Role of Training in Minimal Access Surgery
Introduction
The popularity of laparoscopic techniques has led to a new domain in surgical training, with a move away from the apprenticeship model, toward structured programs of teaching new skills outside the operating room. Hands-on courses enables young surgeons to practice techniques on synthetic, porcine, or more recently virtual-reality models, are now common place. The aim has been to ensure trainees are armed with basic laparoscopic skills, such as hand-eye coordination and depth perception prior to entering the operating room. The success of these initial courses led to the development of similar courses for the advanced laparoscopic skills required for gastric and colonic surgery.
Demonstration of different types of knot to keep them in memory
Compared to aviation, where virtual reality (VR) training has been standardized and simulators have proven their definite benefit in increasing skill, the objectives, needs, and means of VR training in minimal access surgery (MIS) is established.

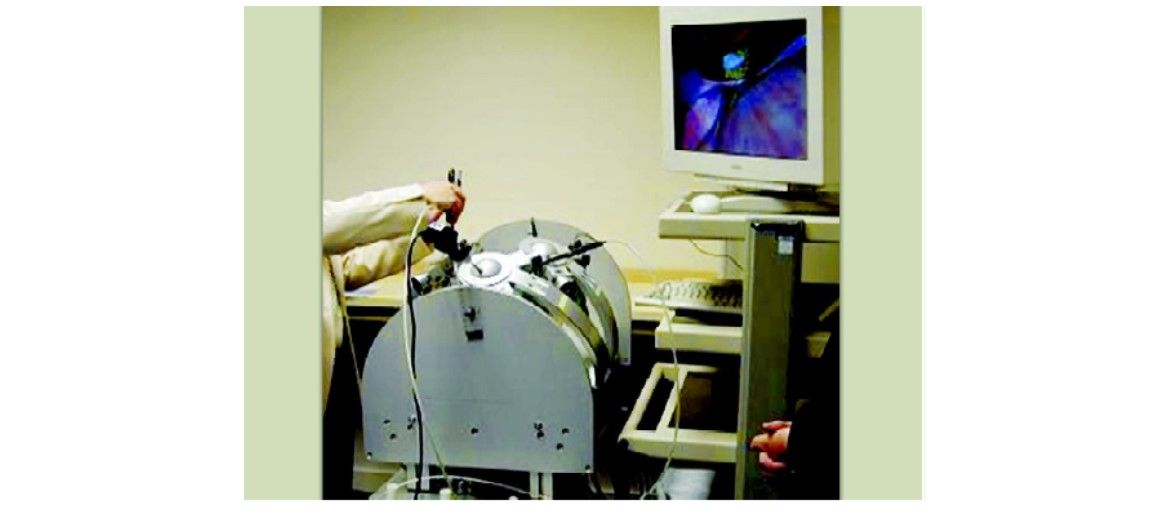
Different types of simple pelvitrainers
Rasmussen distinguishes three levels of human behavior:
1. Skill-based level
2. Rule-based level
3. Knowledge-based behavior
Skill-based Behavior
This represents surgeon’s behavior that takes place without conscious control. Task execution is highly automated at this level of behavior and is based on fast selection of motor programs which control the appropriate muscles. The motor programs are based on an accurate internal representation of the task, the system dynamics, and the environment at hand (e.g. learned by training and experience). An example of an everyday skill is walking. Many tasks in surgery can be considered as a sequence of skilled acts. For example, an experienced surgeon performs a suture task smoothly, without conscious control over his or her movements.
In MIS, suturing can also be considered as skill-based behavior. However, because of the indirect access to the tissue, it is a much more complicated skill because of reduced depth perception and difficult hand-eye coordination.
Pelvitrainer exercises to improve skill
Rule-based Behavior
At the next level of human behavior, rule-based behavior is applied. During rule-based behavior task execution is controlled by stored rules or procedures. These may have been derived empirically from previous occasions or communicated from other persons’ expertise as instructions or as a cookbook recipe. Appropriate rules are selected according to their ‘‘success’’ in previous experiences. For example, procedural steps and the recognition of anatomy and pathology in MIS require rule-based behavior. At the rule-based level, the information is typically perceived as discrete signs. A sign serves to activate or to trigger a stored rule. Stopping your car in front of a red light is a good example of a sign (red light) that triggers a stored rule (stop car). In laparoscopic cholecystectomy, having fully established the critical view of safety is the sign that triggers the rule that the appropriate structures may be clipped next.
Knowledge-based Behavior
In unfamiliar situations, faced with a task for which no rules are available from previous encounters, human behavior is knowledge-based. During knowledge-based behavior the goal is explicitly formulated, based on an analysis of the overall aim. Different plans are developed, and their effects mentally tested against the goal. Finally a plan is selected. Serious complications that occasionally occur during surgery demand a great deal of knowledge-based behavior from the surgeon. He or she has to analyze the complication and the aim of the surgical procedure in order to develop strategies to counter the complication. Then he or she has to select the best strategy and consequently take the appropriate actions.
At the knowledge-based level, information is perceived as symbols. Symbols refer to chunks of conceptual information, which are the basis for reasoning and planning. Pathological symptoms are a good example of symbols in medical practice.
Training in laparoscopic surgery is beginning to evolve into a stepwise, curricular approach that is not organ or procedure-specific. Instead, it is necessary to learn manipulative skills, which are then combined to achieve proficiency in tasks such as laparoscopic suturing or division of a vessel. The constituent parts can then be combined with anatomical knowledge to enable completion of a specific procedure. Basic psychomotor skills can be learnt with a simple, cheap version of a video-box trainer. Higher level skills such as dissection and use of high-energy instruments will necessitate the use of more realistic tissues, which can be achieved on porcine or human cadaveric models. Recent advances in virtual reality simulation are also beginning to produce realistic simulations of complete procedures, for example, laparoscopic cholecystectomy.
It would be rational to assume that a high-fidelity simulation model, such as anesthetized animal tissue, would be superior in terms of training outcome to a synthetic plastic model.
The simple pelvitrainer can be used for improving suturing skill
In fact, a study comparing two groups learning to perform microanastomotic repair of a transected spermatic cord on either the animal or synthetic model found no difference in eventual outcome of the two groups. The synthetic model is obviously cheaper and does not require specialized storage facilities. It can be assumed that as the subjects were using real sutures and instruments, the nature of the task was learnt regardless of the fidelity of the simulated tissue.
Training—Objectives, Needs, and Means
To enable the design and evaluation of an effective and efficient training method it is of utmost importance to determine the training objectives, needs, and means, since they provide an answer to the questions:
1. What is the end goal of the training?
2. What should be trained?
3. How can we train it?
The objectives represent the level of competence that is expected of the trainee after he or she has completed the training. Training needs are the difference between the initial level of competence of the trainees and the required level of competence after successful completion of the training defined in the objectives. Ultimately, demands for effectivity and efficiency on the one hand, and the state-of-the-art in technology on the other hand, determine the tools and methods for training, i.e. the training means. Effective training ensures that all training objectives are met. Efficient training ensures that the training means are cost effective and that the required training time is minimized. Since safety and patient outcome are the most important criteria in surgery, training effectivity should be of primary importance
.
The complexity and the costs of the training means are largely determined by the training objectives that have been set. Fulfilling all training needs of laparoscopic residents with only one training method will require a highly complex and probably very expensive trainer in which all three levels of behavior can be trained. Such a trainer is not yet available. The complexity and the cost of a training means are relatively low if the training objectives comprise skill-based behavior only, since this can be trained with simple models such as pelvitrainers. Evidently, the cost and complexity of a training means increase when the training objectives advance from the training of skill-based behavior to the training of knowledge-based behavior. Fortunately, the overall effectivity of training increases as well when higher levels of behavior, such as knowledge-based behavior, are incorporated in the training objectives.
Present Training in Laparoscopy
A closer look at the training program of laparoscopic residents provides an indication of the training needs that are addressed and the training means that are available today. Much as in conventional surgery, the laparoscopic surgeon must effectively combine the three levels of behavior. Instrument handling and dissection techniques require skill-based behavior, whereas the recognition of surgical anatomy requires a great deal of rule-based behavior. Complications such as uncontrollable bleeding or unsuspected situations such as the encountering of aberrant anatomy require problem solving on a knowledge-based level.
Obviously, training of skill-based behavior in laparoscopic surgery is highly desired as laparoscopy combines unusual hand-eye coordination with the use of complex instruments. Surgical residents are usually trained in laparoscopic surgery during a 2 days introduction course. Basic skill-based behavior such as instrument tissue handling and minimally invasive suturing are trained. Additionally, rule-based behavior is trained through lectures, textbooks, and video instructions. After the resident has successfully completed this course, he or she will receive training in the operating room. It is only in operating room that most knowledge-based behavior necessary to deal with complications and emergencies is acquired. Currently, a living animal model provides the only way to effectively train rule- and knowledge-based behavior outside the operating room. Training on living animal models is very useful in the training curriculum of resident surgeons. However, at the same time the use of laboratory animals for training is discouraged by many government policies. Technological innovations, such as virtual reality simulation, will change the way laparoscopic surgery is trained. Current accomplishments in surgical simulation envision the dawning of the next-generation surgical education. In this respect, aviation industry provides excellent examples of the effectiveness and efficiency of virtual reality simulators as a means of training.
Simulator training in aviation in contrast to surgery, the training needs in aviation has explicitly been defined by regulatory authorities like Federal Aviation Administration (FAA) and the training means are certified accordingly. The training objectives, needs, and means in pilot training have been investigated in depth, and models of pilot behavior have been developed as a tool to design, to evaluate, and to optimize training methods. Half a century of extensive research has resulted in many training tools, from basic flight training devices to the high-tech full flight simulator (FFS).
HALS training box
After the introduction of VR training methods in the 1990s, the training of surgeons has often been compared to the training of pilots. The training of laparoscopic residents can best be compared to type conversion training of pilots. During type conversion training, young pilots who have finished flight training at the academies and have recently joined an airline are trained to fly a particular type of aircraft. The general objective of type conversion training is to teach the trainee how to safely control, navigate, and manage a particular operational aircraft. Since the trainees have already acquired much of the skill-based behavior required to fly a multiengine aircraft, the training needs mainly consist of acquiring additional rule- and knowledge-based behavior. The trainees have to learn the new checklists and the specific procedures during takeoff and landing, and they have to become familiar with all the aircraft systems like electronics, hydraulics. Furthermore, they have to train all sorts of emergency scenarios that may occur during actual flight. Training of this knowledge-based behavior is very important since it significantly improves flight safety. This training provides an excellent training tool to accomplish all the specified training needs. The high level of realism during training of a pilot have even made zero flight time training possible, during which type conversion training takes place completely outside a real aircraft.
For the sake of proper training and for the safety of our patients, the objectives, needs, and means in laparoscopy training should be defined. Along this guideline, VR simulators should be developed. An explicit formulation of the training objectives facilitates the development and certification of a simulator since it determines what the simulator should be capable of. For example, pilots spend many hours training on low-cost simulators.
Virtual reality trainer with programmable circuit
The laparoscopy simulators that have been developed during the past decade can all be considered as laparoscopy training devices. Most of these simulators specifically aim at training skill-based behavior, such as endoscopic manipulation and endoscopic camera navigation. However, performing safe laparoscopy also requires a professional level of rule- and knowledge-based behavior from the surgeon. Ideally these should also be trained outside the operation theatre. Currently, the training of rule- and knowledge-based behavior outside the operation theatre is only possible on living animal models. However, technological innovations like increasing computing power, detailed anatomical models, soft tissue modeling, force feedback will enable the integration of all levels of behavior in a VR training simulator for laparoscopy. In the future, this might result in a full-scale laparoscopy simulator (FLS), comparable to the FFS in pilot training. Perhaps a FLS even introduces zero operating time training as the ultimate objective.
The medical society should establish detailed objectives of training. Recently, experts have begun to investigate what level of professional behavior is required to perform safe laparoscopy. In addition, they are establishing the training needs of laparoscopic residents by determining what should be trained to accomplish the training objective. The question of which aspects of skill, rule, and knowledge-based behavior should be trained is addressed. Currently, there is no such standard available. Once the training objectives have been standardized and the training needs at the different levels of behavior have been identified, the simulator society will have clear guidelines as to what their training devices should be capable of.
One of the most obvious training needs of laparoscopic residents is the training of manual skills. The manual skills required during laparoscopy are rather different from those in conventional surgery. Training of skill-based behavior is feasible with basic trainers such as a pelvitrainer. The VR basic skill trainers that are commercially available usually simulate a generic abdomen and endoscopic instruments on a computer monitor. Basic tasks, such as pick and place tasks, are implemented to train endoscopic manipulation. The training of skill-based behavior does not require a highly realistic anatomical environment, e.g. the organs do not necessarily have to be simulated realistically. For example, the virtual reality trainer simulates basic manipulation tasks in a highly simplified environment similar to the pelvitrainer box. Several studies have reported that training on the virtual reality facilitated the learning of skill-based behavior.
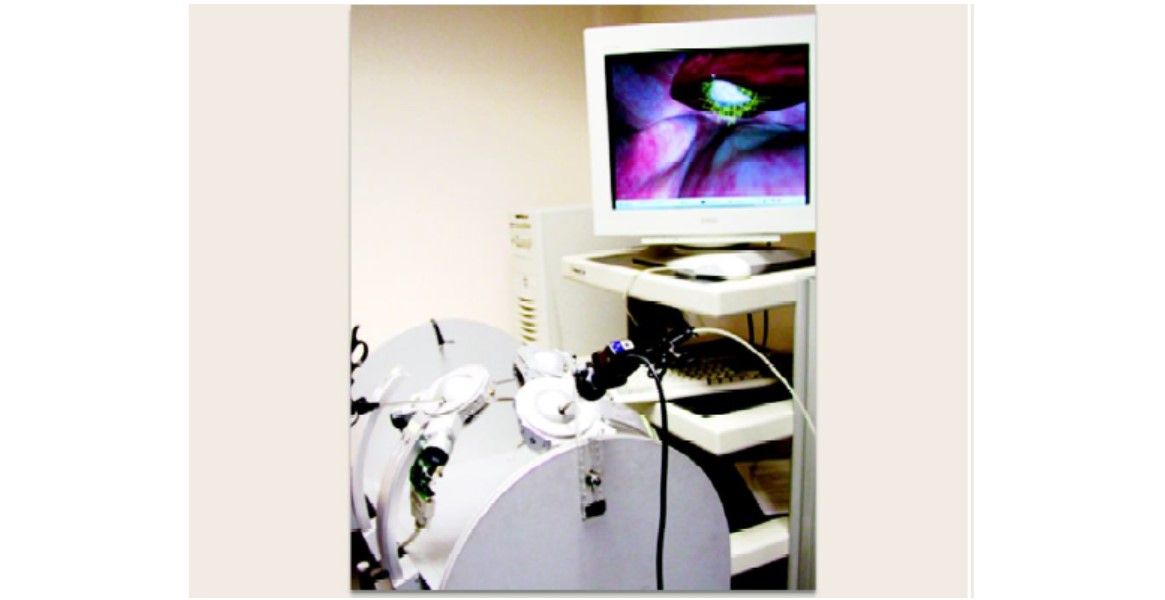
Virtual reality trainer with software control
An advantage of virtual reality simulators over simple. Pelvitrainers is the capability to easily extend the training to the rule-based level of behavior, since textbook theory, instructions, and training videos can easily be integrated in the simulator software. Much textbook material and many training videos that provide rule-based behavior training have been made available on the internet. Laparoscopy simulators are capable of training skill and rule-based behavior. To train knowledge-based behavior, a laparoscopy simulator should be capable of accurately imitating the surgical environment encountered during laparoscopic surgery.

Virtual reality trainer for LAVH
The perceived information from the environment should be simulated accurately to ensure effective training. The training of knowledge-based behavior on a simulator still poses a huge challenge. Two fundamental problems occur. Whereas the physics that determine the behavior of an aircraft is fairly well known and described mathematically, the physics that describes the behavior of soft-tissue organs is highly complicated and many parameters are simply still missing. Additionally, each aircraft roughly has the same flight characteristics and cockpit layout, but each new patient has a different anatomical layout than the previous one. Laparoscopy simulators have to be able to generate ‘‘random’’ patients.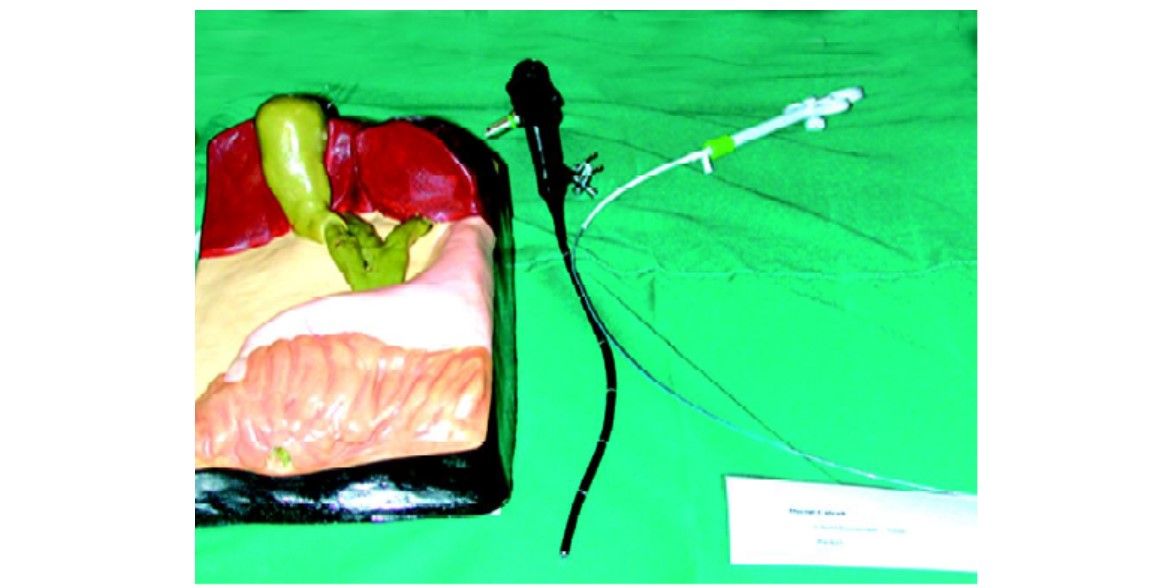
Simulated models of GB and CBD to improve choledochoscopic skill
The integration of knowledge-based behavior training in a future simulator would enhance safety levels in laparoscopy, since then every possible surgical complication could be trained beforehand. As in aviation, intensive training can reduce a situation that at first required improvising at a knowledge-based behavior level from the trainee, to a situation that can be solved by applying trained rules.
Learning Curve in Laparoscopy
TP Wright originally introduced the concept of a learning curve in aircraft manufacturing in 1936. He described a basic theory for costing the repetitive production of airplane assemblies. The term was introduced to medicine in the 1980s after the advent of minimal access surgery. It also caught the attention of the public and the legal profession when a surgeon told a public enquiry in Britain that a high death rate was inevitable while surgeons were on a learning curve. Recently, it has been labeled as a dangerous curve with a morbidity, mortality and unproven outcomes. Yet there is no standardization of what the term means. In an endeavor to help laparoscopic surgeons towards evidence based practices, this commentary will define and describe the learning curve, its drawing followed by a discussion of the factors affecting it, statistical evaluation, effect on randomized controlled trials and clinical implications for both practice and training, the limitations and pitfalls, ethical dilemmas and some thoughts to pave the way ahead.
Definition and Description
For the Wright learning curve, the underlying hypothesis is that the direct man-hours necessary to complete a unit of production will decrease by a constant percentage each time the production quantity is doubled. In manufacturing, the learning curve applies to the time and cost of production. Can a surgeon’s learning curve be described on similar lines? A simple definition would be: The time taken and/or the number of procedures an average surgeon needs to be able to perform a procedure independently with a reasonable outcome. But then who is an average surgeon? Another definition may be that a learning curve is a graphic representation of the relationship between experience with a new procedure or technique and an outcome variable such as operation time, complication rate, hospital stay or mortality. A learning curve may also be operationally defined as an improvement in performance over time. Although learning theorists often disagree about what learning is, they agree that whatever the process is, its affects are clearly cumulative and may therefore be plotted as a curve. By cumulative it is meant that somehow the effects of experience carry over to aid later performance. This property is fundamental to the construction of learning curves. The improvement tends to be most rapid at first and then tails off. Hence, there are three main features of a learning curve. First, the initial or starting point defines where the performance of an individual surgeon begins. Secondly, the rate of learning measures how quickly the surgeon will reach a certain level of performance and thirdly the asymptote or expert level measures where the surgeon’s performance stabilizes. This has implications for the laparoscopic surgeon—it suggests that practice always help improve performance but the most dramatic improvement happens first. Also, with sufficient practice, surgeons can achieve comparable levels of performance.
The Drawing of Learning Curves
There are a variety of methods of constructing learning curves. They all assume that successive exposures in a learning series may be plotted on the X-axis, response characteristics on Y-axis and the data points distributed in the XY plane may be legitimately connected by a curve. This is the Cartesian method. More recently, the cumulative sum method has been applied for the construction of these curves for basic skills in anesthetic procedures—the method consists of relatively simple calculations that can be easily performed on an electronic spreadsheet. Statistical inferences can be made from observed success and failure. The method also provides both numerical and graphical representation of the learning process.
The multimode learning curve is useful because several factors can be put into one graph. The earlier used method of the performance analysis with it’s on the spot appraisals at certain time intervals have been replaced by continuous assessment. For continuous data like operation time the moving average method is useful.
Factors Affecting Learning Curves
Complex hierarchies of factors are involved here. Factors like guidelines, protocols and standards for clinical governance agreed upon by the medical fraternity are vital. Next, the institutional policies and cost effectiveness are contributory. Needless to say the surgical team, the case mix and public awareness are relevant. The final level in the hierarchy that can influence individual learning is the characteristics of the surgeon such as attitude, capacity for acquiring new skills and previous experience.
Amongst the latter, that is the characteristics of the surgeon, the learning curve may depend on the manual dexterity of the individual surgeon and the background knowledge of surgical anatomy. The type of training the surgeon has received is also important as training on inanimate trainers and animal tissue has been shown to facilitate the process of learning. The slope of the curve depends on the nature of the procedure and frequency of procedures performed in specific time period. Many studies suggest that complication rates are inversely proportional to the volume of the surgical workload. However, rapidity of learning is not significantly related to the surgeon’s age, size of practice or hospital setting. Another important factor that affects the learning curve is the supporting surgical team. A recent observational study to investigate the incidence of technical equipment problems during laparoscopic procedures reported that in 87 percent of procedures one or more incidents with technical equipment or instruments occurred. Hence, improvement and standardization of equipment combined with incorporation of check lists to be used before surgery has been recommended.
Statistical Evaluation of Learning Curves
Various statistical methods have been reported in the assessment of the learning curve. Commonly data are split into arbitrary groups and the means compared by chi- squared test or ANOVA. Some studies had data displayed graphically with no statistical analysis. Others used univariate analysis of experience versus outcome. Some studies used multivariate analysis techniques such as logistic regression and multiple regression to adjust for confounding factors. A systematic review concluded that the statistical methods used for assessing learning curves have been crude and the reporting of studies poor. Recognizing that better methods may be developed in other nonclinical fields where learning curves are present (psychology and manufacturing) a systematic search was made of the nonclinical literature to identify novel statistical methods for modeling learning curves. A number of techniques were identified including generalized estimating equations and multilevel models. The main recommendation was that given the hierarchical nature of the learning curve data and the need to adjust for covariant, hierarchical statistical models should be used.
Effect of Learning Curve on Randomized Controlled Trials
The learning curve can cause difficulties in the interpretation of RCTs by distorting comparisons. The usual approaches to designing trials of new surgical techniques has been either to provide intensive training and supervision or require participating surgeons to perform a fixed number of procedures prior to participation in a trial. Surgeons have been reluctant to randomize until they are proficient in a technique but once convinced of its worth, argue that it is too late to randomize. However, the best way to address the problem is to have a statistical description of the learning curve effect within a trial and various methods can then be used example Bayesian hierarchical model.
Implications for Practice and Training
In the current era of evidence based medicine enthusiasm for laparoscopic surgery is rapidly gaining momentum. There is an immense amount of literature showing advantages of minimal access surgery and acceptance by the public. The learning curve for many procedures has been documented. As far as training is concerned, the introduction of laparoscopic techniques in surgery led to many unnecessary complications. This led to the development of skills laboratories involving use of box trainers with either innate or animal tissues but lacks objective assessment of skill acquisition. Virtual reality simulators have the ability to teach psychomotor skills. However, it is a training tool and needs to be thoughtfully introduced into the surgical training curriculum. A recent prospective randomized controlled trial showed that virtual simulator combined with inanimate box training leads to better laparoscopic skill acquisition. An interesting finding reported is that in skills training every task should be repeated at least 30 to 35 times for maximum benefit. The distribution of training over several days has also been shown to be superior to training in one day. Other factors enhancing training are fellowship programmer, or playing video games. One can also obtain feedback for improvement of training program. In one such study, the deficiency factors identified were lack of knowledge, lack of synchronized movement of the nondominant hand and easy physical fatigue. Incorporation of intensive, well planned in vitro training into the curriculum was made and the programmed reassessed.
What are the Limitations or Pitfalls?
“Steep” learning curves are usually used to describe procedures that are difficult to learn. However, this is a misnomer as it implies that large gains in proficiency are achieved over a small number of cases. Instead the curve for a procedure that requires a lot of cases to reach proficiency should be described as “flattened”.
As long as no valid scoring system concerning the complexity of a surgical intervention exists, the learning curve cannot be used as benchmarks to compare different surgeons or clinics as legitimate instruments to rank surgeons or different hospitals. Limitations of long learning curves, facilities for training, mistakes of pioneers, surgical techniques not being described in books are some of the limitations. There are other limitations due to the nature of laparoscopic surgery like the lack of 3D vision and of tactile sensations, difficult hand eye coordination and long instruments.
Ethical Dilemmas
Many dilemmas exist and many questions will always be with us—who bears the burden of the learning curve? Are the patients aware of the risks? Many reports validate the impression that a patient operated upon during the learning curve takes greater risks and incurs more adverse circumstances than the patient operated upon later. The issue of how informed the informed consent should be needs to be addressed. Is the integrity and conscience of a surgeon measurable? Should the forces of marketing be curtailed or regulated?
The Way Forward
Laparoscopic surgery is here to stay and success in it is determined by how quickly and effectively we learn. However, certain measures may be taken to lessen some of the adverse effects of the learning curve and others to help laparoscopic surgeons ease into the specialist. Setting up of minimal standards and credentialing is a must. Current guidelines in many countries are vague and general. The evidence for training is well documented. The message for individual surgeons is to identify their deficiencies, and chart a way forward for their personal graph of progress. Evaluation and monitoring in a systematic scientific manner will benefit the surgeon with a satisfactory learning curve that will ensure that patient welfare is not compromised.
Conclusion
In this article, it has been pointed out that it is important to establish the training objectives, needs, and means, since they provide an answer to the questions. What is the end goal of the training?, What should be trained?, and How can we train it? Rasmussen’s model of human behavior provides a practical framework for the definition of the training objectives, needs, and means in MIS, and the evaluation thereof.





