologist every 15 minutes or whenever there is a significant volume of use (500 cc).
The resectoscope’s monopolar electrocautery loop is attached to an electrical generator with variable power (wattage) settings. For any given power setting selected, there are also various blends of cutting or coagulation that can be chosen. Use blend 1 which applies current 80 percent of the time and gives just a little coagulation as compared to pure cutting. Most resectoscopes use 50 to 80 watts on blend 1 and coagulate bleeders (if not initially controlled with the blend 1 settings) using 50 watts at pure coagulation.
Once the hysteroscopic portion of the case is completed, a final tabulation of inflow and outflow volumes for the distending media is done. Direct your attention to the laparoscopy once the hysteroscopy is complete. A uterine manipulator is placed through the cervix.
A laparoscope should be inserted now. For this Veress needle is introduced. Insufflation of the abdomen with CO2 gas so as to create a pneumoperitoneum is accomplished after “confirming the proper placement” of the Veress needle. Once the pneumoperitoneum is created, the Veress needle is replaced by a trocar and sleeve. The diameter of the umbilical (main) trocar is 10 to 12 mm so that this instrument can cause considerable injury if not placed properly and atraumatically into the abdominal cavity. The presence of adhesions (scar) that elevates the bowel to the anterior abdominal wall is a consistent source of concern for laparoscopic surgeons.
If abundant adhesions are anticipated such that the surgeon believes that the complication rate with the blind Veress needle and trocar insertion is unacceptably high, then “open laparoscopy” may be chosen. Hasson introduced this technique in which the direct insertion of the trocar without the creation of a prior pneumoperitoneum is accomplished by performing a cut down under direct observation of the layers of the abdominal wall. Suture holds the layers of the inner abdominal wall (fascia and peritoneum) to the trocar sleeve to prevent the release of gas through the incision site during the case. Extreme care must be exercised in making the peritoneal incision since bowel injury to adherent bowel may occur under direct observation as well.
Accessory trocar sites are usually required during the laparoscopic case. Typically, use two additional sites for placement of 5 mm (or uncommonly 10 mm) trocars in the suprapubic midline and left lower quadrant. All accessory trocars have the advantage of being able to be inserted under direct observation so injury is less common. One injury associated with placement of the accessory trocars is laceration of the deep inferior epigastric vessels (which may be difficult to see either directly or via transillumination). Injury to the inferior epigastric vessels can be consistently avoided by the placement of the additional trocars either lateral to the internal inguinal ring or medial to the umbilical ligaments (two structures that are usually easy to identify under direct laparoscopic observation).
Tools that are selected for the performance of the laparoscopic surgery should allow the surgeon to minimize postoperative adhesion formation. The surgical principles as discussed above are very important in terms of achieving the desired outcome. Gentle tissue handling during laparoscopy takes a great deal of time to develop. Avoidance of bleeding with gentle tissue handling is important and so is careful hemostasis using (selective) bipolar cautery. Continuous irrigation and aspiration of the tissues to remove char and minimize drying should be second nature to the laparoscopic infertility surgeon. The use of cutting instruments that minimize lateral tissue damage is also a primary concern.
Once the case has been completed, the instruments are removed from the abdomen allowing for the efflux of CO2 gas. Usually, take an additional 5 or so minutes to move the abdominal wall and contents about with only one remaining trocar sleeve in place to try to allow any trapped gas to escape. Incisions are closed with subcuticular stitches so as to avoid cosmetically unpleasant “railroad” type skin scars. The fascia is closed on any incision in the fascia greater than 5 mm. In the immediate postoperative recovery time period, common problems include nausea and vomiting, most likely related to the CO2 gas or the narcotic pain medications used perioperatively. Zofran is often the most effective antiemetic agent for post laparoscopic vomiting. Nausea and vomiting do not typically persist for more than 12 hours postoperatively.
Shoulder pain due to retained CO2 gas, which is trapped under the diaphragm (at base of the lungs) causes irritation of the phrenic nerve to cause the sensation of shoulder pain. Lying on one’s abdomen with a pillow under the hips and lower abdomen (or the knee-chest position) may allow the CO2 gas to recollect in the pelvis rather than under the lungs and reduce this discomfort. Subcutaneous crepitance (crackling) under the skin over the abdomen and extending superiorly to the chest and neck or inferiorly to the buttocks and thighs is typically a minor complication due to the escape of the gas into the abdominal wall. A rare patient develops a very low blood pressure (not related to blood loss) and usually responds immediately to a bolus of IV solution. Incisional pain is usually mild but the internal (visceral) pain after surgery can be intense and may require narcotics or anti-inflammatory agents. Reportedly a heating pad applied to the abdomen may also be helpful. If a large volume of fluid is left in the abdomen at the conclusion of the case then leakage through the incision sites is common for up to 2 days. The surgeon should be called if there is fever (greater than 100 degrees) or chills, heavy or prolonged vaginal bleeding, heat or swelling of the incision sites, frequency or burning on urination, severe pelvic pain, persistent nausea or vomiting, faintness or dizziness, inability to spontaneously urinate.
Postoperative urinary retention occurs more often in cases that last longer than 2 hours. If the patient is not able to void within 4 to 5 hours postoperative (and after removal of the Foley’s catheter) then she should be straight catheterized for the residual volume of urine and she should try to void spontaneously once again. Do not allow patients to go home until either they can void spontaneously or they have an indwelling Foley catheter placed (for about 1 day).





