Transanal Endoscopic Microsurgery
Transanal endoscopic microsurgery (TEM) was developed by Professor Gerhard Buess from Tuebingen, Germany and it became available for widespread use in 1983. A surgeon's ability to remove rectal lesions transanally is limited by access and exposure, with conventional instruments usually restricting the surgeon to the distal six to seven centimeters of the rectum. When transanal excision is not possible, the traditional transabdominal approach, a major surgical procedure is necessary. Transanal endoscopic microsurgery (TEM), with its longer reach and enhanced visibility of the entire rectum, extends the boundaries of transanal surgery, giving appropriately selected patients a minimally invasive surgical option with a faster and virtually pain-free recovery.
Transanal endoscopic microsurgery (TEM) allows for local excision of rectal neoplasm with greater exposure than transanal excision and less morbidity than transabdominal approaches. Supporters of the TEM technique praise the excellent exposure of the rectum and the minimal invasiveness, as opposed to conventional surgical techniques. The arrival of TEM was associated with an increase in the number of operations for rectal cancer; however, the use of TEM remained constant relative to radical resections. The use of TEM resection alone is appropriate for all adenomas and cancers staged Tis and T1. The use of TEM alone is not an appropriate treatment for T2 cancers.
Local excision of rectal neoplasms is an accepted method of treating selected lesions and can be accomplished through either a transanal approach or a posterior proctotomy. The former is hindered by poor exposure and visibility of lesions in the middle and upper rectum. While the latter approach does give somewhat improved exposure of these more cephalad tumors, it may be complicated by fecal fistulae or sphincter impairment. Transanal endoscopic microsurgery (TEM) has emerged as a better technique for removing lesions in the middle and upper rectum, and it obviates the need for a posterior proctotomy. Furthermore, the transanal rectoscope extends the boundaries of transanal surgery by providing access to lesions previously inaccessible with conventional means. A net result is an operative approach to rectal lesions that is not hindered by the poor exposure and limited reach associated with conventional retractors.
Virtually any adenoma of any size or degree of circumferential involvement can be removed with TEM. Adenomas are removed with a 5 mm margin of normal mucosa, and dissection is undertaken in the submucosal plane. For large adenomas or those that have firm areas within them or previous histological evidence of atypia or dysplasia, the risk of harboring an occult cancer is increased; for such lesions, it is generally recommended that a full-thickness excision be performed. Other benign indications for TEM include transrectal rectopexy for prolapse, for which there has been a limited experience to date, and correction of anastomotic strictures by stricturoplasty.
Indications of Transanal Endoscopic Microsurgery
Benign
• Rectal polyps
• Carcinoid tumors
• Retrorectal masses
• Anastomotic strictures
• Extrasphincteric fistulae
• Pelvic abscesses
Malignant
• Malignant rectal polyps
• T1-T2 rectal cancer
• Palliative excision of T3 cancer
Instruments
The basic TEM instrumentation includes the combined endosurgical unit, which regulates carbon dioxide insufflation, saline irrigation, and suction. The rectoscope is 40 mm in diameter and is available in lengths of 12 and 20 cm. Once the rectoscope is inserted to the desired location within the rectum, it is secured to the operating room table with a double ball-and-socket supporting arm. During the dissection, the supporting arm is moved frequently to maintain direct visibility of the lesion. The end of the rectoscope is sealed with an airtight facepiece that has 5 entry ports. These ports, in turn, are sealed by rubber caps and sleeves so that the various instruments necessary for the dissection can be inserted. One of the big advantages of TEM is binocular vision. The binocular stereoscopic eyepiece is inserted through one of the ports, and it has an accessory scope for video hook-up. The various instruments needed are a suction catheter, a needle-tipped high-frequency electrical knife, tissue graspers that are oriented to either the right or left, scissors, and a needle holder. The suction catheter, tissue graspers, and needle-tipped knife can all be connected to the cautery unit, which greatly facilitates control of hemorrhage and coagulation of bleeding vessels.

The position of the lesion determines the positioning of the patient on the operating room table. The patient should be positioned in such a way that the lesion should be made to be in the 6 O'clock position for the operator.


The position of the patient in the operating room is dependent on tumor location. Since the bevel of the rectoscope must face downward, patients with anterior lesions are placed in the prone position, whereas patients with posterior lesions are placed in the lithotomy position. Patients with lateral lesions are placed accordingly into the appropriate decubitus position.
Transanal Endoscopic Microsurgery Procedures
Properly selected rectal cancers can also be removed with TEM; for such lesions, a 1 cm margin of normal tissue surrounding the lesion should be obtained. A full-thickness excision is mandatory to accurately stage the depth of penetration and unpredictable in its location. Transanal endoscopic microsurgery is a safe technique, and having a low number of complications; however, this procedure is not a license to disregard established criteria for local excision of cancers. The exceptions to this may be tumor size and location. With its superior optics, constant rectal distention, and longer instrument casing, TEM is not limited to small, distally located lesions. Because of the magnification capabilities of the TEM equipment—about 30 times greater than normal—we are better able to visualize the lesion and get very good margins. This minimizes the chances of the patient needing a colostomy, which can sometimes result with open surgery, even with benign lesions. One may argue that cancers within the middle and upper rectum should all be treated with low shrinking tumors, or even inducing a complete remission, TEM may have an increased role. However, this remains to be seen and can only be answered with further studies.


Data presented at the annual meeting of the American Society of Colon and Rectal Surgeons last July also suggests that TEM offers certain advantages over the more standard procedure. In a retrospective study that compared transanal excision with TEM for both benign and malignant rectal masses, the TEM procedure was much more likely to result in a complete resection and yield negative margins compared with transanal excision (88 vs 71%). This was true whether the lesion was benign or malignant. It was also more likely to produce an intact, non-fragmented specimen compared with transanal excision (94 vs 63%), making it easier for pathological evaluation.
The rate of recurrence, both local and distant, was also lower in patients who had undergone TEM compared with transanal excision (5 vs 25%). This was particularly true for rates of local recurrence, which were significantly lower for both benign and malignant lesions following TEM (4 vs 20%). The rate of complications was similar between both groups.
Common Complications
• Perforation of the intraperitoneal rectal wall—unable to close using TEM in 3.9 percent
• Required LAR or diversion (1 patient)
• Early mild incontinence/soiling in 2.6 percent resolved by 10 weeks.
The cost of the TEMS equipment must be mentioned. The capital outlay of more than $50,000 is considerable. However, this is offset by several factors. There is no doubt that some surgeons will argue about how many patients have rectal lesions that are definitely reachable only with the TEMS system. These patients are clearly saved a transabdominal rectal excision and realize a very significant cost saving. In addition, there are no disposable costs per case, and the equipment is robust, requiring minimal maintenance (our own system is now 10 years old). The imaging stack is compatible with the laparoscopic surgical system available in most operating suites. However, in view of the limited number of patients undergoing a TEMS in a tertiary referral center, we believe that this is not a suitable approach for every colorectal unit and suggest that only larger centers would have enough patients to justify the costs. TEM is appropriate for a very specific patient population that includes patients with rectal benign or early cancer with no lymph node involvement. However, in this setting, the benefits are such that this technique has a rightful place as part of the colorectal surgeon's operative armamentarium.
Established TEM
• Laparoscopic cholecystectomy
• Diagnostic laparoscopy
• Laparoscopic appendicectomy
• Laparoscopic Nissen fundoplication
• Laparoscopic (or thoracoscopic) Heller’s myotomy
• Laparoscopic adrenalectomy
• Laparoscopic splenectomy
• Thoracoscopic sympathectomy
• Laparoscopic rectopexy.
Under Evaluation
• Laparoscopic hernia repair
• Laparoscopic colectomy
• Laparoscopic nephrectomy for living related donor transplant
• Parathyroidectomy (guided with hand held gamma probe)
• Laparoscopic repair of duodenal perforation.
Prospects
• Sentinel node biopsy
• Hepatic resection
• Gastrectomy.
The future laparoscopic technology includes three- dimensional, virtual reality, and HDTV. HDTV expands the scanning rate from 525 lines of resolution to 1000 or 1200 lines per frame and the quality of picture would be twice better than existing system.
With virtual reality, a three-dimensional computer image is presented through liquid crystal glasses.
The future of three-dimensional images is not far away and many instrument companies have prototype in the field. Laparoscopic surgery is growing in such a speed that 3D image projection system is going to replace the conventional monitor in near future and surgeon will get a virtual image in air just above the body of patient. This new projection system will abolish all the limitation of current two-dimensional images without depth perception.

Hologram projection system
Over the past 10 years, the major drive in surgery has been the development and application of minimal access approaches to traditional operations. This philosophy has crossed all surgical specialties and has had a major impact on training, technological developments, and patient care.
In general surgery, the emphasis has been on laparoscopic techniques, which can now be applied to the majority of intra-abdominal procedures. Evidence suggests that the reduction in trauma to the abdominal wall and the physiology of the pneumoperitoneum has a positive impact on patients undergoing abdominal operations. Although still not widely applied, these techniques have put surgeons on notice that flexible endoscopy may become an important component of their practice.
Surgeons have gone beyond the luminal confines of the gastrointestinal tract to perform intra-abdominal procedures. With existing flexible endoscopic instrumentation, the wall of the stomach is punctured and an endoscope is advanced into the peritoneal cavity to perform various procedures; thus far, the use of this technique for diagnostic exploration, liver biopsy, cholecystectomy, splenectomy, and tubal ligation has been reported in animal models. Recently transvaginal endoscopic cholecystectomy is performed in France.
Transvaginal cholecystectomy
After the intervention is finished, the scope is pulled back into the stomach and the puncture closed. Several videos have been shown at scientific meetings that suggest that at least transgastric appendectomy has been performed in humans. Other natural orifices, such as the anus or vagina, also allow access to the peritoneal cavity. Although in its infancy, the performance of Natural Orifice Transluminal Endoscopic Surgery (NOTES) may thus further revolutionize the field of abdominal surgery.
Obvious questions are raised by the possibilities of NOTES:
• Is there any clinical advantage to avoiding incisions in the abdominal wall? Can the visceral wall be closed safely and reliably?
• Do the flora of the natural orifice lead more to peritoneal infection?
• Who should perform these procedures, and how should the individuals be trained in NOTES?
Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) and gastroenterologists from the American Society of Gastrointestinal Endoscopists (ASGE) held a summit meeting to build a conceptual framework for the initial safe application of NOTES procedures. It was acknowledged that the development of NOTES further blurred the lines between the traditional boundaries of GI surgeons and endoscopists. Several broad concepts and principles were agreed upon and will soon be published in detail in a white paper.

Introduction of operative endoscope through the vaginal orifice
Safe Application of NOTES
The concepts included the following: Initially, NOTES should be performed by a team of experienced laparoscopic surgeons and interventional endoscopists in an operating room. Clinical procedures should be done under Institutional Review Board supervision and entered into a prospective outcomes database. Basic research is needed to assess the physiologic alterations caused by the visceral puncture and the bacteriology of the peritoneal cavity following transluminal interventions. Collaboration with industry is critical to the development of effective instruments allowing traction/countertraction and stable optical platforms, as well as the means to control hemostasis, securely close the visceral wall, and perform suturing functions and gastrointestinal anastomoses.
The roots of NOTES have been established but work is still needed to refine techniques, verify safety, and document efficacy. With continued research, NOTES may prove to be a sound method with clinical benefit to patients. Appropriate scientific scrutiny, collaboration among gastrointestinal interventionalists, and effective means of training for these techniques will be critical on emerging technologies.
Transanal endoscopic microsurgery (TEM) was developed by Professor Gerhard Buess from Tuebingen, Germany and it became available for widespread use in 1983. A surgeon's ability to remove rectal lesions transanally is limited by access and exposure, with conventional instruments usually restricting the surgeon to the distal six to seven centimeters of the rectum. When transanal excision is not possible, the traditional transabdominal approach, a major surgical procedure is necessary. Transanal endoscopic microsurgery (TEM), with its longer reach and enhanced visibility of the entire rectum, extends the boundaries of transanal surgery, giving appropriately selected patients a minimally invasive surgical option with a faster and virtually pain-free recovery.
Transanal endoscopic microsurgery (TEM) allows for local excision of rectal neoplasm with greater exposure than transanal excision and less morbidity than transabdominal approaches. Supporters of the TEM technique praise the excellent exposure of the rectum and the minimal invasiveness, as opposed to conventional surgical techniques. The arrival of TEM was associated with an increase in the number of operations for rectal cancer; however, the use of TEM remained constant relative to radical resections. The use of TEM resection alone is appropriate for all adenomas and cancers staged Tis and T1. The use of TEM alone is not an appropriate treatment for T2 cancers.
Local excision of rectal neoplasms is an accepted method of treating selected lesions and can be accomplished through either a transanal approach or a posterior proctotomy. The former is hindered by poor exposure and visibility of lesions in the middle and upper rectum. While the latter approach does give somewhat improved exposure of these more cephalad tumors, it may be complicated by fecal fistulae or sphincter impairment. Transanal endoscopic microsurgery (TEM) has emerged as a better technique for removing lesions in the middle and upper rectum, and it obviates the need for a posterior proctotomy. Furthermore, the transanal rectoscope extends the boundaries of transanal surgery by providing access to lesions previously inaccessible with conventional means. A net result is an operative approach to rectal lesions that is not hindered by the poor exposure and limited reach associated with conventional retractors.
Virtually any adenoma of any size or degree of circumferential involvement can be removed with TEM. Adenomas are removed with a 5 mm margin of normal mucosa, and dissection is undertaken in the submucosal plane. For large adenomas or those that have firm areas within them or previous histological evidence of atypia or dysplasia, the risk of harboring an occult cancer is increased; for such lesions, it is generally recommended that a full-thickness excision be performed. Other benign indications for TEM include transrectal rectopexy for prolapse, for which there has been a limited experience to date, and correction of anastomotic strictures by stricturoplasty.
Indications of Transanal Endoscopic Microsurgery
Benign
• Rectal polyps
• Carcinoid tumors
• Retrorectal masses
• Anastomotic strictures
• Extrasphincteric fistulae
• Pelvic abscesses
Malignant
• Malignant rectal polyps
• T1-T2 rectal cancer
• Palliative excision of T3 cancer
Instruments
The basic TEM instrumentation includes the combined endosurgical unit, which regulates carbon dioxide insufflation, saline irrigation, and suction. The rectoscope is 40 mm in diameter and is available in lengths of 12 and 20 cm. Once the rectoscope is inserted to the desired location within the rectum, it is secured to the operating room table with a double ball-and-socket supporting arm. During the dissection, the supporting arm is moved frequently to maintain direct visibility of the lesion. The end of the rectoscope is sealed with an airtight facepiece that has 5 entry ports. These ports, in turn, are sealed by rubber caps and sleeves so that the various instruments necessary for the dissection can be inserted. One of the big advantages of TEM is binocular vision. The binocular stereoscopic eyepiece is inserted through one of the ports, and it has an accessory scope for video hook-up. The various instruments needed are a suction catheter, a needle-tipped high-frequency electrical knife, tissue graspers that are oriented to either the right or left, scissors, and a needle holder. The suction catheter, tissue graspers, and needle-tipped knife can all be connected to the cautery unit, which greatly facilitates control of hemorrhage and coagulation of bleeding vessels.

40 mm proctoscope
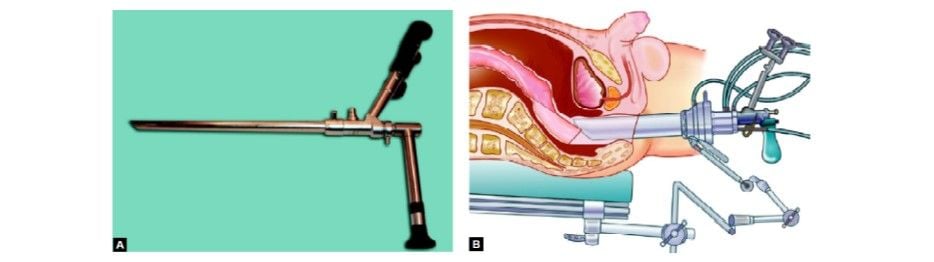
Stereoscope used in TEM

Fine curve tipped instruments for TEM

Needle holders and electrosurgical instruments used in TEM
Patient Positioning in Transanal Endoscopic Microsurgery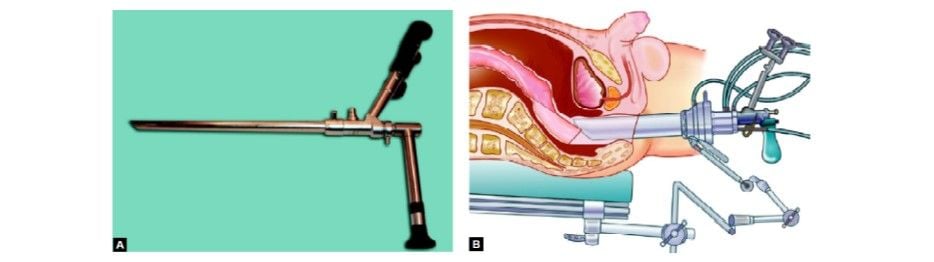
Stereoscope used in TEM

Fine curve tipped instruments for TEM

Needle holders and electrosurgical instruments used in TEM
The position of the lesion determines the positioning of the patient on the operating room table. The patient should be positioned in such a way that the lesion should be made to be in the 6 O'clock position for the operator.

The positioning of the patient for TEM

Patient position for a lesion at a right lateral position
The position of the patient in the operating room is dependent on tumor location. Since the bevel of the rectoscope must face downward, patients with anterior lesions are placed in the prone position, whereas patients with posterior lesions are placed in the lithotomy position. Patients with lateral lesions are placed accordingly into the appropriate decubitus position.
Transanal Endoscopic Microsurgery Procedures
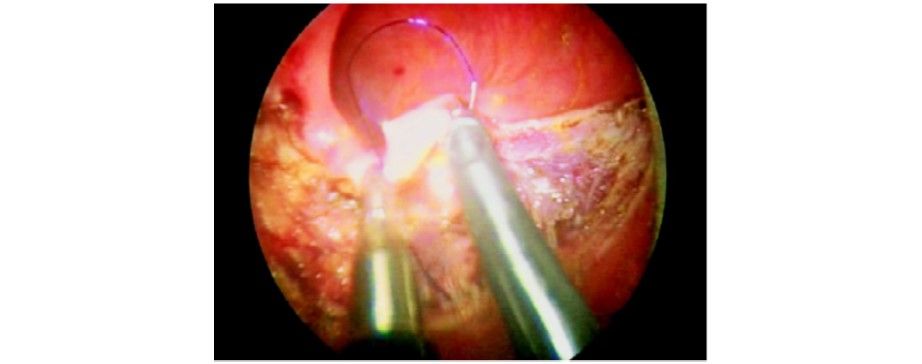
Properly selected rectal cancers can also be removed with TEM; for such lesions, a 1 cm margin of normal tissue surrounding the lesion should be obtained. A full-thickness excision is mandatory to accurately stage the depth of penetration and unpredictable in its location. Transanal endoscopic microsurgery is a safe technique, and having a low number of complications; however, this procedure is not a license to disregard established criteria for local excision of cancers. The exceptions to this may be tumor size and location. With its superior optics, constant rectal distention, and longer instrument casing, TEM is not limited to small, distally located lesions. Because of the magnification capabilities of the TEM equipment—about 30 times greater than normal—we are better able to visualize the lesion and get very good margins. This minimizes the chances of the patient needing a colostomy, which can sometimes result with open surgery, even with benign lesions. One may argue that cancers within the middle and upper rectum should all be treated with low shrinking tumors, or even inducing a complete remission, TEM may have an increased role. However, this remains to be seen and can only be answered with further studies.

Setting us instruments in TEM to start the procedure

Resected tissue through TEM
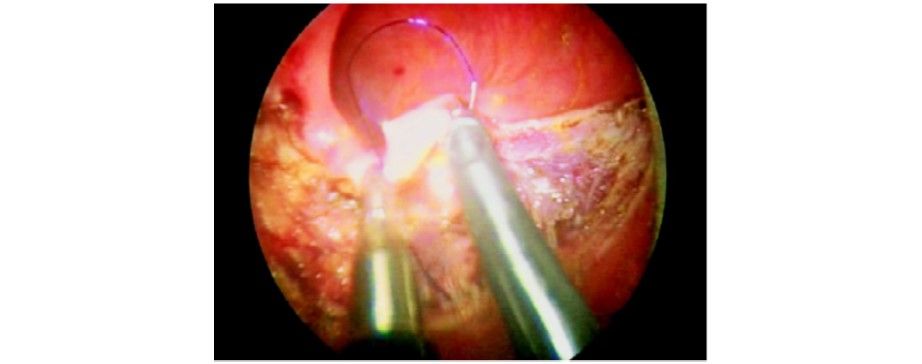
Suturing in TEM
Data presented at the annual meeting of the American Society of Colon and Rectal Surgeons last July also suggests that TEM offers certain advantages over the more standard procedure. In a retrospective study that compared transanal excision with TEM for both benign and malignant rectal masses, the TEM procedure was much more likely to result in a complete resection and yield negative margins compared with transanal excision (88 vs 71%). This was true whether the lesion was benign or malignant. It was also more likely to produce an intact, non-fragmented specimen compared with transanal excision (94 vs 63%), making it easier for pathological evaluation.
The rate of recurrence, both local and distant, was also lower in patients who had undergone TEM compared with transanal excision (5 vs 25%). This was particularly true for rates of local recurrence, which were significantly lower for both benign and malignant lesions following TEM (4 vs 20%). The rate of complications was similar between both groups.
Common Complications
• Perforation of the intraperitoneal rectal wall—unable to close using TEM in 3.9 percent
• Required LAR or diversion (1 patient)
• Early mild incontinence/soiling in 2.6 percent resolved by 10 weeks.
The cost of the TEMS equipment must be mentioned. The capital outlay of more than $50,000 is considerable. However, this is offset by several factors. There is no doubt that some surgeons will argue about how many patients have rectal lesions that are definitely reachable only with the TEMS system. These patients are clearly saved a transabdominal rectal excision and realize a very significant cost saving. In addition, there are no disposable costs per case, and the equipment is robust, requiring minimal maintenance (our own system is now 10 years old). The imaging stack is compatible with the laparoscopic surgical system available in most operating suites. However, in view of the limited number of patients undergoing a TEMS in a tertiary referral center, we believe that this is not a suitable approach for every colorectal unit and suggest that only larger centers would have enough patients to justify the costs. TEM is appropriate for a very specific patient population that includes patients with rectal benign or early cancer with no lymph node involvement. However, in this setting, the benefits are such that this technique has a rightful place as part of the colorectal surgeon's operative armamentarium.
Established TEM
• Laparoscopic cholecystectomy
• Diagnostic laparoscopy
• Laparoscopic appendicectomy
• Laparoscopic Nissen fundoplication
• Laparoscopic (or thoracoscopic) Heller’s myotomy
• Laparoscopic adrenalectomy
• Laparoscopic splenectomy
• Thoracoscopic sympathectomy
• Laparoscopic rectopexy.
Under Evaluation
• Laparoscopic hernia repair
• Laparoscopic colectomy
• Laparoscopic nephrectomy for living related donor transplant
• Parathyroidectomy (guided with hand held gamma probe)
• Laparoscopic repair of duodenal perforation.
Prospects
• Sentinel node biopsy
• Hepatic resection
• Gastrectomy.
The future laparoscopic technology includes three- dimensional, virtual reality, and HDTV. HDTV expands the scanning rate from 525 lines of resolution to 1000 or 1200 lines per frame and the quality of picture would be twice better than existing system.
With virtual reality, a three-dimensional computer image is presented through liquid crystal glasses.
The future of three-dimensional images is not far away and many instrument companies have prototype in the field. Laparoscopic surgery is growing in such a speed that 3D image projection system is going to replace the conventional monitor in near future and surgeon will get a virtual image in air just above the body of patient. This new projection system will abolish all the limitation of current two-dimensional images without depth perception.

Hologram projection system
Over the past 10 years, the major drive in surgery has been the development and application of minimal access approaches to traditional operations. This philosophy has crossed all surgical specialties and has had a major impact on training, technological developments, and patient care.
In general surgery, the emphasis has been on laparoscopic techniques, which can now be applied to the majority of intra-abdominal procedures. Evidence suggests that the reduction in trauma to the abdominal wall and the physiology of the pneumoperitoneum has a positive impact on patients undergoing abdominal operations. Although still not widely applied, these techniques have put surgeons on notice that flexible endoscopy may become an important component of their practice.
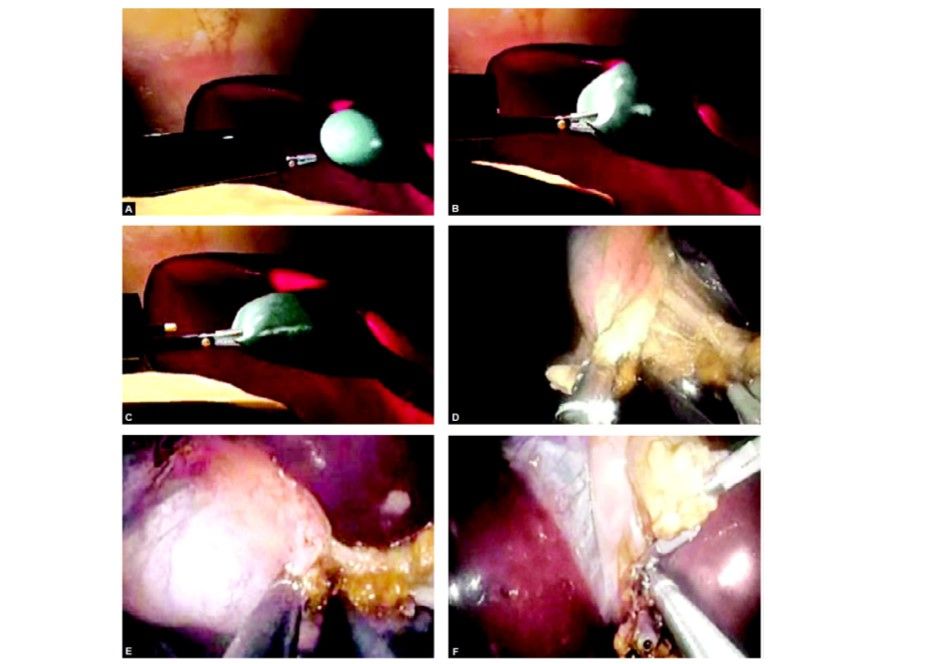
Surgeons have gone beyond the luminal confines of the gastrointestinal tract to perform intra-abdominal procedures. With existing flexible endoscopic instrumentation, the wall of the stomach is punctured and an endoscope is advanced into the peritoneal cavity to perform various procedures; thus far, the use of this technique for diagnostic exploration, liver biopsy, cholecystectomy, splenectomy, and tubal ligation has been reported in animal models. Recently transvaginal endoscopic cholecystectomy is performed in France.
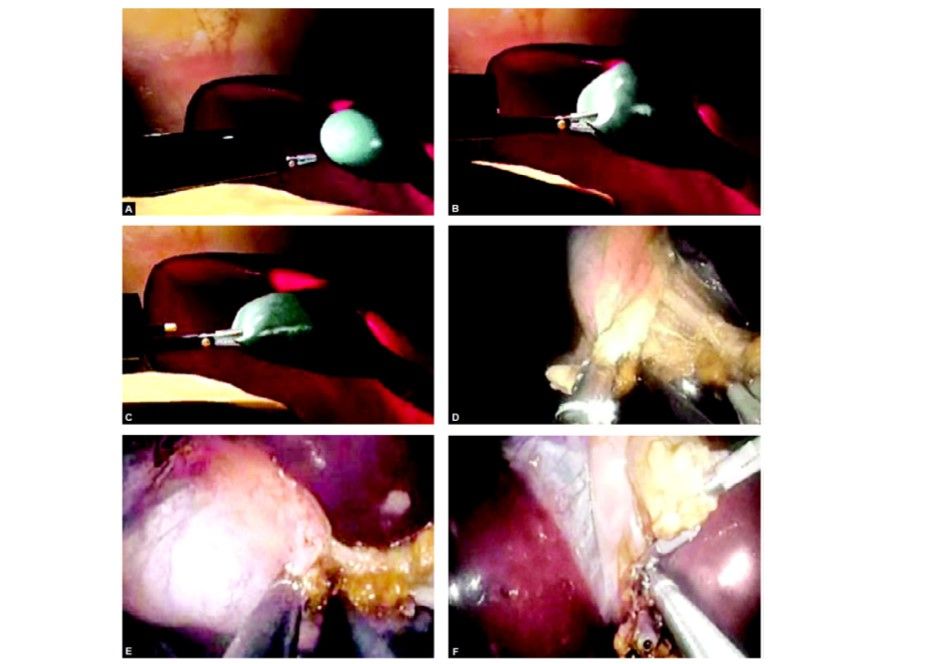
Transvaginal cholecystectomy
After the intervention is finished, the scope is pulled back into the stomach and the puncture closed. Several videos have been shown at scientific meetings that suggest that at least transgastric appendectomy has been performed in humans. Other natural orifices, such as the anus or vagina, also allow access to the peritoneal cavity. Although in its infancy, the performance of Natural Orifice Transluminal Endoscopic Surgery (NOTES) may thus further revolutionize the field of abdominal surgery.
Obvious questions are raised by the possibilities of NOTES:
• Is there any clinical advantage to avoiding incisions in the abdominal wall? Can the visceral wall be closed safely and reliably?
• Do the flora of the natural orifice lead more to peritoneal infection?
• Who should perform these procedures, and how should the individuals be trained in NOTES?
Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) and gastroenterologists from the American Society of Gastrointestinal Endoscopists (ASGE) held a summit meeting to build a conceptual framework for the initial safe application of NOTES procedures. It was acknowledged that the development of NOTES further blurred the lines between the traditional boundaries of GI surgeons and endoscopists. Several broad concepts and principles were agreed upon and will soon be published in detail in a white paper.

Introduction of operative endoscope through the vaginal orifice
Safe Application of NOTES
The concepts included the following: Initially, NOTES should be performed by a team of experienced laparoscopic surgeons and interventional endoscopists in an operating room. Clinical procedures should be done under Institutional Review Board supervision and entered into a prospective outcomes database. Basic research is needed to assess the physiologic alterations caused by the visceral puncture and the bacteriology of the peritoneal cavity following transluminal interventions. Collaboration with industry is critical to the development of effective instruments allowing traction/countertraction and stable optical platforms, as well as the means to control hemostasis, securely close the visceral wall, and perform suturing functions and gastrointestinal anastomoses.
The roots of NOTES have been established but work is still needed to refine techniques, verify safety, and document efficacy. With continued research, NOTES may prove to be a sound method with clinical benefit to patients. Appropriate scientific scrutiny, collaboration among gastrointestinal interventionalists, and effective means of training for these techniques will be critical on emerging technologies.


