DR VISHWANATH MOGALI MBBS, DNB (Gen.Surg), F.MAS, D.MAS
General and advanced laparoscopic surgeon
Saveetha medical college and hospital Chennai, India
This task analysis is submitted as a part of fulfillment of rules and regulations of world laparoscopy hospital for the award of Fellowship and diploma in minimal access surgery - December 2016 batch
TASK ANALYSIS OF SILS CHOLECYSTECTOMY
INTRODUCTION
Cholecystectomy is the most common major abdominal procedure performed now a day. Management of gall stone disease has progressed through eras of nonsurgical management, laparotomy, mini-laparotomy and now laparoscopic cholecystectomy which is the gold standard treatment for benign diseases of gall bladder.
Laparoscopic surgery is the procedure of choice for most benign gall bladder diseases unless contraindicated. The advantages like earlier return of bowel function, less postoperative pain, good cosmesis, shorter length of hospital stay, earlier return to full activity were appreciated.
As the technology and instruments improved, surgeons modified the procedure from traditional four ports laparoscopy to three ports and then to two ports.
As surgeons and industry continue to push the boundaries of laparoscopic or minimally invasive surgery(MIS), new and controversial approaches such as natural orifice trans-luminal endoscopic surgery (NOTES) and single-incision laparoscopic surgery(SILS) are being explored with the goal of reducing surgical morbidity.
Various natural orifices like mouth (trans-gastric), umbilicus and vagina are being used as portals for surgery. Termed variously as Single Port Access(SPA) surgery, Single Incision Laparoscopic Surgery (SILS) or OnePort Umbilical Surgery (OPUS) or Single Port Incision Less Conventional Equipment Utilizing Surgery (SPICES) or Natural Orifice Trans-umbilical Surgery (NOTUS).
SILS is a novel technique which promises all advantages of minimally invasive surgery with additional benefits like reduced postoperative morbidity, improved cosmesis and patients acceptance.
INDICATIONS:
1. Symptomatic gallstones causing repeated episodes of biliary colic.
2. Mucocele of gallbladder, biliary pancreatitis after ERCP and CBD stone extraction.
3. Cholecystitis - acute calculus/acalculus cholecystitis, chronic cholecystitis.
4. Gall bladder polyp size more than 1cm is also an indication for cholecystectomy.
5. In asymptomatic cholelithiasis indications include diabetics, patients undergoing bariatric surgery, renal transplantation, and those with hemolytic diseases.
CONTRAINDICATIONS:
1. Patients who are not fit for general anesthesia.
2. Significant portal hypertension, uncorrectable coagulopathy.
3. Patients with proven or suspected carcinoma of gallbladder.
4. Relative contraindications include complications of cholecystitis like empyma, gangrenous gall bladder and perforation of gallbladder, morbid obesity, pregnancy and cirrhosis of liver.
TASK ANALYSIS SILS CHOLECYSTECTOMY
1. Preparation and anesthesia
2. Procedural steps
3. Executional steps
1. Preparation and anaesthesia:General anaesthesia with Ryle’s tube for decompression of stomach, Bladder catheterization using 14 or 16 Fr Folay’s catheter.
2. Procedural steps:
I. French position of the patient, painting with betadine and draping.
II. Arrangement of optical instruments and energy sources and instrument tray.
III. Creation of pneumoperitoneum and insertion of SILS port and trocars.
IV. Retraction of fundus and dissection of calots triangle to expose cystic artery and cystic duct.
V. Clipping and division of cystic artery and cystic duct.
VI. Dissection of GB from liver and hemostasis.
VII. Specimen retrival along with removal of trocars and SILS port.
VIII. Closure of fascial layer followed by skin.
3. Executional steps:
SINGLE INCISION LAPAROSCOPIC HOLECYSTECTOMY:
Since SILS procedure is relatively new and in evolution, many techniques happen to be described but no widely accepted standard exists. As the primary benefit of SILS seems to be cosmetic, most agree that the umbilicus may be the preferred incision site.
I. Patient Positioning: Patient can be put within supine, split leg lithotomy, or French position. Most prefer the French position in which the patient’s legs split with slight reverse-Trendelenburg position. Surgeon stands between the patient’s legs and assistant surgeon stands either left or right of the surgeon to hold camera, and second assistant who stands either left or right of the patient. The scrub nurse usually stands on left side of the patient. The camera monitor is placed usually at head end or at right shoulder as in standard laparoscopic cholecystectomy. The light source and insufflator are placed similar to the laparoscopic cholecystectomy positioning.

Figure 1. Position of patient and operation room set up in SILS cholecystectomy.
S-Surgeon stands between patients leg, A-Assistant stands to hold camera.
II. Instruments and Devices: All the instruments and devices mentioned above for laparoscopic cholecystectomy are required along with SILS port and 5mm Apple trocars or trocars with small head. Unlike standard laparoscopy, all the trocars, usually 3 to 4, are crowded into one skin incision. To allow the greater freedom of movement and reduced clashing, a few modified trocars with smaller heads, lower profile and absence of insufflation ports such as Apple trocar (Apple Medical Corporation, Marlborough, Massachusetts) and Ternamian EndoTIPTM (Karl Storz Endoscopy, Tuttlingen, Germany). This allows freedom from the hands while maximizing technique incision. Some surgeons use instruments directly through with no trocars. Purpose-designed ports include multilumen, single-trocar system, such as the R-port (Advanced Surgical Concepts, Wicklow, Ireland), Uni-X single laparoscopic port system, and GelPort (Alexis). Recently, Covidien received FDA clearance to promote its SILS multiple instrument access port.
Flexible or roticulating or articulating instruments are preferable for SILS such as grasper, forceps and clip applicator. Most of surgeons use 10mm clip applicator however 5mm clip applicator if available should be used. The camera scope in SILS cholecystectomy can be 10mm or 5mm with 30 or 45 degree angulation.

Figure 2.SILS kit with port, trocars and roticulating instruments.
III. Incision and port placement: It is advisable to do a formal diagnostic laparoscopy using 10mm vertical incision before the actual SILS incision for the beginners. If the anatomy is clear and less adhesions the umbilical skin incision can be increased to 2cm and fascia, sheath and peritoneum should be divided. Incision can vertical in the umbilicus or ohm (Ω) shape over superior crease of the umbilicus. Then the SILS port should be introduced through the umbilical incision (fig 4) and the gas tube should be connected to create pneumoperitoneum.
IV. Pneumoperitoneum is similar to the laparoscopic cholecystectomy procedure except for, pneumo port in SILS port is separate small tube which connects gas tube outside and enter through the SILS port and opens into abdominal cavity side of SILS port. Once the SILS port is introduced through the umbilical incision the pneumo port should be connected to gas tube and pressures are maintained as in any laparoscopic procedures. Some surgeons use gas evacuator tube which sucks out gas when fumes are build up inside the abdominal cavity due to use of cautery or Harmonic scalpel.
V. SILS port which contains 3 small holes for trocar placement, one 10mm trocar inserted through lower hole, which is used for camera scope. Another 5mm or 10mm trocar is inserted through the upper right hole in SILS port and finally the upper left hole is used for 5mm trocar insertion. Three 5mm trocars (Apple trocars) can be used if 5mm camera scope and 5mm clip applicator are available or only one 10mm or 12mm trocar for camera scope and remaining two 5mm trocars can be used.

Figure 3.Various SILS ports.a. Covidien SILS port, b. Quad port, c.Triport 15 and d.GelPoint.
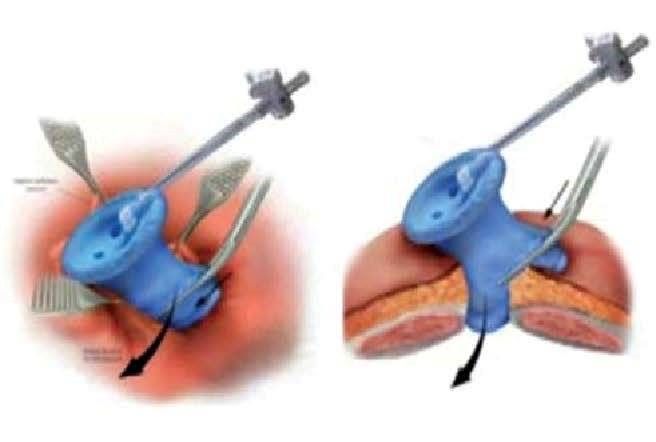
Figure 4.Virtual Picture showing SILS port placement.
VI. Instruments: Once the SILS port is introduced, trocars are placed, and pneumoperitoneum created, the 5mm or 10mm diameter, 30 degree laparoscope inserted through the camera port. Endo Eye coaxial camera(fig 6) can be used to avoid collision of light cable with instruments. The 5mm roticulating grasper is introduced through the upper left trocar and held in surgeon’s left hand. Through the upper right trocar the hook with cautery or Harmonic scalpel™or Maryland dissecting forceps can be used. The 5mm diameter suction cannula, 5mm or 10mm clip applicator, laparoscopic curved scissor, toothed grasper or claw forceps should be kept ready.

Figure 5. Endo EYE with coaxial light cable.
VII. Gallbladder fundus retraction:This is an important step in SILS cholecystectomy which is not usually done in standard laparoscopic cholecystectomy. The fundus retraction in SILS cholecystectomy can be done using 2-0 ProleneTM (Polypropylene Suture; Ethicon, Johnson & Johnson Intl, Sint-Stevens-Woluwe, Belgium) suture on straight needle which is passed through the abdominal wall under vision at the right mid-clavicular line about two finger breadth above the right costal margin and then passed through the fundus of the gallbladder and back again through the abdominal wall and tied on the outside of the abdominal wall. Gallbladder can be retracted using two sutures, one at fundus and another at Hartmann’s pouch. The fundus retraction can also be done using Veress needle inserted through the sub-xiphoid 2mm incision.
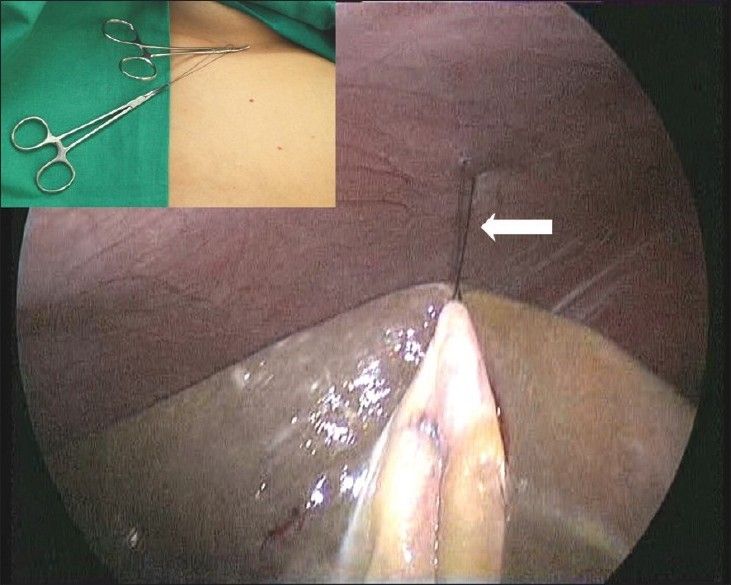
Figure 6.Laparoscopic view of GB fundus traction with external view of suture clip.
VIII. Procedure: After fundus of gallbladder retracted with suture, the remaining steps are similar to the standard laparoscopic cholecystectomy but difference is that the left hand instrument is used to dissect gallbladder while right hand instrument for retraction of Hartman’s pouch. The Hartman’s pouch held with the roticulating grasper and the dissection of triangle of Calot is done using Maryland forceps or hook with cautery or Harmonic scalpel. The posterior peritoneum is divided tofree the Hartman’s pouch. This is followed by further dissection of the anterior and posterior peritoneal leaves overlying the Calot’s triangle. The cystic artery and cystic duct are skeletonized similar to standard laparoscopic cholecystectomy and end point of this dissection is obtaining a “critical view” showing the window between the cystic duct and artery, and between the cystic artery and the liver. These two windows in the Calot’s triangle are dissected well so as to safely observe the tip of the instrument controlling artery and the duct. Then the cystic artery clipped with two medium sized clips using 5mm or 10mm reusable clip applicator and artery is divided using either scissor or Harmonic scalpel. After dividing the artery, the cystic duct clipped with two medium or large sized clips slightly away from cystic to common bile duct junction and one clip on duct close to the gallbladder. Then the cystic duct is divided using curved scissor.

Figure 7.Dissection of Calot’s triangle in SILS.
Once both cystic artery and cystic duct divided safely, the dissection of the gallbladder using hook with cautery or Harmonic scalpel is done by alternating medial and lateral rotation of infundibulum held with roticulating grasper. The gallbladder is separated from the liver and suture applied to retract the fundus is divided. Fundus retraction released by cutting the suture. The gallbladder placed in a sterile plastic bag and kept over the liver waiting for extraction. At this stage the gallbladder fossa is inspected for any bile leak or bleeding, also the cystic duct remnant and cystic artery stump are inspected for bile leak or bleeding. When in doubt a thorough saline wash can be given to gallbladder fossa, and fluid suctioned out meticulously. Any inadvertent spillage of stones are grabbed and placed in the plastic bag containing gallbladder. Once the good hemostasis is ensured, the plastic bag containing gallbladder is removed along with all the instruments and SILS port through the umbilicus.
IX. Closure of the incision: Careful closure of the umbilical incision is mandatory to prevent formation of port site incisional hernia. The edges of the fascial incision are identified, grasped and elevated with Allis forceps or Kocher’s forceps. A non-absorbable suture material like no 1 or 1-0 Prolene or Ethilon can be used for closure of fascial layer in continuous manner or two to three Figure -of-eight manner. After closing the fascia, local anaesthetic infiltration to fascia and skin can be done. The skin is closed with absorbable monofilament suture material by running subcuticular fashion.
Complications of SILS Cholecystectomy:
I. Hemorrage due to injury to cystic artery
II. Bile leak due to CBD or CHD injury.
III. Infection of surgical site.
IV. Incisional hernia.
Difficulties in SILS Cholecystectomy:
Although SILS has many similarities with conventional laparoscopic techniques, there are also a number of differences. Initially, accessing the target organ with multiple instruments and telescope through a single site creates a lot of ergonomic issues like,
I. Triangulation of conventional instruments is difficult
II. As a result clashing or swording of instruments occurs
III. It is difficult to manipulate the instruments as two hands of the surgeon and camera hand of assistant are placed close proximally each other in the SILS port.
To overcome these difficulties, specialized instruments such as Roticulating instruments,endo EYE coaxial telescopes are required and the learning curve to use this technology is higher and it also implies higher technical and financial burden to the person concerned.
ADVANTAGES:
I. Good cosmosis as the umbilicus can completely hide the scar.
II. Early recovery, reduced post operative pain and quality of life which is almost similar to laparoscopic cholecystectomy.
III. Patient’s acceptance is good compared to NOTES and Conventional laparoscopic cholecystectomy.
IV. Specimen retrival is easy through the port.
V. Comined procedures can performed eg; cholecystectomy with appendicectomy or cholecystectomy with hysterectomy.
VI. Surgeon’s domain compared to NOTES which is also performed by physicians.
DISADVANTAGES:
I. Bad ergonomics as base ball-diamond concept not applicable.
II. Difficult with conventional lap instruments, hence need for specialized instruments.
III. Increased cost due use of specialized instruments.
IV. Long learning curve with more stress on surgeons.
V. Increased incidence of surgical site infection and incisional hernia.
| Older Post | Home | Newer Post |
How to Perform and Implement Task Analysis of Laparoscopic and Robotic Procedures
Task analysis is a critical component of any complex surgical procedure, including laparoscopic and robotic surgeries. It involves breaking down the procedure into its constituent tasks, identifying the steps, skills, and cognitive processes required. Task analysis not only enhances the understanding of these intricate surgeries but also serves as a foundation for training, skill assessment, and continuous improvement in healthcare. In this essay, we will delve into how to conduct and implement task analysis for laparoscopic and robotic procedures.
Understanding the Significance of Task Analysis
Before we explore the procedure for task analysis, it's essential to recognize why it is of paramount importance in the realm of surgery, particularly for laparoscopic and robotic procedures.
1. Enhanced Learning and Training: Task analysis helps in developing structured training programs. It breaks down complex procedures into manageable components, making it easier for trainees to learn and practice each step methodically.
2. Skill Assessment: By understanding the tasks and sub-tasks involved, it becomes possible to assess the competence of surgeons and surgical teams. This is crucial for ensuring patient safety and quality care.
3. Workflow Optimization: Task analysis can reveal inefficiencies in surgical workflows. Identifying these bottlenecks allows for process improvements, potentially reducing surgical times and enhancing outcomes.
4. Error Reduction: Recognizing potential points of error is vital for preventing surgical complications. Task analysis can highlight critical steps where errors are more likely to occur, leading to proactive measures to mitigate risks.
Procedure for Task Analysis of Laparoscopic and Robotic Procedures:
Task analysis for laparoscopic and robotic procedures involves several steps:
Step 1: Define the Surgical Procedure
Begin by clearly defining the surgical procedure you wish to analyze. Whether it's a laparoscopic cholecystectomy or a robotic prostatectomy, having a specific procedure in mind is essential.
Step 2: Gather Expert Input
Engage experts in the field, including experienced surgeons, nurses, and other surgical team members. Their input is invaluable in identifying and detailing the tasks involved.
Step 3: Identify the Tasks and Sub-Tasks
Break down the surgical procedure into tasks and sub-tasks. For instance, in a laparoscopic cholecystectomy, tasks could include trocar placement, camera insertion, gallbladder dissection, and suturing. Sub-tasks under "trocar placement" might involve choosing trocar sizes, making incisions, and inserting trocars.
Step 4: Sequence the Tasks
Establish the chronological order of tasks. Determine which tasks are dependent on others and identify any parallel processes. Sequencing tasks is essential for understanding the flow of the procedure.
Step 5: Define Task Goals and Objectives
For each task and sub-task, define the goals and objectives. What should be achieved in each step? For instance, in gallbladder dissection, the goal might be to safely detach the gallbladder from the liver while preserving nearby structures.
Step 6: Skill and Equipment Requirements
Specify the skills and equipment required for each task. Consider the level of expertise needed, such as basic laparoscopic skills or advanced robotic manipulation. Document the instruments and technology involved.
Step 7: Cognitive Processes
Identify the cognitive processes involved, such as decision-making, spatial orientation, and problem-solving. Understanding the mental aspects of surgery is critical for training and error prevention.
Step 8: Consider Variations and Complications
Acknowledge potential variations in the procedure and anticipate complications. How would the surgical team adapt if unexpected issues arise? Task analysis should encompass both the standard procedure and potential deviations.
Step 9: Develop Training and Assessment Tools
Use the task analysis results to create structured training modules. These modules should align with the identified tasks, objectives, and skill requirements. Additionally, design assessment tools to evaluate the competence of trainees and surgical teams.
Step 10: Continuous Improvement
Task analysis is not a one-time endeavor. Regularly revisit the analysis to incorporate new techniques, technology, and best practices. Continuous improvement is vital for staying at the forefront of surgical care.
Implementing Task Analysis Results:
Once task analysis is complete, it's crucial to implement the findings effectively:
1. Training Programs: Develop and deliver training programs based on the task analysis. These programs should encompass both simulation-based training and real-life surgical experience.
2. Skill Assessment: Use the assessment tools developed during task analysis to evaluate the skills of surgical teams. This can be done through structured evaluations and objective metrics.
3. Quality Improvement: Task analysis can reveal areas for process improvement. Work with the surgical team to implement changes that enhance efficiency and patient outcomes.
4. Error Prevention: Utilize the identified points of error to develop strategies for error prevention. This might involve checklists, preoperative briefings, and enhanced communication protocols.
5. Research and Innovation: Task analysis can also guide research efforts, leading to the development of new techniques and technologies that improve surgical procedures.
In conclusion, task analysis is an indispensable tool in understanding, teaching, and advancing complex surgical procedures such as laparoscopic and robotic surgeries. By meticulously dissecting each task and sub-task, identifying skill requirements, and considering cognitive processes, healthcare professionals can enhance patient safety, optimize surgical workflows, and continually improve the quality of surgical care. Task analysis is not merely an analytical exercise; it is a pathway to excellence in surgical practice.




Thanks DR VISHWANATH MOGALI