Patient Monitoring in Laparoscopic Surgery
Careful monitoring of a patient undergoing a laparoscopic surgical procedure is very important. Monitoring has certain elements in common for all patients. Others are more specific to patients with cardiopathy. A multi-parameter monitor is essential and minimum parameters are important to look for:
• ECG
• Rate of respiration
• SpO2
• NIBP
• Temperature
• Pulse rate
• Cardiac output
• EtCO2

Multiparameter monitor

Capnograph
Routine Monitoring
The stethoscope remains an important instrument enabling anesthetist to auscultate both the lungs after any change in position and after insufflation of the pneumoperitoneum, because it pushes back the tracheal carina, can displace intubation to the right. The use of a stethoscope in the precordial position is a good practice in order to detect gas embolism but requires permanent auscultation.
Electrocardioscopic monitoring during laparoscopy enables arrhythmia, which may occur due to hypercapnia, to be rapidly detected. At the time of laparoscopic surgery, the sudden appearance of a micro voltage can be the sign of subcutaneous emphysema or pneumomediastinum.
Oximetry monitoring (SpO2) is an essential part of any surgery but it is especially important in laparoscopic surgery because of the dim lighting in the laparoscopic surgery theater and the wearing of protective glasses if a laser is being used make it difficult to recognize cyanosis. In any case, the latter is a late clinical sign of hypoxia. Variations in saturation are not specific during laparoscopic surgery. Desaturation is a late sign of complications such as gas embolism, pneumothorax, selective intubation, or a shunt effect due to excessively high intraperitoneal pressure.
During laparoscopic surgery, control of intraperitoneal pressure is an integral part of the anesthesia monitoring. The insufflator must be microprocessor controlled; it must be reliable and subjected to regular checks. Excessive intraperitoneal pressure must trigger an alert and an immediate halt in insufflation. As the majority of older insufflators do not have a safety valve for a reduction in intraperitoneal pressure, this must be carried out by manual exsufflation via opening the valve of the cannula.
The monitoring of the neuromuscular block is also important. Proper relaxation is good for laparoscopic surgery. Stable and deep myoresolution improves the laparoscopic surgeon’s view and limits the peritoneal insufflation pressures. In addition, the wide range of operating times and the rapidity with which an operation is terminated means it is essential to know exactly what the neuromuscular block situation is at any point in time. When equipment for reading the muscular activity in the thumb is not available, the simplest stimulation is a train of four on a temporal branch of the facial nerve and observation of the contraction of the orbicular eye muscle.
Intraperitoneal insufflation of dry and unheated gas, possibly accompanied by irrigation with cold liquids results in heat loss during laparoscopic surgery which is at least equal to that with laparotomy. Temperature monitoring associated with measures to combat heat loss is also essential when procedures take several hours. It is important to remember that excessive leakage of gas through the cannula causes rapid hypothermia to the patient.
Cardiovascular Monitoring
Measurement via the bloodstream enables arterial pressure to be monitored in real-time. In addition, the appearance of cyclic variations in time with ventilation is an excellent indication of drops in preloading which prompts the intraperitoneal insufflation pressure to be limited, to increase filling, or even to accentuate the Trendelenburg’s position when possible. Installation of an arterial entry point also helps with blood gas measurements.
Measurement of central venous pressure is traditionally used to supervise the filling pressures in the right heart. This becomes difficult during laparoscopic surgery because of the changes in the position which require continual changes at the cell level, and particularly because of the increase in intrathoracic pressure transmitted from the peritoneal area via the diaphragm. It is important to perform simultaneous measurement of intrathoracic pressure which is obtained by esophageal pressure and to deduct this from the measured central venous pressure.
Catheterization of the right heart using a Swan Ganz probe has been used for monitoring during laparoscopic surgery. As for central venous pressure, the values measured need to be corrected according to the intrathoracic pressure. An increase in pulmonary arterial pressure is an early sign of gas embolism. Aspiration of the gas bubbles by the proximal orifice placed in the right atrium theoretically helps to minimize the consequences of air embolism. The use of a Swan Ganz probe during laparoscopy for patients with the coronary disease helps adapt the anesthesia protocol and therapy, for simple measurement of arterial pressure is insufficient in 80 percent of these cases. Nevertheless, in the course of general anesthesia with controlled ventilation when SaO2, hemoglobin, and oxygen consumption are stable, a change in SvO2 is often the sign of a change in cardiac flow rate.
Because right heart catheterization is an invasive procedure, several studies have reported the use of cardiac flow rate monitoring by electrical bio-impedance during laparoscopic surgery. The principle is founded on continuous measurement of the blood flow rate in the thorax by analysis of the variations in conductivity relative to an electrical field. Transthoracic electrical bio-impedance brings a certain number of advantages:
• Low-risk (non-invasive monitoring)
• Easy and simple to use
• Continuous measurement in real-time
• Not limited in time
• Inexpensive
• Reliability seems to be satisfactory compared to other methods.
It is important that the skin be carefully prepared and the electrodes are of good quality and correctly positioned.
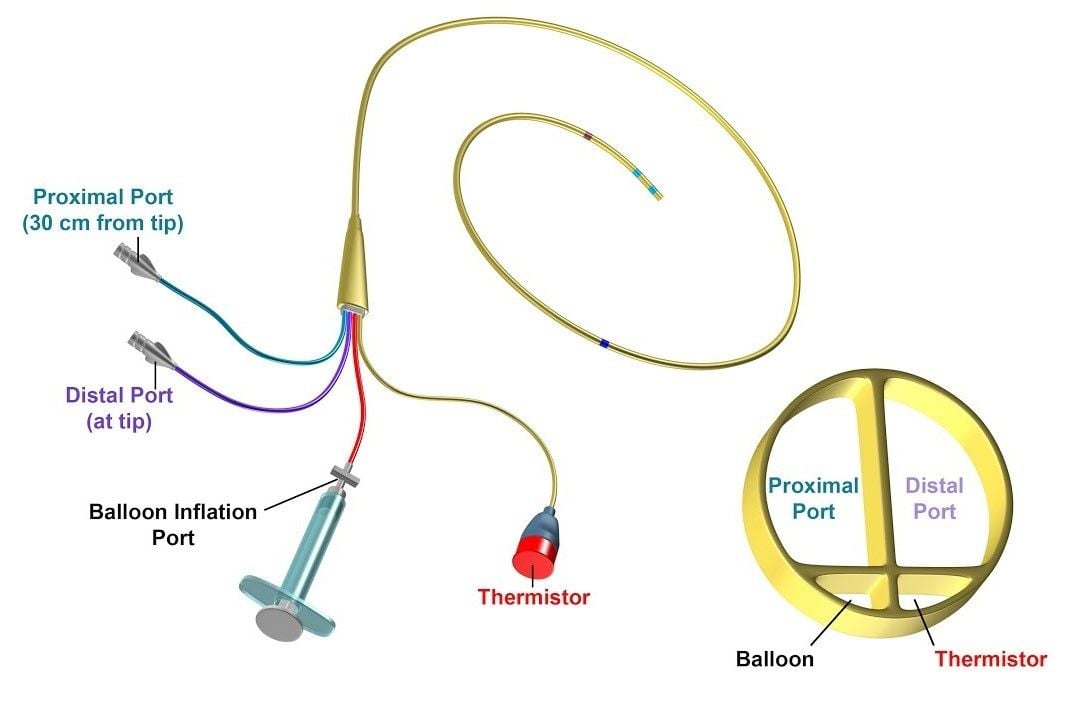
Swan Ganz catheter
However, its use in standard monitoring is still limited due in large part to the frequent difficulties encountered in interpreting the variations. Some studies have been made of hemodynamic monitoring during laparoscopic surgery using transesophageal ultrasound cardiography. Whereas the advantages of this technique for monitoring and diagnosis are considerable, the cost remains an important barrier. Interpretation can also be difficult because of the variations in the viewing axis of the heart according to peritoneal pressure and the variable patient’s position.
Measurement of the cardiac flow rate by pulsed Doppler velocimetry can be carried out by either the transesophageal or the supra-sternum route at the time of laparoscopic surgery. The basic principle is the same as with any Doppler device with a piezoelectric transducer transmitter and a transducer receiver which receives the return echoes modified by the Doppler effect when they bounce off mobile structures like the wall of the heart, vessels or red blood cells. Based on the effective diameter of the aorta which can either be calculated from the cardiac flow rate measured by another method or estimated from the patient's biometric factors, the ejection volume can be deduced and thus the continuous cardiac flow rate.
Respiratory Monitoring
Quantitative waveform capnography is the continuous, noninvasive measurement and graphical display of end-tidal carbon dioxide (ETCO2, also called PetCO2). Capnography uses a sample chamber/sensor placed for optimum evaluation of expired CO2. The inhaled and exhaled carbon dioxide is graphically displayed on a capnograph as a waveform on the monitor along with its corresponding numerical measurement.
As an assessment tool during laparoscopic surgery, capnography can help the anesthetist determine the number of things. It is a direct measurement of ventilation in the lungs, CO2 absorption causing hypercarbia and it also indirectly measures metabolism and circulation. For example, an increase in CO2 absorption during laparoscopy will increase the ETCO2 and a decrease in perfusion will lower the delivery of carbon dioxide to the lungs. This will cause a decrease in the ETCO2 (end-tidal CO2), and this will be observable on the waveform as well as with the numerical measurement. Capnography is a continuous and noninvasive method for carbon dioxide (CO2) measurement, and it has become the standard of care for basic respiratory monitoring for intubated patients during laparoscopic surgery. The CO2 end-tidal pressure (PetCO2) provides evidence of the production of carbon dioxide by cellular metabolism, absorbed through the peritoneal cavity and pulmonary exchanges. A rapid increase in PetCO2 is a serious complication. Thus, Continuous and careful monitoring of EtCO2 by Capnography is a useful and effective noninvasive monitoring technique in anesthesia for laparoscopy. The EtCO2 immediately reflects changes in circulatory status and ventilation as well as detects complications related to CO2 pneumoperitoneum (Hypercarbia, Subcutaneous emphysema, Gas embolism, Pneumothorax, etc.) Thus, EtCO2 monitoring is mandatory and essential monitoring during laparoscopic surgery for the safe conduct of general anesthesia.

Portable CO2 monitor
• A rapid rise of a few millimeters of mercury returning a few minutes later to the base figures may be the sign of minimal CO2 gas embolism.
• A more gradual and persistent rise is often the sign of extraperitoneal diffusion of CO2 (preperitoneal, subcutaneous, retroperitoneal, mediastinal, etc.). This increase in expired CO2 continues after exsufflation of the pneumoperitoneum, indeed often several hours after the laparoscopic procedure, justifying a follow-up of hypercapnia in the recovery room.
• The CO2 is transported by the circulatory system from the peripheral areas towards the lungs. Any disturbance in the circulation will reduce the CO2 expired. A rapid drop in PetCO2 may be the sign of a drop in cardiac flow rate or a decreased venous return, but also pulmonary arterial obliteration. This is what happens in massive gas embolism which shows up as a drop-in PetCO2 proportional in size and duration to the volume of the CO2 embolus.
Classically the PetCO2 values are 2 to 6 mm Hg lower than PaCO2. During anesthesia with artificial ventilation, the ventilation/perfusion ratio of often greater than 1, so a PaCO2-PetCO2 gradient of 10 to 15 mm Hg must be expected. However, during laparoscopic surgery, the change in the arterial CO2-ETCO2 gradient is very variable.
Changes in a position such as the Trendelenburg’s or the lateral reclined position can modify the value of the PetCO2. Furthermore, it is shown that in cases of cardiovascular disease, the correlation between PetCO2 and PaCO2 was less good when compared with patients with no such pathology, and the same is true with obese patients. A recent study confirms that in patients with respiratory impairment; the increases in PaCO2 are underestimated by PetCO2. So for these patients with respiratory or heart pathology, it is particularly useful to duplicate the PetCO2 measurement by arterial gasometry at the beginning of the operation and every time there is an important variation in PetCO2.
In view of this uncertainty, transcutaneous CO 2 monitoring would give a better idea of PaCO2, but this also raises a certain number of technical problems (heating of electrodes, difficulties with measurements in adults, etc.). The anesthetist should keep the following points in mind at the time of laparoscopic surgery:
• The patient voids urine just prior to entering the operating room.
• No shaving is necessary.
• All patients undergoing laparoscopy should have an empty bowel. In the unlikely event of bowel damage, there is much less risk of contamination if the bowel is empty.
• The position of leg is important considering a different laparoscopic procedure. Pressure stocking prevents DVT.
• Good muscle relaxation reduces the intra-abdominal pressure required for the adequate working room in the abdominal cavity.
• The inflation of the stomach should be avoided during artificial ventilation using a mask as this increases the risk of gastric injury during trocar insertion or instrumentation.
• The distended stomach also hampers the visibility of Calot’s triangle at the time of laparoscopic cholecystectomy or laparoscopic bile duct surgery.
• Tracheal intubation and intermittent positive pressure ventilation should be routinely used. This ensures airway protection and controls pulmonary ventilation to avoid hypocarbia.
• The ventilatory pattern should be adjusted according to the respiratory and hemodynamic performance of the individual patient.
• Ventilation with large tidal volumes (12–15 ml/kg) prevents alveolar atelectasis and hypoxemia and allows adequate alveolar ventilation and CO2 elimination.
• Halothane increases the incidence of arrhythmia during
laparoscopic surgery especially in the presence of hypercarbia.
• Isoflurane is the preferred volatile anesthetic agent in minimal access surgery as it has less arrhythmogenic and myocardial depressant effects.
• Patients should receive adequate airway humidification and protection against unintentional hypothermia because generally, the duration of the operation is more in laparoscopic surgery.
• Excessive intravenous sedation should be avoided because it diminishes airway reflexes against pulmonary aspiration in the event of regurgitation.
• Monitoring of PetCO2 is mandatory during laparoscopic surgery. The continuous monitoring of PetCO2 allows adjustment of the minute ventilation to maintain a normal concentration of carbon dioxide and oxygen.
• Airway pressure monitor is mandatory for anesthetized patients receiving intermittent positive pressure ventilation.
Postoperative Considerations
At the end of the procedure, antagonism of the residual muscle relaxation should be reversed by an appropriate dose of neostigmine. When the patient is awake he or she should be extubated and transferred to the recovery room in a semi-recumbent position. Before extubation, the patient’s stomach may be emptied with an orogastric tube. During the next five hours in the postoperative period, analgesia should be achieved. Patients spend a minimum of an hour in the recovery room. Vital signs and O2 saturation are monitored and supplemental O2 is administered by mask or nasal prongs.
Nausea is frequent after general anesthesia. Intravenous droperidol, ondansetron, or metoclopramide can be administered if nausea persists. Vomiting is also common after recovery from anesthesia. Ondem or vomiset, given half an hour before a reversal agent is very helpful in preventing postoperative nausea and vomiting.
The urine output should be at a rate of 100 ml/h and that should continue for 18 hours postoperatively. The nursing management included oxygen therapy, early mobilization, incentive spirometry, and chest physiotherapy. These should repeat at 2 hours interval. She or he should be transferred to the surgical ward and may be discharged home the next day if everything is alright. On the morning of the first postoperative day, the patient should be mobile, pain-free, and should start a soft diet.
It is very common to expect some pain after the procedure. Shoulder pain may occur as a result of distension of the abdomen with gas. As the gas absorbs into the bloodstream and is exhaled through the lungs the pain will gradually disappear, usually over 24 or 48 hours. Depending on the surgery carried out, there may be some interference in bowel function leading to abdominal distension and colicky discomfort. Tramadol hydrochloride is effective for these types of pain. An initial loading dose of these analgesics if administered can give smooth painless recovery.
All procedures under anesthesia carry small but inherent risks and the patient should understand these before agreeing to undergo the procedure. However, the risks of anesthesia for elective surgery under modern conditions are very small indeed.
Careful monitoring of a patient undergoing a laparoscopic surgical procedure is very important. Monitoring has certain elements in common for all patients. Others are more specific to patients with cardiopathy. A multi-parameter monitor is essential and minimum parameters are important to look for:
• ECG
• Rate of respiration
• SpO2
• NIBP
• Temperature
• Pulse rate
• Cardiac output
• EtCO2

Multiparameter monitor

Capnograph
Routine Monitoring
The stethoscope remains an important instrument enabling anesthetist to auscultate both the lungs after any change in position and after insufflation of the pneumoperitoneum, because it pushes back the tracheal carina, can displace intubation to the right. The use of a stethoscope in the precordial position is a good practice in order to detect gas embolism but requires permanent auscultation.
Electrocardioscopic monitoring during laparoscopy enables arrhythmia, which may occur due to hypercapnia, to be rapidly detected. At the time of laparoscopic surgery, the sudden appearance of a micro voltage can be the sign of subcutaneous emphysema or pneumomediastinum.
Oximetry monitoring (SpO2) is an essential part of any surgery but it is especially important in laparoscopic surgery because of the dim lighting in the laparoscopic surgery theater and the wearing of protective glasses if a laser is being used make it difficult to recognize cyanosis. In any case, the latter is a late clinical sign of hypoxia. Variations in saturation are not specific during laparoscopic surgery. Desaturation is a late sign of complications such as gas embolism, pneumothorax, selective intubation, or a shunt effect due to excessively high intraperitoneal pressure.
During laparoscopic surgery, control of intraperitoneal pressure is an integral part of the anesthesia monitoring. The insufflator must be microprocessor controlled; it must be reliable and subjected to regular checks. Excessive intraperitoneal pressure must trigger an alert and an immediate halt in insufflation. As the majority of older insufflators do not have a safety valve for a reduction in intraperitoneal pressure, this must be carried out by manual exsufflation via opening the valve of the cannula.
The monitoring of the neuromuscular block is also important. Proper relaxation is good for laparoscopic surgery. Stable and deep myoresolution improves the laparoscopic surgeon’s view and limits the peritoneal insufflation pressures. In addition, the wide range of operating times and the rapidity with which an operation is terminated means it is essential to know exactly what the neuromuscular block situation is at any point in time. When equipment for reading the muscular activity in the thumb is not available, the simplest stimulation is a train of four on a temporal branch of the facial nerve and observation of the contraction of the orbicular eye muscle.
Intraperitoneal insufflation of dry and unheated gas, possibly accompanied by irrigation with cold liquids results in heat loss during laparoscopic surgery which is at least equal to that with laparotomy. Temperature monitoring associated with measures to combat heat loss is also essential when procedures take several hours. It is important to remember that excessive leakage of gas through the cannula causes rapid hypothermia to the patient.
Cardiovascular Monitoring
Measurement via the bloodstream enables arterial pressure to be monitored in real-time. In addition, the appearance of cyclic variations in time with ventilation is an excellent indication of drops in preloading which prompts the intraperitoneal insufflation pressure to be limited, to increase filling, or even to accentuate the Trendelenburg’s position when possible. Installation of an arterial entry point also helps with blood gas measurements.
Measurement of central venous pressure is traditionally used to supervise the filling pressures in the right heart. This becomes difficult during laparoscopic surgery because of the changes in the position which require continual changes at the cell level, and particularly because of the increase in intrathoracic pressure transmitted from the peritoneal area via the diaphragm. It is important to perform simultaneous measurement of intrathoracic pressure which is obtained by esophageal pressure and to deduct this from the measured central venous pressure.
Catheterization of the right heart using a Swan Ganz probe has been used for monitoring during laparoscopic surgery. As for central venous pressure, the values measured need to be corrected according to the intrathoracic pressure. An increase in pulmonary arterial pressure is an early sign of gas embolism. Aspiration of the gas bubbles by the proximal orifice placed in the right atrium theoretically helps to minimize the consequences of air embolism. The use of a Swan Ganz probe during laparoscopy for patients with the coronary disease helps adapt the anesthesia protocol and therapy, for simple measurement of arterial pressure is insufficient in 80 percent of these cases. Nevertheless, in the course of general anesthesia with controlled ventilation when SaO2, hemoglobin, and oxygen consumption are stable, a change in SvO2 is often the sign of a change in cardiac flow rate.
Because right heart catheterization is an invasive procedure, several studies have reported the use of cardiac flow rate monitoring by electrical bio-impedance during laparoscopic surgery. The principle is founded on continuous measurement of the blood flow rate in the thorax by analysis of the variations in conductivity relative to an electrical field. Transthoracic electrical bio-impedance brings a certain number of advantages:
• Low-risk (non-invasive monitoring)
• Easy and simple to use
• Continuous measurement in real-time
• Not limited in time
• Inexpensive
• Reliability seems to be satisfactory compared to other methods.
It is important that the skin be carefully prepared and the electrodes are of good quality and correctly positioned.
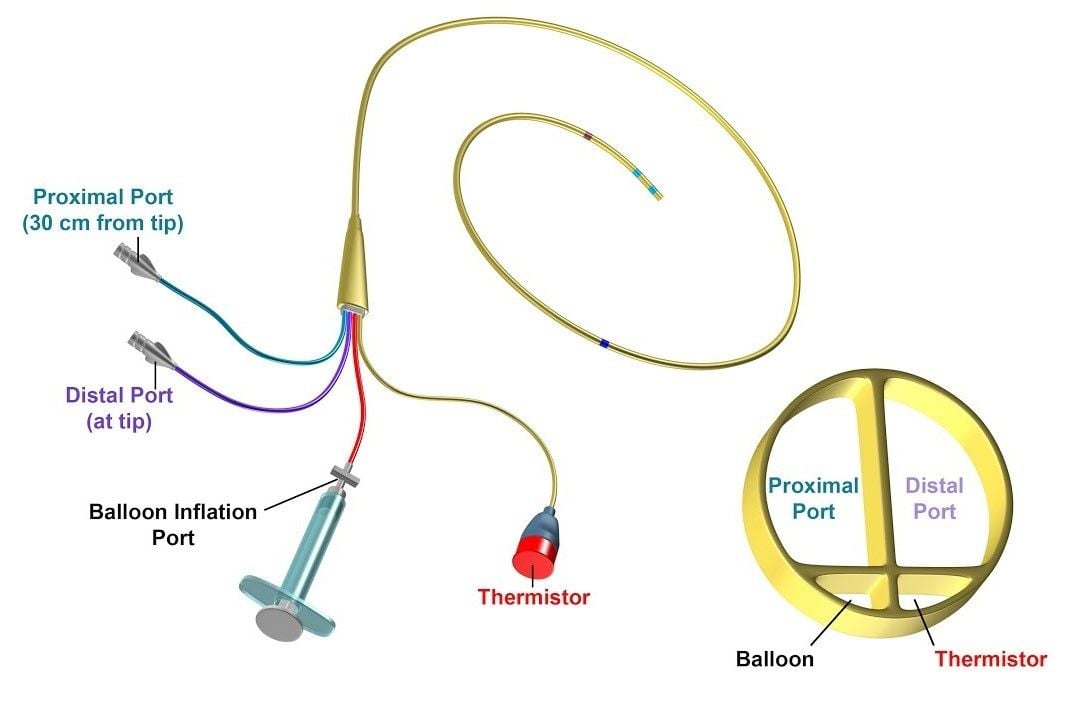
Swan Ganz catheter
However, its use in standard monitoring is still limited due in large part to the frequent difficulties encountered in interpreting the variations. Some studies have been made of hemodynamic monitoring during laparoscopic surgery using transesophageal ultrasound cardiography. Whereas the advantages of this technique for monitoring and diagnosis are considerable, the cost remains an important barrier. Interpretation can also be difficult because of the variations in the viewing axis of the heart according to peritoneal pressure and the variable patient’s position.
Measurement of the cardiac flow rate by pulsed Doppler velocimetry can be carried out by either the transesophageal or the supra-sternum route at the time of laparoscopic surgery. The basic principle is the same as with any Doppler device with a piezoelectric transducer transmitter and a transducer receiver which receives the return echoes modified by the Doppler effect when they bounce off mobile structures like the wall of the heart, vessels or red blood cells. Based on the effective diameter of the aorta which can either be calculated from the cardiac flow rate measured by another method or estimated from the patient's biometric factors, the ejection volume can be deduced and thus the continuous cardiac flow rate.
Respiratory Monitoring
Quantitative waveform capnography is the continuous, noninvasive measurement and graphical display of end-tidal carbon dioxide (ETCO2, also called PetCO2). Capnography uses a sample chamber/sensor placed for optimum evaluation of expired CO2. The inhaled and exhaled carbon dioxide is graphically displayed on a capnograph as a waveform on the monitor along with its corresponding numerical measurement.
As an assessment tool during laparoscopic surgery, capnography can help the anesthetist determine the number of things. It is a direct measurement of ventilation in the lungs, CO2 absorption causing hypercarbia and it also indirectly measures metabolism and circulation. For example, an increase in CO2 absorption during laparoscopy will increase the ETCO2 and a decrease in perfusion will lower the delivery of carbon dioxide to the lungs. This will cause a decrease in the ETCO2 (end-tidal CO2), and this will be observable on the waveform as well as with the numerical measurement. Capnography is a continuous and noninvasive method for carbon dioxide (CO2) measurement, and it has become the standard of care for basic respiratory monitoring for intubated patients during laparoscopic surgery. The CO2 end-tidal pressure (PetCO2) provides evidence of the production of carbon dioxide by cellular metabolism, absorbed through the peritoneal cavity and pulmonary exchanges. A rapid increase in PetCO2 is a serious complication. Thus, Continuous and careful monitoring of EtCO2 by Capnography is a useful and effective noninvasive monitoring technique in anesthesia for laparoscopy. The EtCO2 immediately reflects changes in circulatory status and ventilation as well as detects complications related to CO2 pneumoperitoneum (Hypercarbia, Subcutaneous emphysema, Gas embolism, Pneumothorax, etc.) Thus, EtCO2 monitoring is mandatory and essential monitoring during laparoscopic surgery for the safe conduct of general anesthesia.

Portable CO2 monitor
• A rapid rise of a few millimeters of mercury returning a few minutes later to the base figures may be the sign of minimal CO2 gas embolism.
• A more gradual and persistent rise is often the sign of extraperitoneal diffusion of CO2 (preperitoneal, subcutaneous, retroperitoneal, mediastinal, etc.). This increase in expired CO2 continues after exsufflation of the pneumoperitoneum, indeed often several hours after the laparoscopic procedure, justifying a follow-up of hypercapnia in the recovery room.
• The CO2 is transported by the circulatory system from the peripheral areas towards the lungs. Any disturbance in the circulation will reduce the CO2 expired. A rapid drop in PetCO2 may be the sign of a drop in cardiac flow rate or a decreased venous return, but also pulmonary arterial obliteration. This is what happens in massive gas embolism which shows up as a drop-in PetCO2 proportional in size and duration to the volume of the CO2 embolus.
Classically the PetCO2 values are 2 to 6 mm Hg lower than PaCO2. During anesthesia with artificial ventilation, the ventilation/perfusion ratio of often greater than 1, so a PaCO2-PetCO2 gradient of 10 to 15 mm Hg must be expected. However, during laparoscopic surgery, the change in the arterial CO2-ETCO2 gradient is very variable.
Changes in a position such as the Trendelenburg’s or the lateral reclined position can modify the value of the PetCO2. Furthermore, it is shown that in cases of cardiovascular disease, the correlation between PetCO2 and PaCO2 was less good when compared with patients with no such pathology, and the same is true with obese patients. A recent study confirms that in patients with respiratory impairment; the increases in PaCO2 are underestimated by PetCO2. So for these patients with respiratory or heart pathology, it is particularly useful to duplicate the PetCO2 measurement by arterial gasometry at the beginning of the operation and every time there is an important variation in PetCO2.
In view of this uncertainty, transcutaneous CO 2 monitoring would give a better idea of PaCO2, but this also raises a certain number of technical problems (heating of electrodes, difficulties with measurements in adults, etc.). The anesthetist should keep the following points in mind at the time of laparoscopic surgery:
• The patient voids urine just prior to entering the operating room.
• No shaving is necessary.
• All patients undergoing laparoscopy should have an empty bowel. In the unlikely event of bowel damage, there is much less risk of contamination if the bowel is empty.
• The position of leg is important considering a different laparoscopic procedure. Pressure stocking prevents DVT.
• Good muscle relaxation reduces the intra-abdominal pressure required for the adequate working room in the abdominal cavity.
• The inflation of the stomach should be avoided during artificial ventilation using a mask as this increases the risk of gastric injury during trocar insertion or instrumentation.
• The distended stomach also hampers the visibility of Calot’s triangle at the time of laparoscopic cholecystectomy or laparoscopic bile duct surgery.
• Tracheal intubation and intermittent positive pressure ventilation should be routinely used. This ensures airway protection and controls pulmonary ventilation to avoid hypocarbia.
• The ventilatory pattern should be adjusted according to the respiratory and hemodynamic performance of the individual patient.
• Ventilation with large tidal volumes (12–15 ml/kg) prevents alveolar atelectasis and hypoxemia and allows adequate alveolar ventilation and CO2 elimination.
• Halothane increases the incidence of arrhythmia during
laparoscopic surgery especially in the presence of hypercarbia.
• Isoflurane is the preferred volatile anesthetic agent in minimal access surgery as it has less arrhythmogenic and myocardial depressant effects.
• Patients should receive adequate airway humidification and protection against unintentional hypothermia because generally, the duration of the operation is more in laparoscopic surgery.
• Excessive intravenous sedation should be avoided because it diminishes airway reflexes against pulmonary aspiration in the event of regurgitation.
• Monitoring of PetCO2 is mandatory during laparoscopic surgery. The continuous monitoring of PetCO2 allows adjustment of the minute ventilation to maintain a normal concentration of carbon dioxide and oxygen.
• Airway pressure monitor is mandatory for anesthetized patients receiving intermittent positive pressure ventilation.
Postoperative Considerations
At the end of the procedure, antagonism of the residual muscle relaxation should be reversed by an appropriate dose of neostigmine. When the patient is awake he or she should be extubated and transferred to the recovery room in a semi-recumbent position. Before extubation, the patient’s stomach may be emptied with an orogastric tube. During the next five hours in the postoperative period, analgesia should be achieved. Patients spend a minimum of an hour in the recovery room. Vital signs and O2 saturation are monitored and supplemental O2 is administered by mask or nasal prongs.
Nausea is frequent after general anesthesia. Intravenous droperidol, ondansetron, or metoclopramide can be administered if nausea persists. Vomiting is also common after recovery from anesthesia. Ondem or vomiset, given half an hour before a reversal agent is very helpful in preventing postoperative nausea and vomiting.
The urine output should be at a rate of 100 ml/h and that should continue for 18 hours postoperatively. The nursing management included oxygen therapy, early mobilization, incentive spirometry, and chest physiotherapy. These should repeat at 2 hours interval. She or he should be transferred to the surgical ward and may be discharged home the next day if everything is alright. On the morning of the first postoperative day, the patient should be mobile, pain-free, and should start a soft diet.
It is very common to expect some pain after the procedure. Shoulder pain may occur as a result of distension of the abdomen with gas. As the gas absorbs into the bloodstream and is exhaled through the lungs the pain will gradually disappear, usually over 24 or 48 hours. Depending on the surgery carried out, there may be some interference in bowel function leading to abdominal distension and colicky discomfort. Tramadol hydrochloride is effective for these types of pain. An initial loading dose of these analgesics if administered can give smooth painless recovery.
All procedures under anesthesia carry small but inherent risks and the patient should understand these before agreeing to undergo the procedure. However, the risks of anesthesia for elective surgery under modern conditions are very small indeed.





