Surgical Technique of Sleeve Gastrectomy
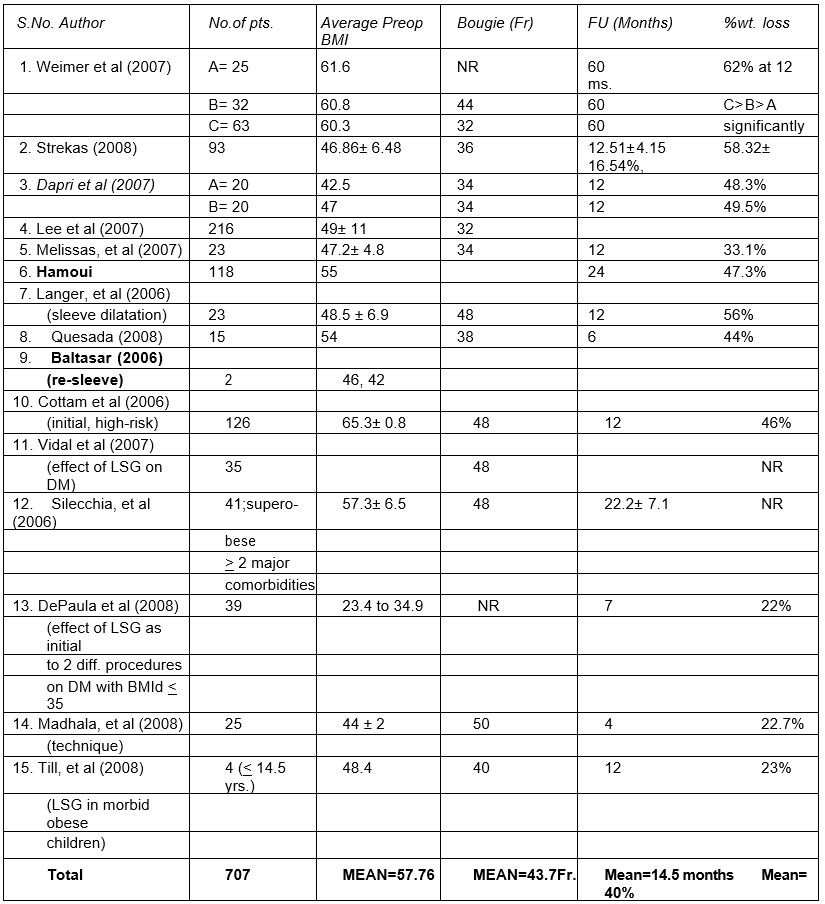
The patient is positioned in a modified reverse Trendelenburg position with the right arm away from the body. The abdomen is prepared and draped in the customary fashion. Ports are used according to the baseball diamond concept as shown in the image below.
Port position for laparoscopic sleeve gastrectomy
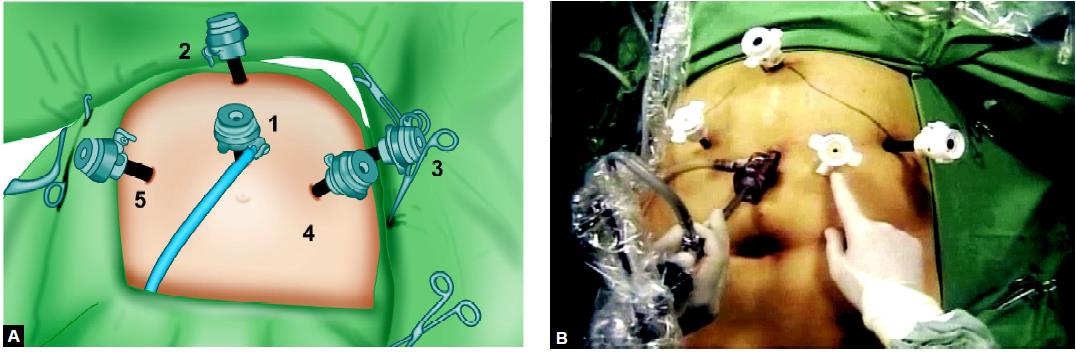
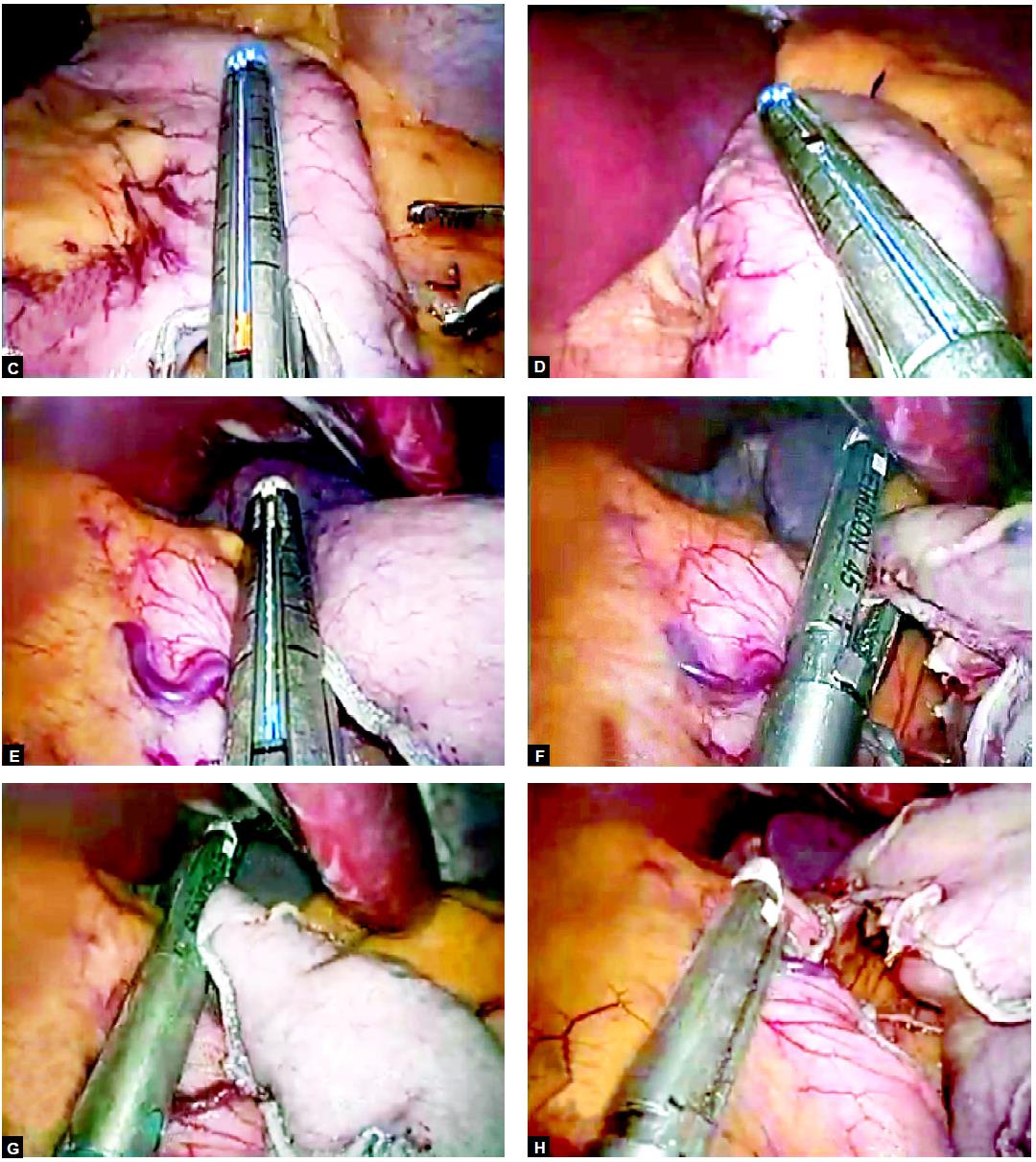
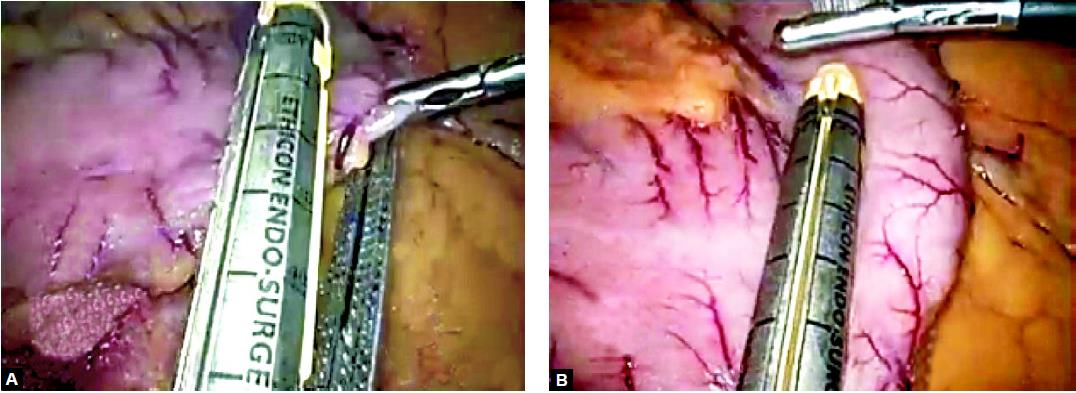
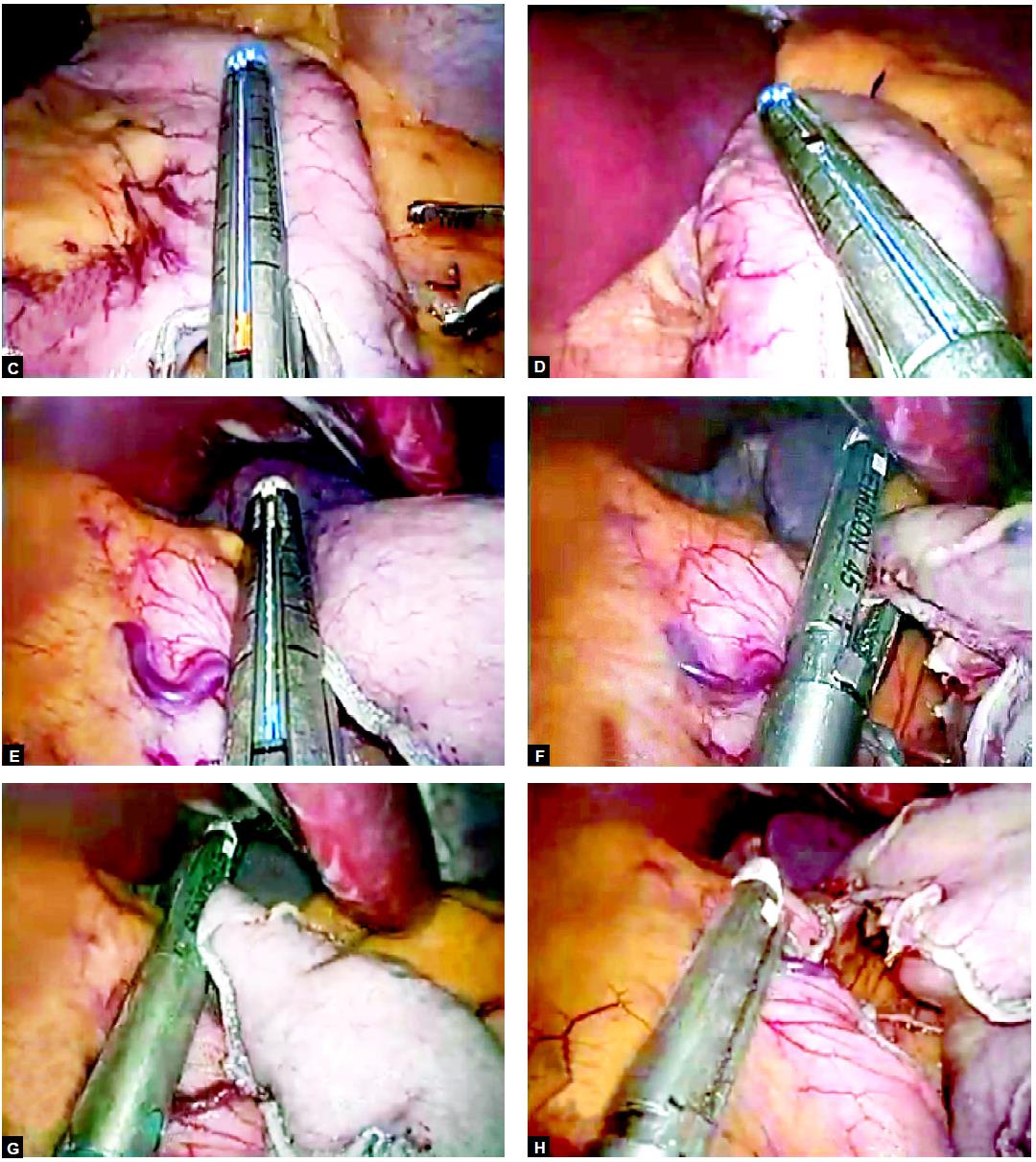
After the exploration of the abdomen and the anterior wall of the stomach, the liver is retracted via a fifth port. Dissection should be started with dissection of the short gastric vessels to the point of the angle of his using either the harmonic scalpel (Ethicon Endo-Surgery) or ligasure. The greater omentum is then separated from the greater curvature under the protection of the gastroepiploic arcade. The endpoint of the preparation is about 7 to 8 cm prepyloric. A 34-Fr tube is then positioned along the lesser curvature of the stomach as the leading structure for the stapling line to follow. After freeing the omentum, staple should be applied along the greater curvature strictly along the stomach tube using a 60-mm Endo-GIA, Ethicon Endo-Surgery, or Auto Suture. The starting point is 7 to 8 cm prepyloric to the point of the angle of His. Typically, four to five staple lines are needed. Different types of the stapler are available in the market.

Exposure of the stomach up to an angle of HIS

6 cm of the stomach towards the pylorus is left

Endo GIA stapler
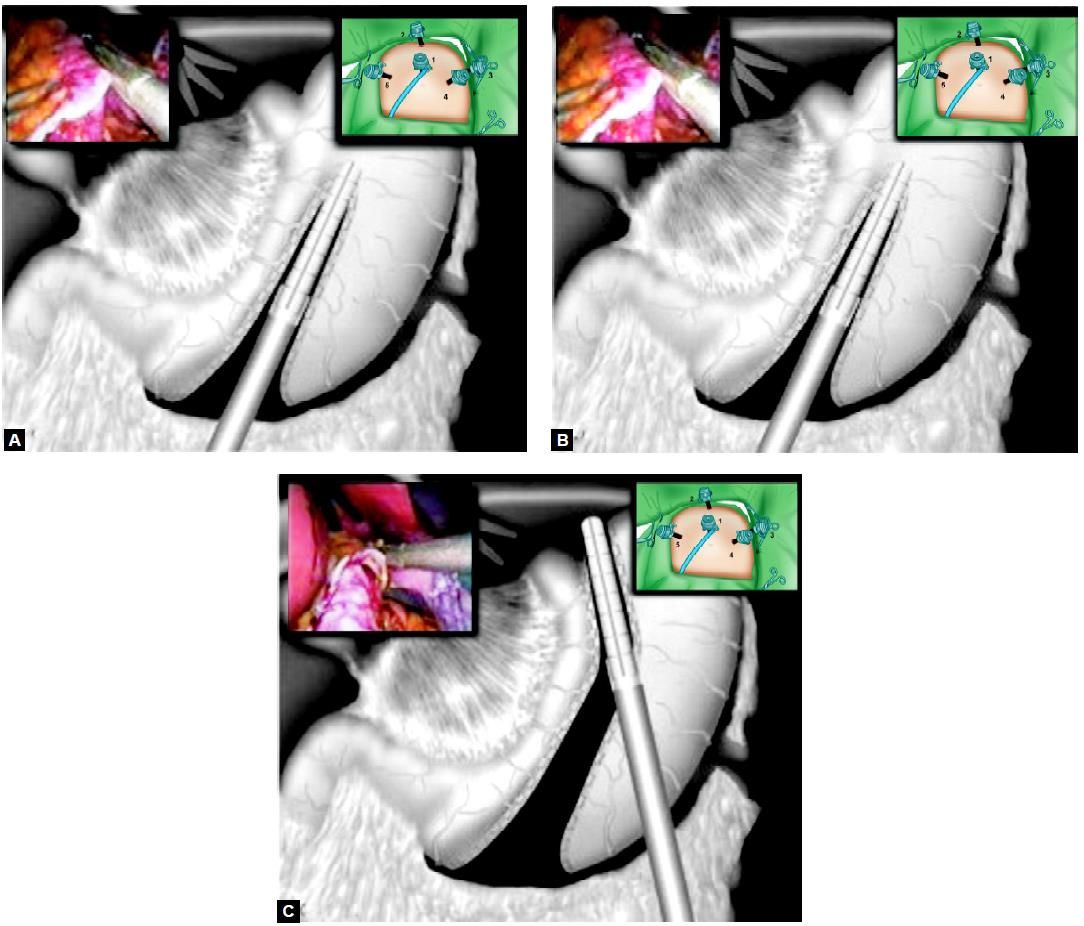
(A) After dissecting the greater omentum from the greater curvature, a 34-Fr stomach tube is placed along the lesser curvature. The first staple line is then set strictly along the stomach. The starting point of the dissection of the greater curvature is about 7-8 cm prepyloric
(B) The second staple line is set strictly and continued along the stomach tube
(C) Finishing of the gastric sleeve with the third staple line. The greater curvature is resected to the point of the angle of His
The dissected part of the stomach is withdrawn from the abdomen at port no: 3 and the staple line will be over-stitched by absorbable intracorporeal suturing. This is done not to prevent insufficiency in the staple line but rather to prevent staple line bleeding. It is possible to overstitch only areas of bleeding between the staples, not the whole staple line. Like most of the bariatric surgery operations, currently, there are multiple variations in the technique for the LSG. Some of these variations are the size of bougie (determines the size of the pouch) beside which the Endo GIA staplers are placed to divide the stomach, the level at which the surgeons start the division in the central area. Many surgeons leave most of the antrum for its pumping, emptying action and also to avoid the possibility of a leak from this thick-walled tough area, to reinforce or not reinforce this long-staple line.
Five or six ports are used for LSG and the surgeon standing between the patient's legs. An open technique could be used for the first port, establishing a pneumoperitoneum of 15 mm Hg. Then, two right ports, one left port, and midline ports are usually sufficient. The right subcostal trocar is used to insert the fan retractor for the liver. The camera should be placed high between the umbilicus and the xiphoid. Initial decompression of the stomach with NGT is preferable. Some surgeons commence the laparoscopic sleeve gastrectomy with an opening through the gastrocolic ligament to lesser sac, and the posterior stomach wall is visualized and fine adhesions to the pancreas are divided and the lesser sac totally freed using harmonic scalpel, ligasure, or coagulation hook. The left side of the GE junction should be cleared off fat to avoid later compromise of the stapling during the creation of the sleeve. The left crus should be exposed completely.

Dissection and mobilization of the stomach along the greater curvature outside the epiploic arcade
The majority of surgeons start the dissection 5 to 10 cm proximal to the pylorus, but some European surgeons start the dissection closer to the pylorus. If the dissection starts too close to the pylorus, the antrum will not empty properly and its pumping mechanism will be defective, thus postoperative nausea may occur. The linear Endo-GIA stapler is generally introduced through a right trocar towards the left shoulder and leaves about 1 cm of the fat pad along the lesser curvature (3 cm width). This assures adequate blood supply on the lesser curvature for the sleeve. Transaction of the stomach should be started 6 cm proximal to the pylorus and then the anesthesiologist inserts a 36 to 40-Fr bougie down to pylorus, if the LSG is intended as the sole operation but if as a preliminary step before the duodenal switch, a 60-Fr bougie is used. Kueper, et al consider a 34-Fr bougie which results in a pouch of 100 ml. The sleeve is started at the lower end of the crow's foot. The procedure requires five to six firings of the linear cutting stapler (60 mm long, 4.8 mm staple-height, and green cartridge) to divide the entire stomach. It is important to remove all fundus to avoid regain of weight. The vagus nerves anteriorly and posteriorly are preserved for normal gastric emptying.
Gastrectomy with the help of ENDO GI stapler
The resected greater curvature could be extracted in a bag via epigastric or right paramedian port-site after being dilated to two-finger diameter. The typical specimen has the shape of a comma or banana with the fundus at the top. In dividing the stomach, most surgeons use oversewing of the staple-line by continuous or interrupted absorbable sutures to prevent bleeding and leak.
Intraoperative testing through an 18-Fr Argyle tube with dilute methylene blue or air under saline using a gastroscope, with concurrent compression of prepyloric area is a complementary step. A Gastrografin® swallow is ordered by many surgeons on the second postoperative day, or others perform this study only if there is a problem. A liquid diet may be commenced on the first postoperative day.
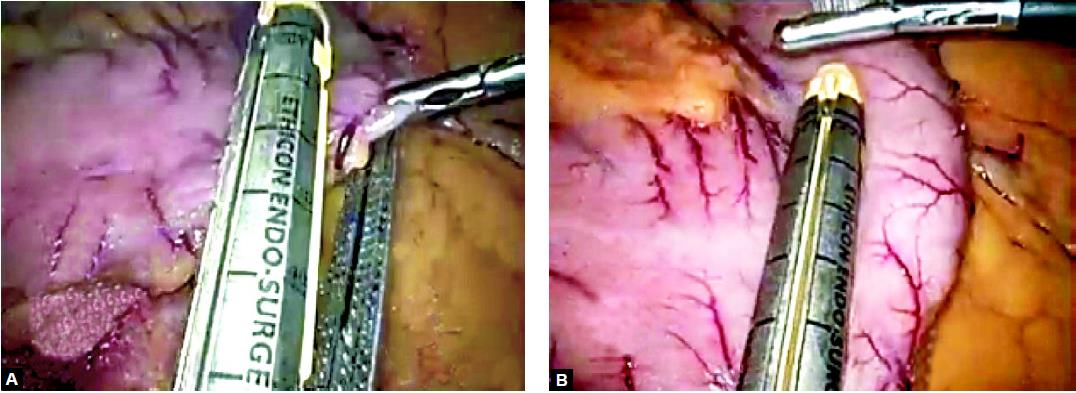
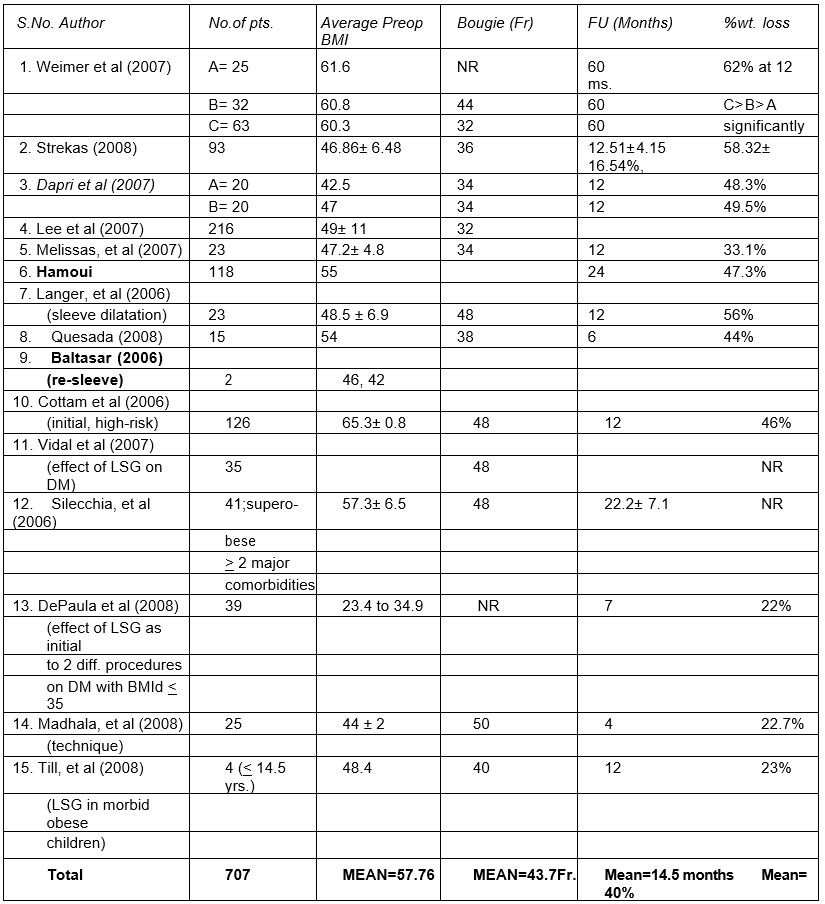
Weight Loss
"Durable" weight loss is the one most important gain of bariatric surgery operations, and it is the parameter by which success or failure of weight-reducing techniques is measured. The success of treatment has been defined as weight loss > 50 percent of excess weight, maintaining, or even losing further after surgery. The percentage weight loss after LSG in 707 morbidly obese patients included in the reviewed series is 40 percent (a mean) after a mean follow up of 14 months.
Effect on Associated Comorbidities
Laparoscopic sleeve gastrectomy had been carried out for super obese patients with multiple severe comorbidities and in at least 50 percent of the patients; there was marked improvement of the comorbidities especially diabetes mellitus which got marked benefit in 50 to 57 percent.
Outcome of published series on sleeve gastrectomy
The patient is positioned in a modified reverse Trendelenburg position with the right arm away from the body. The abdomen is prepared and draped in the customary fashion. Ports are used according to the baseball diamond concept as shown in the image below.
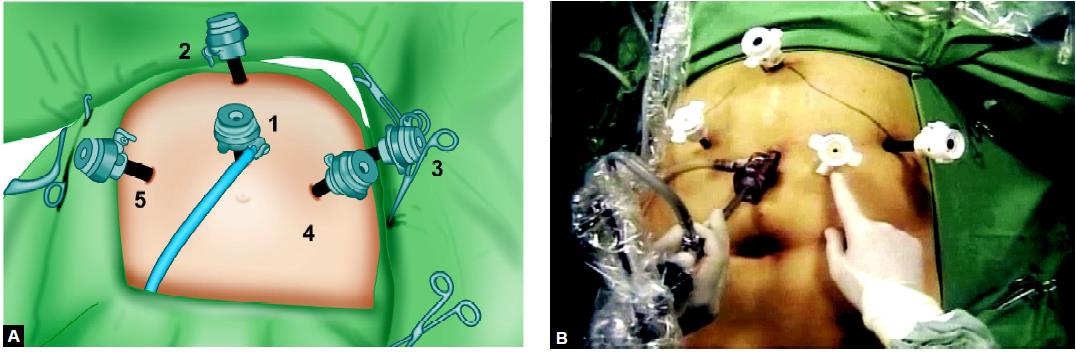
Port position for laparoscopic sleeve gastrectomy
After the exploration of the abdomen and the anterior wall of the stomach, the liver is retracted via a fifth port. Dissection should be started with dissection of the short gastric vessels to the point of the angle of his using either the harmonic scalpel (Ethicon Endo-Surgery) or ligasure. The greater omentum is then separated from the greater curvature under the protection of the gastroepiploic arcade. The endpoint of the preparation is about 7 to 8 cm prepyloric. A 34-Fr tube is then positioned along the lesser curvature of the stomach as the leading structure for the stapling line to follow. After freeing the omentum, staple should be applied along the greater curvature strictly along the stomach tube using a 60-mm Endo-GIA, Ethicon Endo-Surgery, or Auto Suture. The starting point is 7 to 8 cm prepyloric to the point of the angle of His. Typically, four to five staple lines are needed. Different types of the stapler are available in the market.

Exposure of the stomach up to an angle of HIS

6 cm of the stomach towards the pylorus is left

Endo GIA stapler
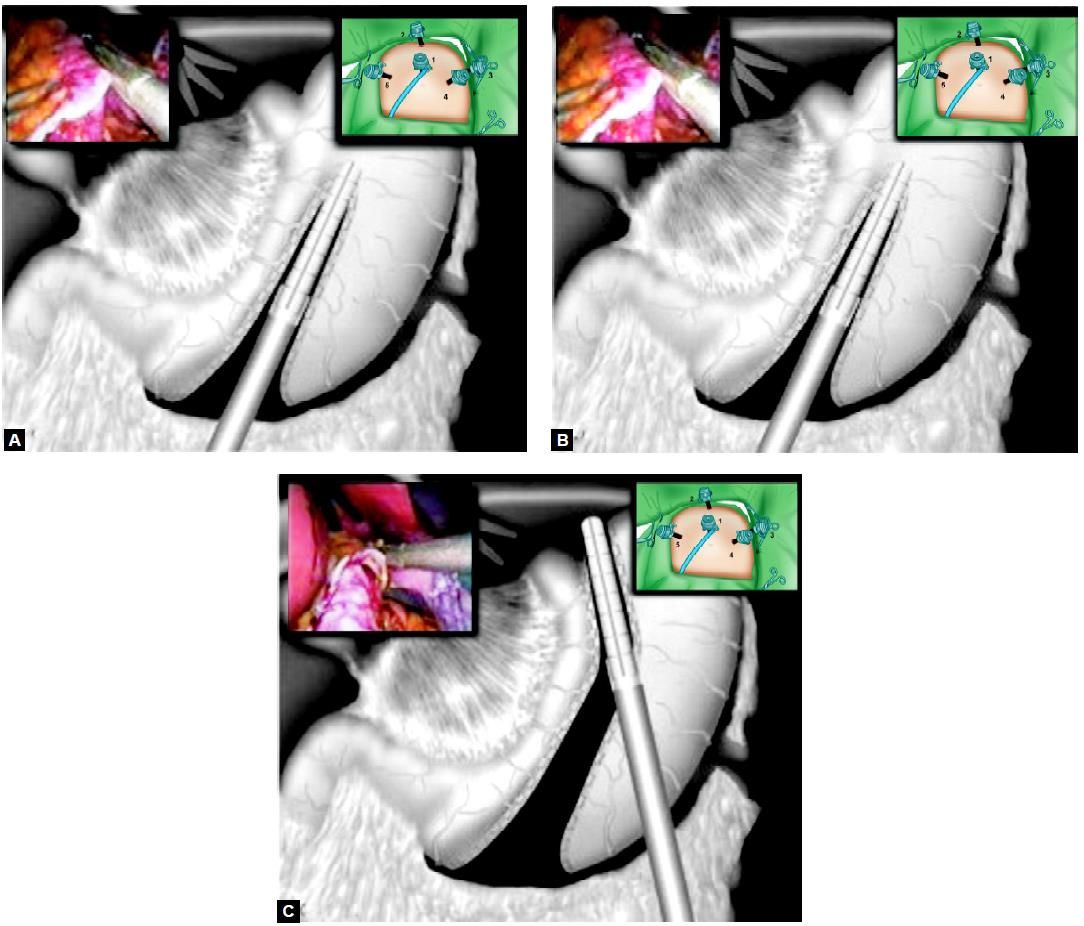
(A) After dissecting the greater omentum from the greater curvature, a 34-Fr stomach tube is placed along the lesser curvature. The first staple line is then set strictly along the stomach. The starting point of the dissection of the greater curvature is about 7-8 cm prepyloric
(B) The second staple line is set strictly and continued along the stomach tube
(C) Finishing of the gastric sleeve with the third staple line. The greater curvature is resected to the point of the angle of His
The dissected part of the stomach is withdrawn from the abdomen at port no: 3 and the staple line will be over-stitched by absorbable intracorporeal suturing. This is done not to prevent insufficiency in the staple line but rather to prevent staple line bleeding. It is possible to overstitch only areas of bleeding between the staples, not the whole staple line. Like most of the bariatric surgery operations, currently, there are multiple variations in the technique for the LSG. Some of these variations are the size of bougie (determines the size of the pouch) beside which the Endo GIA staplers are placed to divide the stomach, the level at which the surgeons start the division in the central area. Many surgeons leave most of the antrum for its pumping, emptying action and also to avoid the possibility of a leak from this thick-walled tough area, to reinforce or not reinforce this long-staple line.
Five or six ports are used for LSG and the surgeon standing between the patient's legs. An open technique could be used for the first port, establishing a pneumoperitoneum of 15 mm Hg. Then, two right ports, one left port, and midline ports are usually sufficient. The right subcostal trocar is used to insert the fan retractor for the liver. The camera should be placed high between the umbilicus and the xiphoid. Initial decompression of the stomach with NGT is preferable. Some surgeons commence the laparoscopic sleeve gastrectomy with an opening through the gastrocolic ligament to lesser sac, and the posterior stomach wall is visualized and fine adhesions to the pancreas are divided and the lesser sac totally freed using harmonic scalpel, ligasure, or coagulation hook. The left side of the GE junction should be cleared off fat to avoid later compromise of the stapling during the creation of the sleeve. The left crus should be exposed completely.

Dissection and mobilization of the stomach along the greater curvature outside the epiploic arcade
The majority of surgeons start the dissection 5 to 10 cm proximal to the pylorus, but some European surgeons start the dissection closer to the pylorus. If the dissection starts too close to the pylorus, the antrum will not empty properly and its pumping mechanism will be defective, thus postoperative nausea may occur. The linear Endo-GIA stapler is generally introduced through a right trocar towards the left shoulder and leaves about 1 cm of the fat pad along the lesser curvature (3 cm width). This assures adequate blood supply on the lesser curvature for the sleeve. Transaction of the stomach should be started 6 cm proximal to the pylorus and then the anesthesiologist inserts a 36 to 40-Fr bougie down to pylorus, if the LSG is intended as the sole operation but if as a preliminary step before the duodenal switch, a 60-Fr bougie is used. Kueper, et al consider a 34-Fr bougie which results in a pouch of 100 ml. The sleeve is started at the lower end of the crow's foot. The procedure requires five to six firings of the linear cutting stapler (60 mm long, 4.8 mm staple-height, and green cartridge) to divide the entire stomach. It is important to remove all fundus to avoid regain of weight. The vagus nerves anteriorly and posteriorly are preserved for normal gastric emptying.
Gastrectomy with the help of ENDO GI stapler
The resected greater curvature could be extracted in a bag via epigastric or right paramedian port-site after being dilated to two-finger diameter. The typical specimen has the shape of a comma or banana with the fundus at the top. In dividing the stomach, most surgeons use oversewing of the staple-line by continuous or interrupted absorbable sutures to prevent bleeding and leak.
Intraoperative testing through an 18-Fr Argyle tube with dilute methylene blue or air under saline using a gastroscope, with concurrent compression of prepyloric area is a complementary step. A Gastrografin® swallow is ordered by many surgeons on the second postoperative day, or others perform this study only if there is a problem. A liquid diet may be commenced on the first postoperative day.
Weight Loss
"Durable" weight loss is the one most important gain of bariatric surgery operations, and it is the parameter by which success or failure of weight-reducing techniques is measured. The success of treatment has been defined as weight loss > 50 percent of excess weight, maintaining, or even losing further after surgery. The percentage weight loss after LSG in 707 morbidly obese patients included in the reviewed series is 40 percent (a mean) after a mean follow up of 14 months.
Effect on Associated Comorbidities
Laparoscopic sleeve gastrectomy had been carried out for super obese patients with multiple severe comorbidities and in at least 50 percent of the patients; there was marked improvement of the comorbidities especially diabetes mellitus which got marked benefit in 50 to 57 percent.
Outcome of published series on sleeve gastrectomy