Safety Consideration During Use of Electrosurgery in Laparoscopic Surgery
Laparoscopic dissection requires more extensive dissection and thus meticulous hemostasis becomes particularly important. Any loss of view will result in loss of control and hence decreased safety. Hemorrhage, even to a minor extent, tends to obscure their operative field and is to be avoided. This means that vessels of a size that in open surgery could be divided without particular attention need to be secured prior to division when working endoscopically. Dissection must be more meticulous to proceed smoothly to avoid any unacknowledged injury.
The magnification produced by the endoscope may initially confuse the surgeon as to the extent of electrical injury. However, an inexperienced endoscopic surgeon is well advised to convert should he have any doubt about his ability to control the situation expeditiously.
Safety Considerations in MAS
The potential for accidental damage with electrosurgery must always be borne in mind at the time of minimal access surgery. The following are the most commonly encountered problems specific to the minimal access surgery.
• Overshooting
• Overcooking
• Direct coupling
• Capacitive coupling
• Insulation failure.
Overshooting
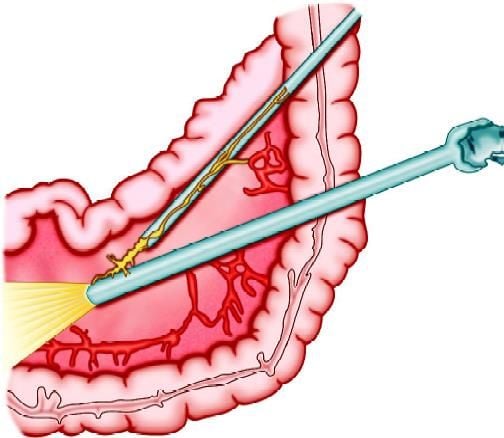
Overshooting means the tip of an energized instrument going beyond the field of vision during electrosurgery. Overshooting is one of the common mistakes done by beginners. The surgeon should be careful that if they are cutting any structure they should apply less force otherwise their instrument will overshoot once the structure is cut and the energized instrument can heat any nearby viscera leading to perforation.
During the initial learning phase of laparoscopy, the trainer surgeon should keep a hold on the hand of the trainee at the time of electrosurgery to prevent any inadvertent injury by overshooting. At the time of laparoscopic cholecystectomy, if hook overshoots it may hit diaphragm or duodenum. If overshooting is not under the control of the surgeon he should try to keep the tip of the hook towards the anterior abdominal wall so that only peritoneum will be injured.
Overcooking
Proper hemostasis requires optimum application of energy over the tissue. Due to visual limitations and fear of impending bleeding, laparoscopic surgeons have a tendency of overcooking. It is important to remember that instead of more secure coagulation overcooking can create rebleeding. To understand the effect of overcooking it is important to know the physiology of tissue sealing.
Coagulation current is high voltage low-frequency current. At this current, the ions inside the cell will move but it can not explode. Due to an increase in intracellular heat, the protein inside the cell will be denatured, coagulated, and shrink. Due to shrinkage of tissue, the lumen of small bleeder obliterates and bleeding stops. At the same time due to heat, the collagen of tissue melts and once the paddle of the electrosurgical generator is of the melted collagen will cool down and solidify.
Overcooking results in charring of melted collagen and the sealing strength of tissue is decreased. It could be understood just by the example of sealing of polythene over a flame of a candle. If you want to seal the polythene bag but applying more temperature on polythene by putting it over direct flame, instead of getting sealed the polythene will start burning. One should know the sealing temperature of polythene so that the required temperature is applied, the polythene will melt and once cooled will solidify. Similarly, the burnt collagen does not have any tissue sealing property, and bleeding may start again if it is overcooked.
Most common causes of overcooking or charring of tissue are:
• High power setting of the electrosurgical generator
• Prolonged activation of foot paddle
• Keeping the jaw closed permanently in contact of tissue
• Poorly engineered electrosurgical generator.
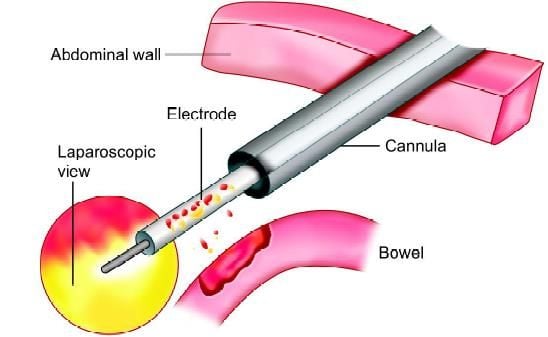
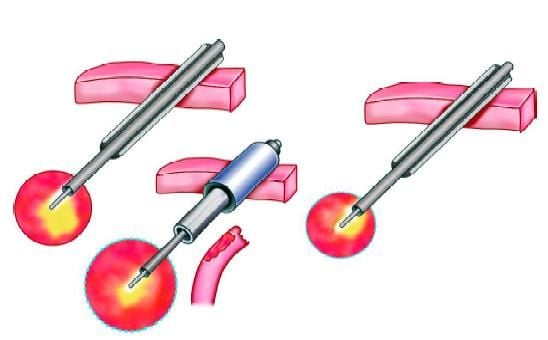
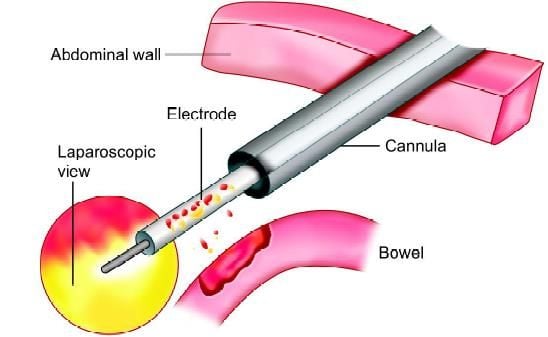
Direct Coupling
If the active electrode touches a non-insulated metal instrument within the abdomen, it will convey energy to the second instrument, which may, in turn, if the current density is high enough, transfer it to surrounding tissues and cause a thermal burn. For example, the active electrode could come in contact or in close proximity (less than 2 mm) to a laparoscope, creating an arc of current between the two. The laparoscope could then brush against surrounding tissue, causing a severe burn to the bowel and other structures. The burns may not be in the visual field of the surgeon and therefore will not be recognized and dealt with in a timely fashion.
To prevent direct coupling, the active electrode should not be in close proximity to or touching another metal instrument before the generator is activated. The bowel is particularly susceptible to this kind of collateral damage from sparks and stray currents. Recognition of this complication may be delayed until the postoperative period with serious consequences. Check that the electrode is touching the target tissue, and only that tissue before you activate the generator. Note that when the target tissue is coagulated (desiccated), the impedance increases and the current may arc to adjacent tissue, following the path of least resistance.
Direct coupling
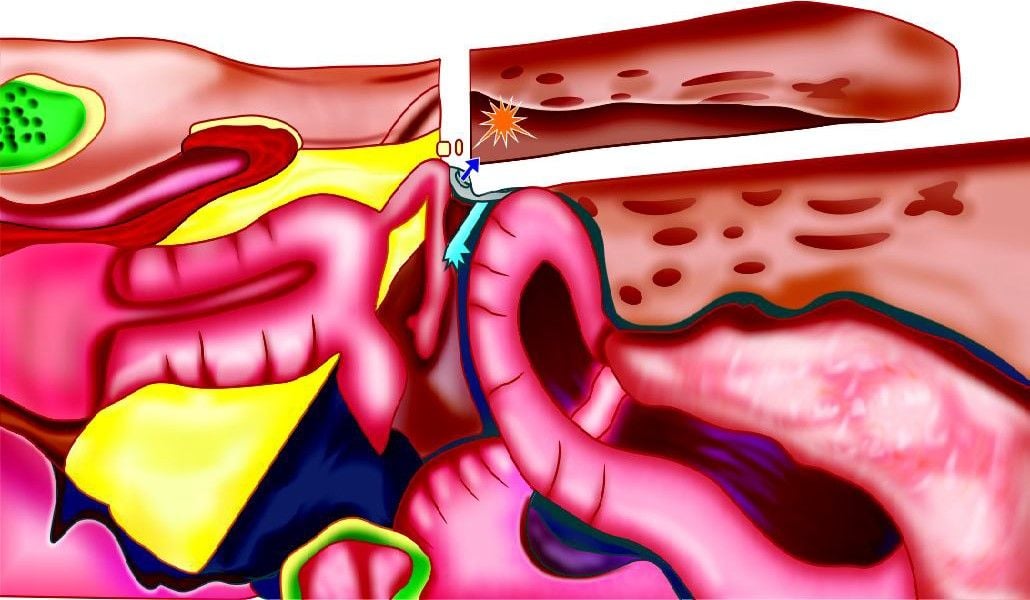
Direct coupling
We should be careful that all metal instruments, such as laparoscopes pass through conductive metal trocars. This way, if the active electrode touches the instrument, the current will simply flow from the instrument to the metal trocar. As long as the trocar is in contact with a relatively large portion of the abdominal wall, the current will not concentrate. Instead, it will dissipate harmlessly from the trocar through the abdomen and back through adjacent tissue to the return electrode. If the trocar is completely or partially constructed of plastic, however, the energy may not be able to dissipate back through the body. The metal within the trocar will build up a charge, which could eventually arc to adjacent tissue and back to the return electrode, but at a harmful level of current. In doing so, it may travel through the bowel, skin, or even the operator’s hands, causing burns. To avoid a direct coupling the surgeon should not activate the generator while the active electrode is touching or in close proximity to another metal object.
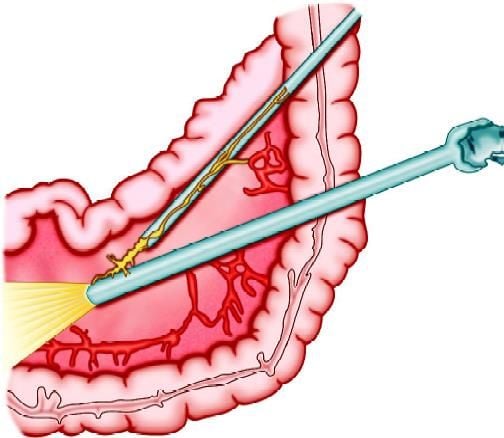
Capacitive Coupling
This now never arise but occurred in the early days of laparoscopic surgery with the use of plastic fixation screws to fix metal ports to the abdominal wall so as to prevent them from being accidentally pulled out or pushed when instruments were withdrawn during the course of an operation. The physics underlying this injury is fairly straight forward. Whenever current is applied through an insulated instrument inserted through a metal trocar (port) some radio frequency electric charge is transferred to the metal cannula by every activation (even if the insulation of the instrument is perfect). This effect is known as capacitance coupling.
There is absolutely no problem if the metal cannula is in contact with the full thickness of the abdominal wall, as the charge accumulated by the cannula is immediately discharged over a wide contact area (low power density, like the neutral return electrode plate) and hence no damage is done.
Capacitive coupling
Burn due to capacitive coupling
However, if the cannula is isolated from the abdominal wall, by a plastic screw (acting as an insulator), the cannula can not discharge and thus accumulates a substantial charge with repeated activation of the electrosurgical instrument. Thus, in essence, it becomes an electric accumulator! Should at any stage, the tip of the cannula inside the abdomen touch tissue or bowel, the accumulated charge will discharge immediately through a single point of contact, i.e. with a high power density sufficient to cause an electrical burn. Since this occurs away from the site of action of the operation, it is usually overlooked. Capacitive coupling is not a problem if plastic fixation screws are not used. The phenomenon of “capacitance” is the ability of two conductors to transmit electrical flow even if they are separated by an intact layer of insulation. Capacitive coupling can occur even in the best-case scenario, that is when the insulation around the active electrode is intact and the tip of the electrode is not touching anything metal. If the active, insulated electrode is wrapped around a towel clamp, or placed inside a metal trocar sleeve, or comes in close contact with any conductive substance for an extended period of time, the current in the active electrode may induce a current in the second conductor.
As long as the induced current can dissipate easily, through a large surface of the tissue, it won’t present a problem. The danger occurs if the second conductor contains some insulating material, as in the case of a metal cannula held in place by a plastic anchor. The plastic anchor will prevent the energy from dissipating and increase the likelihood of a thermal burn. Burns from capacitance current may occur when the surface area is less than 3 cm2 or the current density is approximately 7 W/cm2.
As with direct coupling, the best way to prevent this phenomenon is to use the active electrode monitoring system that prevents current from capacitive coupling from building to dangerous levels. Also, you should avoid all plastic-metal hybrid instruments, including cannulas, trocars, and clamps, when doing electrosurgery.
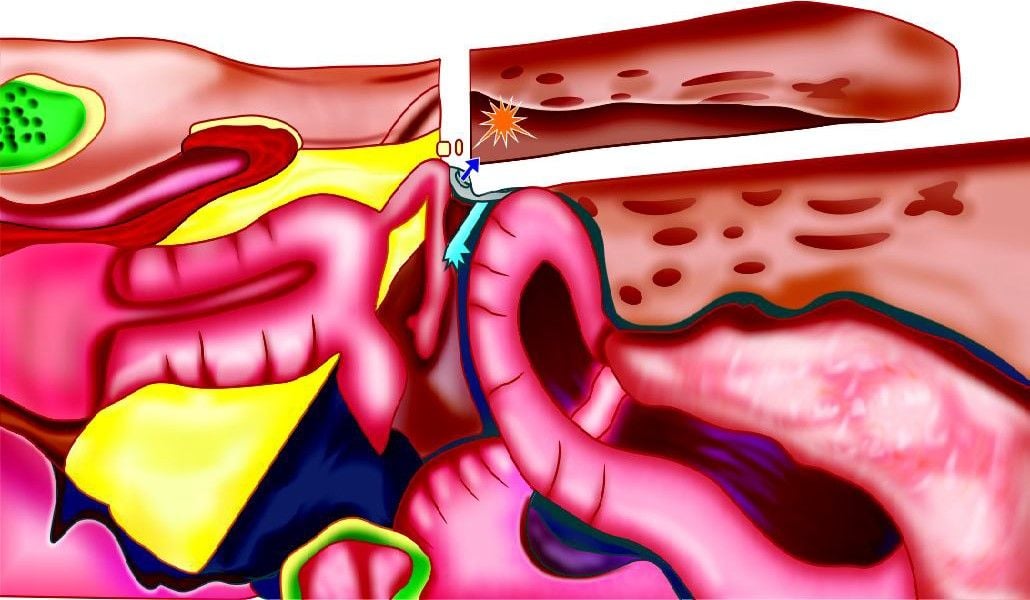
Insulation Failure
During a laparoendoscopic procedure, only about 10 percent of an insulated instrument is visible on the video monitor at any one time, which means about 90 percent of that electrode remains outside the surgeon’s field of view, where it can cause the most damage. Whenever a defective instrument is introduced into the patient, an electric current can escape to contiguous tissue or organs, but the surgeon is not aware that a thermal burn at a peripheral site has occurred. It is estimated that 67 percent of such injuries are not recognized at the time of surgery. Sadly, manifestations of these unsuspected injuries don’t appear until several days after the actual surgery and so, when the impaired patient presents, his or her clinical symptoms are already severe. Diagnosis is difficult and often delayed, and the damage can be irreversible. Complications include perforated bowel diaphragm, urinary bladder, permanent disfigurement, fecal peritonitis cases, etc. Continued regular use of cleaning and sterilization can cause the layer of insulation to cover the shaft of the active electrode to break down. Tiny, visually undetectable tears are actually more dangerous than large cracks, since the current escaping from these minuscule breaks is more concentrated, and therefore capable of causing sparks (averaging 700°C). These sparks can cause severe burns and even ignite fires, especially in oxygen-rich environments. In fact, all insulated electrodes should be considered suspicious, unless adequate safety measures are introduced.
Insulation failure
Unfortunately, many surgeons unknowingly contribute to the problem. Routine use of the high voltage “coagulation” current may actually compromise insulation integrity. The higher the voltage, the greater the risk that the current will break through weak insulation. The surgeon should always use the lowest voltage. All electrosurgery systems will allow you to use a “coagulation” or “cutting” waveform of current. In most cases, we should try to use the cutting current for both cutting and coagulation. The coagulation mode is necessary only when you need to fulgurate or stop diffuse bleeding on highly vascularized tissue. Using the lowest voltage may reduce the wear on the insulation and minimize the chance that the current can escape through hairline cracks.
The surgeon should test for insulation defects in the operating room after the set has been opened. This step can significantly reduce the number of accidental electrosurgical burns because it will prevent a surgeon from inserting a potentially lethal instrument into the patient's abdomen. Insulation that degraded during that final sterilization cycle cannot be detected until this point in time, so it is critical that inspection in the operating room itself be made an integral part of hospital protocol. It is advisable to keep a supply of single-use electrodes available to replace any found to be faulty during the preoperative scan. One can also devise a vigorous and ongoing inspection plan with a qualified technician to ensure that all reusable electrosurgical tools are scanned and reinsulated as needed.
If the instruments are rescanned in the operating room following surgery, the surgeon can be secure in the knowledge, that no stray electrical current escaped into adjacent, but unseen sites, and so if any post-operative clinical complications were to arise, he or she could more easily isolate the cause. Conversely, if the postoperative scan revealed that insulation was damaged during the procedure, he or she may elect to take aggressive steps to investigate further. For documentation purposes, the results of both scans can be recorded in the patient record.
We should always keep in mind that using the cutting current minimizes, but does not eliminate the risk of insulation failure. To really be sure that the insulation is not compromised, it is recommended to use an electrosurgical unit that employs active electrode monitoring (AEM) technology. This technology is called “Electro-Shield” (ElectroScope Inc., Boulder, Colo.) and it virtually eliminates these types of electrical burns.
The traditional system for inspection in the sterile processing department is hardly foolproof, and its weaknesses must be addressed. Because the margin for error is so great, risk managers and physicians alike are insisting on alternatives that will ensure patient safety and reduce liability exposure. Active electrode monitoring protects against thermal burns in two ways. First, it encases the insulated electrode in a protective metal shield that is connected to the generator; the entire probe is also covered with an extra layer of insulation. The extra conductive and insulating layers ensure that the stray current is contained and flows right back to the generator. Second, the system monitors the electrical circuit so if stray energy reaches dangerous levels, the unit shuts off automatically and sounds an alarm before a burn can occur. Electroscope’s AEM system operates on a principle similar to ground fault interrupt (GFI) outlets in our home. It protects against insulation breaks by grounding electricity in unpredictable elements, eliminating stray burns to the patient. This is presently considered the standard of care in endoscopic electrosurgery.
Surgical Smoke
Dissection with electrocautery produces a great deal of smoke. Carbon monoxide at levels as high as 1900 ppm, many times higher than the environmental protection agency standard of 35 ppm for a one-hour exposure, are produced by electrocautery in the hypoxic environment of the carbon dioxide filled abdomen. Fortunately, carbon monoxide is a very insoluble molecule and does not cross the peritoneum. Carbon monoxide absorption is therefore not a problem for patients undergoing laparoscopy. However, contamination by carbon monoxide and other toxic or infectious byproducts of electrocautery may affect the operating room personnel if the smoke is vented into the room.
When an electrosurgical probe heats the tissue and vaporizes cellular fluid, one byproduct is surgical smoke. We know that these fumes, which can contain viral DNA, bacteria, carcinogens, and irritants are malodorous and can cause upper respiratory irritation. We do not yet know whether they are capable of causing cancer or spreading infectious diseases. Surgical smoke can also obscure the operative site and cause the surgeon to inadvertently touch the electrode to non-targeted tissue.
Surgical masks do not adequately filter surgical smoke, the particles are too small. A much better solution is a smoke evacuation system, a high-flow suction, and a filtering device that removes the particles from the air. Two kinds are available commercially. One uses a handheld nozzle, which is intended to be positioned at the surgical site.
To avoid the complication of laparoscopic electrosurgery following important points are:
• Inspect insulation carefully
• Use lowest possible power setting
• Use a low voltage waveform (cut)
• Use brief intermittent activation vs. prolonged activation
• Do not activate in open circuit
• Do not activate in close proximity or direct contact with another instrument
• Use bipolar electrosurgery when appropriate
• Select an all-metal cannula system as the safest choice. Do not use hybrid cannula systems that mix metal with plastic
• Utilize available technology, such as a tissue response generator to reduce capacitive coupling or an active electrode monitoring system, to eliminate concerns about insulation failure and capacitive coupling.
Laparoscopic dissection requires more extensive dissection and thus meticulous hemostasis becomes particularly important. Any loss of view will result in loss of control and hence decreased safety. Hemorrhage, even to a minor extent, tends to obscure their operative field and is to be avoided. This means that vessels of a size that in open surgery could be divided without particular attention need to be secured prior to division when working endoscopically. Dissection must be more meticulous to proceed smoothly to avoid any unacknowledged injury.
The magnification produced by the endoscope may initially confuse the surgeon as to the extent of electrical injury. However, an inexperienced endoscopic surgeon is well advised to convert should he have any doubt about his ability to control the situation expeditiously.
Safety Considerations in MAS
The potential for accidental damage with electrosurgery must always be borne in mind at the time of minimal access surgery. The following are the most commonly encountered problems specific to the minimal access surgery.
• Overshooting
• Overcooking
• Direct coupling
• Capacitive coupling
• Insulation failure.
Overshooting
Overshooting means the tip of an energized instrument going beyond the field of vision during electrosurgery. Overshooting is one of the common mistakes done by beginners. The surgeon should be careful that if they are cutting any structure they should apply less force otherwise their instrument will overshoot once the structure is cut and the energized instrument can heat any nearby viscera leading to perforation.
During the initial learning phase of laparoscopy, the trainer surgeon should keep a hold on the hand of the trainee at the time of electrosurgery to prevent any inadvertent injury by overshooting. At the time of laparoscopic cholecystectomy, if hook overshoots it may hit diaphragm or duodenum. If overshooting is not under the control of the surgeon he should try to keep the tip of the hook towards the anterior abdominal wall so that only peritoneum will be injured.
Overcooking
Proper hemostasis requires optimum application of energy over the tissue. Due to visual limitations and fear of impending bleeding, laparoscopic surgeons have a tendency of overcooking. It is important to remember that instead of more secure coagulation overcooking can create rebleeding. To understand the effect of overcooking it is important to know the physiology of tissue sealing.
Coagulation current is high voltage low-frequency current. At this current, the ions inside the cell will move but it can not explode. Due to an increase in intracellular heat, the protein inside the cell will be denatured, coagulated, and shrink. Due to shrinkage of tissue, the lumen of small bleeder obliterates and bleeding stops. At the same time due to heat, the collagen of tissue melts and once the paddle of the electrosurgical generator is of the melted collagen will cool down and solidify.
Overcooking results in charring of melted collagen and the sealing strength of tissue is decreased. It could be understood just by the example of sealing of polythene over a flame of a candle. If you want to seal the polythene bag but applying more temperature on polythene by putting it over direct flame, instead of getting sealed the polythene will start burning. One should know the sealing temperature of polythene so that the required temperature is applied, the polythene will melt and once cooled will solidify. Similarly, the burnt collagen does not have any tissue sealing property, and bleeding may start again if it is overcooked.
Most common causes of overcooking or charring of tissue are:
• High power setting of the electrosurgical generator
• Prolonged activation of foot paddle
• Keeping the jaw closed permanently in contact of tissue
• Poorly engineered electrosurgical generator.
Direct Coupling
If the active electrode touches a non-insulated metal instrument within the abdomen, it will convey energy to the second instrument, which may, in turn, if the current density is high enough, transfer it to surrounding tissues and cause a thermal burn. For example, the active electrode could come in contact or in close proximity (less than 2 mm) to a laparoscope, creating an arc of current between the two. The laparoscope could then brush against surrounding tissue, causing a severe burn to the bowel and other structures. The burns may not be in the visual field of the surgeon and therefore will not be recognized and dealt with in a timely fashion.
To prevent direct coupling, the active electrode should not be in close proximity to or touching another metal instrument before the generator is activated. The bowel is particularly susceptible to this kind of collateral damage from sparks and stray currents. Recognition of this complication may be delayed until the postoperative period with serious consequences. Check that the electrode is touching the target tissue, and only that tissue before you activate the generator. Note that when the target tissue is coagulated (desiccated), the impedance increases and the current may arc to adjacent tissue, following the path of least resistance.
Direct coupling
Direct coupling
We should be careful that all metal instruments, such as laparoscopes pass through conductive metal trocars. This way, if the active electrode touches the instrument, the current will simply flow from the instrument to the metal trocar. As long as the trocar is in contact with a relatively large portion of the abdominal wall, the current will not concentrate. Instead, it will dissipate harmlessly from the trocar through the abdomen and back through adjacent tissue to the return electrode. If the trocar is completely or partially constructed of plastic, however, the energy may not be able to dissipate back through the body. The metal within the trocar will build up a charge, which could eventually arc to adjacent tissue and back to the return electrode, but at a harmful level of current. In doing so, it may travel through the bowel, skin, or even the operator’s hands, causing burns. To avoid a direct coupling the surgeon should not activate the generator while the active electrode is touching or in close proximity to another metal object.
Capacitive Coupling
This now never arise but occurred in the early days of laparoscopic surgery with the use of plastic fixation screws to fix metal ports to the abdominal wall so as to prevent them from being accidentally pulled out or pushed when instruments were withdrawn during the course of an operation. The physics underlying this injury is fairly straight forward. Whenever current is applied through an insulated instrument inserted through a metal trocar (port) some radio frequency electric charge is transferred to the metal cannula by every activation (even if the insulation of the instrument is perfect). This effect is known as capacitance coupling.
There is absolutely no problem if the metal cannula is in contact with the full thickness of the abdominal wall, as the charge accumulated by the cannula is immediately discharged over a wide contact area (low power density, like the neutral return electrode plate) and hence no damage is done.
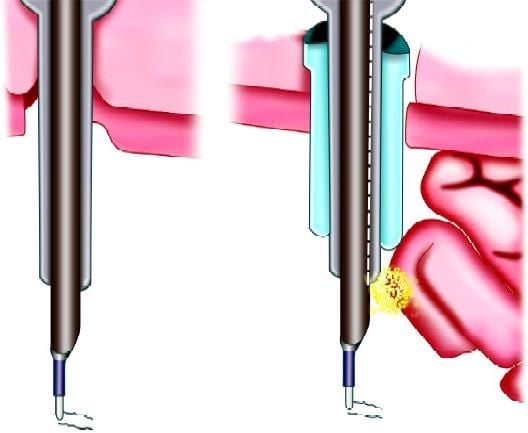
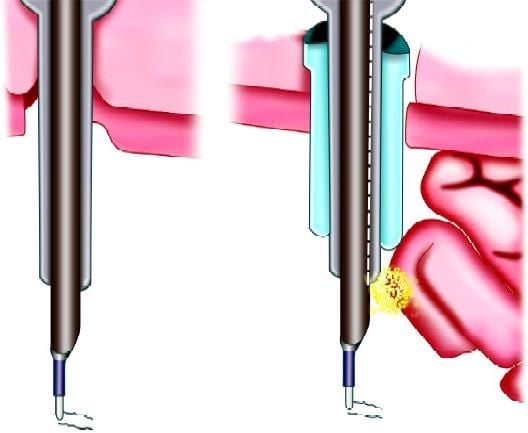
Capacitive coupling
Burn due to capacitive coupling
However, if the cannula is isolated from the abdominal wall, by a plastic screw (acting as an insulator), the cannula can not discharge and thus accumulates a substantial charge with repeated activation of the electrosurgical instrument. Thus, in essence, it becomes an electric accumulator! Should at any stage, the tip of the cannula inside the abdomen touch tissue or bowel, the accumulated charge will discharge immediately through a single point of contact, i.e. with a high power density sufficient to cause an electrical burn. Since this occurs away from the site of action of the operation, it is usually overlooked. Capacitive coupling is not a problem if plastic fixation screws are not used. The phenomenon of “capacitance” is the ability of two conductors to transmit electrical flow even if they are separated by an intact layer of insulation. Capacitive coupling can occur even in the best-case scenario, that is when the insulation around the active electrode is intact and the tip of the electrode is not touching anything metal. If the active, insulated electrode is wrapped around a towel clamp, or placed inside a metal trocar sleeve, or comes in close contact with any conductive substance for an extended period of time, the current in the active electrode may induce a current in the second conductor.
As long as the induced current can dissipate easily, through a large surface of the tissue, it won’t present a problem. The danger occurs if the second conductor contains some insulating material, as in the case of a metal cannula held in place by a plastic anchor. The plastic anchor will prevent the energy from dissipating and increase the likelihood of a thermal burn. Burns from capacitance current may occur when the surface area is less than 3 cm2 or the current density is approximately 7 W/cm2.
As with direct coupling, the best way to prevent this phenomenon is to use the active electrode monitoring system that prevents current from capacitive coupling from building to dangerous levels. Also, you should avoid all plastic-metal hybrid instruments, including cannulas, trocars, and clamps, when doing electrosurgery.
Insulation Failure
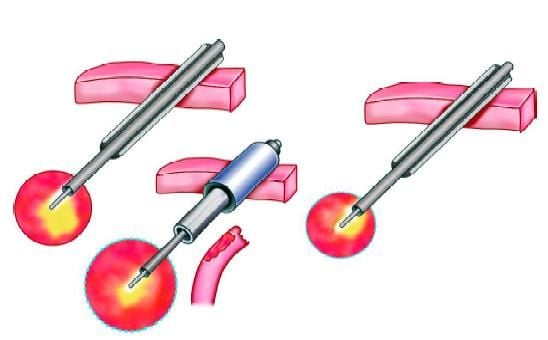
During a laparoendoscopic procedure, only about 10 percent of an insulated instrument is visible on the video monitor at any one time, which means about 90 percent of that electrode remains outside the surgeon’s field of view, where it can cause the most damage. Whenever a defective instrument is introduced into the patient, an electric current can escape to contiguous tissue or organs, but the surgeon is not aware that a thermal burn at a peripheral site has occurred. It is estimated that 67 percent of such injuries are not recognized at the time of surgery. Sadly, manifestations of these unsuspected injuries don’t appear until several days after the actual surgery and so, when the impaired patient presents, his or her clinical symptoms are already severe. Diagnosis is difficult and often delayed, and the damage can be irreversible. Complications include perforated bowel diaphragm, urinary bladder, permanent disfigurement, fecal peritonitis cases, etc. Continued regular use of cleaning and sterilization can cause the layer of insulation to cover the shaft of the active electrode to break down. Tiny, visually undetectable tears are actually more dangerous than large cracks, since the current escaping from these minuscule breaks is more concentrated, and therefore capable of causing sparks (averaging 700°C). These sparks can cause severe burns and even ignite fires, especially in oxygen-rich environments. In fact, all insulated electrodes should be considered suspicious, unless adequate safety measures are introduced.
Insulation failure
Unfortunately, many surgeons unknowingly contribute to the problem. Routine use of the high voltage “coagulation” current may actually compromise insulation integrity. The higher the voltage, the greater the risk that the current will break through weak insulation. The surgeon should always use the lowest voltage. All electrosurgery systems will allow you to use a “coagulation” or “cutting” waveform of current. In most cases, we should try to use the cutting current for both cutting and coagulation. The coagulation mode is necessary only when you need to fulgurate or stop diffuse bleeding on highly vascularized tissue. Using the lowest voltage may reduce the wear on the insulation and minimize the chance that the current can escape through hairline cracks.
The surgeon should test for insulation defects in the operating room after the set has been opened. This step can significantly reduce the number of accidental electrosurgical burns because it will prevent a surgeon from inserting a potentially lethal instrument into the patient's abdomen. Insulation that degraded during that final sterilization cycle cannot be detected until this point in time, so it is critical that inspection in the operating room itself be made an integral part of hospital protocol. It is advisable to keep a supply of single-use electrodes available to replace any found to be faulty during the preoperative scan. One can also devise a vigorous and ongoing inspection plan with a qualified technician to ensure that all reusable electrosurgical tools are scanned and reinsulated as needed.
If the instruments are rescanned in the operating room following surgery, the surgeon can be secure in the knowledge, that no stray electrical current escaped into adjacent, but unseen sites, and so if any post-operative clinical complications were to arise, he or she could more easily isolate the cause. Conversely, if the postoperative scan revealed that insulation was damaged during the procedure, he or she may elect to take aggressive steps to investigate further. For documentation purposes, the results of both scans can be recorded in the patient record.
We should always keep in mind that using the cutting current minimizes, but does not eliminate the risk of insulation failure. To really be sure that the insulation is not compromised, it is recommended to use an electrosurgical unit that employs active electrode monitoring (AEM) technology. This technology is called “Electro-Shield” (ElectroScope Inc., Boulder, Colo.) and it virtually eliminates these types of electrical burns.
The traditional system for inspection in the sterile processing department is hardly foolproof, and its weaknesses must be addressed. Because the margin for error is so great, risk managers and physicians alike are insisting on alternatives that will ensure patient safety and reduce liability exposure. Active electrode monitoring protects against thermal burns in two ways. First, it encases the insulated electrode in a protective metal shield that is connected to the generator; the entire probe is also covered with an extra layer of insulation. The extra conductive and insulating layers ensure that the stray current is contained and flows right back to the generator. Second, the system monitors the electrical circuit so if stray energy reaches dangerous levels, the unit shuts off automatically and sounds an alarm before a burn can occur. Electroscope’s AEM system operates on a principle similar to ground fault interrupt (GFI) outlets in our home. It protects against insulation breaks by grounding electricity in unpredictable elements, eliminating stray burns to the patient. This is presently considered the standard of care in endoscopic electrosurgery.
Surgical Smoke
Dissection with electrocautery produces a great deal of smoke. Carbon monoxide at levels as high as 1900 ppm, many times higher than the environmental protection agency standard of 35 ppm for a one-hour exposure, are produced by electrocautery in the hypoxic environment of the carbon dioxide filled abdomen. Fortunately, carbon monoxide is a very insoluble molecule and does not cross the peritoneum. Carbon monoxide absorption is therefore not a problem for patients undergoing laparoscopy. However, contamination by carbon monoxide and other toxic or infectious byproducts of electrocautery may affect the operating room personnel if the smoke is vented into the room.
When an electrosurgical probe heats the tissue and vaporizes cellular fluid, one byproduct is surgical smoke. We know that these fumes, which can contain viral DNA, bacteria, carcinogens, and irritants are malodorous and can cause upper respiratory irritation. We do not yet know whether they are capable of causing cancer or spreading infectious diseases. Surgical smoke can also obscure the operative site and cause the surgeon to inadvertently touch the electrode to non-targeted tissue.
Surgical masks do not adequately filter surgical smoke, the particles are too small. A much better solution is a smoke evacuation system, a high-flow suction, and a filtering device that removes the particles from the air. Two kinds are available commercially. One uses a handheld nozzle, which is intended to be positioned at the surgical site.
To avoid the complication of laparoscopic electrosurgery following important points are:
• Inspect insulation carefully
• Use lowest possible power setting
• Use a low voltage waveform (cut)
• Use brief intermittent activation vs. prolonged activation
• Do not activate in open circuit
• Do not activate in close proximity or direct contact with another instrument
• Use bipolar electrosurgery when appropriate
• Select an all-metal cannula system as the safest choice. Do not use hybrid cannula systems that mix metal with plastic
• Utilize available technology, such as a tissue response generator to reduce capacitive coupling or an active electrode monitoring system, to eliminate concerns about insulation failure and capacitive coupling.





