Uterine artery ligation in laparoscopic hysterectomy and myomectomy technique and outcome
Purpose: To review the feasibility of ligating the uterine artery in laparoscopic hysterectomy and myomectomy and its advantages in ligating the vessel and understanding the benefits and disadvantages.
MATERIALS AND METHODS: From literature published in Pub Med, Medline biomedicine data base, obstetrics and gynecology journal, Journal of the society of laparoendoscopic surgeons, Journal of Minimally invasive gynecology, Journal of Minimally invasive surgery, Google images.
RESULTS: Uterine artery being a large vessel with varied anatomy and high pressure artery it is good to ligate the artery during laparoscopic hysterectomy. This technique which resulted in reduced intraoperative blood loss and increases the success rate of laparoscopic surgeries. Laparoscopic uterine artery ligation can also be done in association with laparoscopic myomectomy, or just laparoscopic uterine artery ligation (LUAL) in symptomatic fibroid. Studies show decreased intraoperative bloodloss, reduced recurrence of myoma, and good response from symptoms. Better alternative to uterine artery embolism (UAE) in patients who wants preserve fertility in symptomatic fibroid.
Conclusion: It is feasible to ligate the uterine artery during the laparoscopic hysterectomy and laparoscopic myomectomy. Any complications of the surgery can be minimized without conversion to laparotomy by sufficiently developed suturing technique and knowledge of retroperitoneal anatomy.
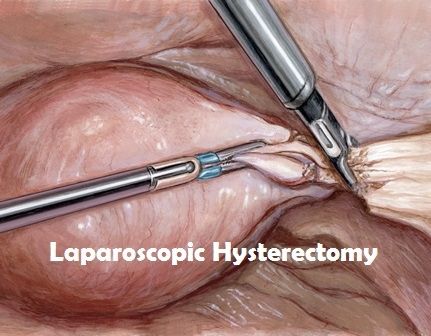
¹Hysterectomy is most common gynecologic surgery. The appropriate route to surgery is determined by the type of the pathology expected, anatomical considerations, patient’s preference, surgeons experience and training.
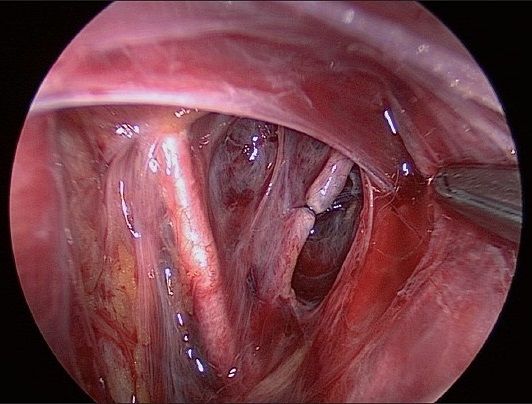
²Laparoscopic approach with appropriate surgical technique has advantages like magnification of anatomy and pathology by 7-10 fold easy access to retroperitoneal space to ligate the uterine artery because of the pneumoperitoneum. Pneumoperitoneum facilitates development of the pelvic spaces, decreases the venous bleeding, there by maintaining a clean operative field while dissecting, access to vagina and rectum and bility to achieve complete hemostasis and clot evacuation.
³Other advantages are avoidance of painful large incision, reduced duration of hospital stays, low rate of infection and ileus and recuperation time. Having many advantages of laparoscopic surgeries, uterine artery ligation increases the success rate of laparoscopic surgery. Total laparoscopic hysterectomy (TLH) includes uterine artery ligation and complete dissection of the uterus from its attachments. Technique and benefits of identifying and ligating the uterine artery in TLH and laparoscopic myomectomy.
Surgeon should know precise anatomy of the pelvis. Uterine artery can be ligated at the origin of the artery, or lateral to where it crosses over the ureter, or just at the level of internal os where uterine artery gives of ascending branch and cervical branch just beside the uterus.
ANATOMY OF UTERINE ARTERY:
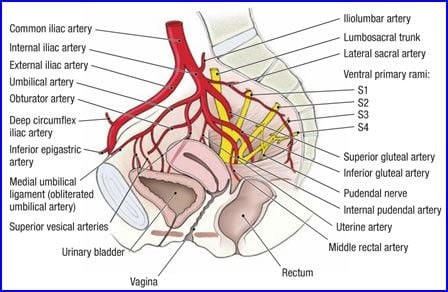
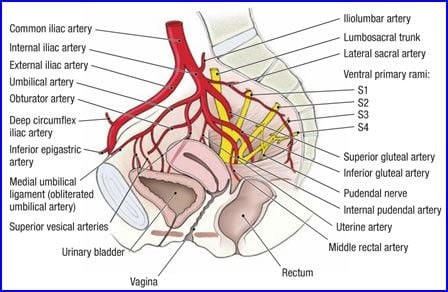
Uterine artery is a branch of anterior division of the internal iliac artery. It is the first medial branch of internal iliac artery. It arises below the Obturator artery on the lateral pelvic wall and runs inferomedially into the broad ligament. Umbilical artery also a branch of the anterior division of internal iliac artery is the surgical land mark that leads to the origin of uterine artery and superior vesical artery. It is studied in three segments.
In the broad ligament It course is first downwards and forwards until it reaches the parametrium when it turns medially to the level of internal os then it crosses the ureter anteriorly before it branches. It reaches the uterus at the level of cervicouterine junction, it gives one major branch which ascends along the lateral border of the uterus tortuously within the broad ligament until it reaches the region of the ovarian hilum, where it anastomoses with the branch of ovarian artery. Another branch descends to supply the cervix and anastomose with branches of the vaginal artery. These branches are 2-6 mm in diameter. The ascending branch and ovarian arteries anastomose to perfuse the uterus. Arcuate arteries arise from ascending branch, runs transversely within the wall of uterus and radial arteries penetrate deeply into the myometrium. The presence of leiomyomas in the uterus distorts the normal vascular architecture.
Branches of uterine artery - Vesicovaginal artery, Cervico vaginal artery, Sinuous cervical artery, corporeal artery, Vaginal artery and Round ligament artery.
ANATOMY OF URETER: It is 25-30 cm long and has thickened wall and narrow lumen (3mm) continuous with renal shape pelvis extending from pelviureteric junction to bladder. It is a retroperitoneal structure in the posterior abdominal wall and lateral pelvic wall, each ureter descends slightly medially and anterior to psoas major and enters the pelvic cavity where it curves initially laterally and then medially, to open into the base of the bladder. It is narrow at renal pelvis, brim of the lesser pelvis and within wall of urinary bladder.
Abdominal ureter: Passes downwards and medially to lie on the medial edge of the psoas major, at this level, anteriorly the ureter is covered at its origin by the second part of the duodenum and then lies lateral to the inferior vena cava and behind the posterior peritoneum Right ureter is crossed by the ovarian, right colic, and iliocolic vessels. The left ureter is crossed by the ovarian and the left colic vessels. Then enters into the pelvis at the bifurcation of the common iliac artery in front of the sacroiliac joint. Then it enters the true pelvis where it is crossed by the ovarian vessels, behind the mesosigmoid and sigmoid colon.
In the pelvis the ureter lies is anterior to the internal iliac artery it is behind the ovary forming the posterior boundary of the ovarian fossa. Laterally it lies on the fascia of obturator internus progressively crosses to become medial to umbilical, medial sacral artery, inferior vesical artery.
It Descends to opposite the ischial spine it turns anteromedially to reach the base of the bladder in the broad ligament. On the pelvic floor, the ureter pierces Mackenrodt´s ligament where the ureteric canal is developed. It is here that the uterine artery crosses the ureter, below it is related to uterine plexus of veins thus ureter being forked between the vessels. After leaving the ureteric canal it runs medially to pierce the posterior aspect of the bladder, being separated from the cervix by a distance of 2cm.It is here that the ureters get damaged in hysterectomy. The ureter pierces the posterior aspect of the bladder and runs obliquely through its wall for a distance of 1.5 cm before terminating at the ureteric orifice. Its vascular supply is from common, internal and external arteries, uterine artery and inferior vesical artery.
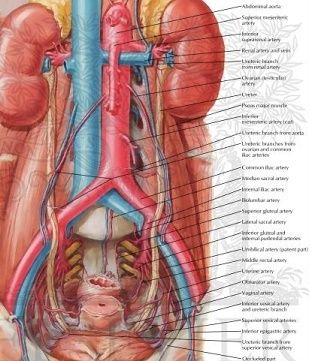
Pararectal space: It is a triangular space, with the base of the cardinal ligament representing the anterior border, the medial border is the ureter and the lateral border is the internal iliac artery. It is important to dissect this space for uterine artery ligation.
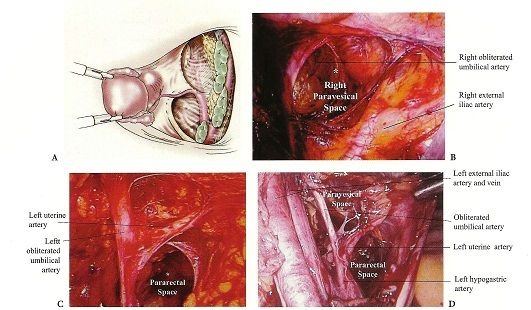
Paravesical space: Laterally, the retropubic space is contiguous with the paravesical spaces, their point of separation being the medial umbilical ligaments (obliterated umbilical arteries). The paired paravesical space is bounded laterally by the obturator internus muscle and the obturator nerve, artery and vein. The posterior border is the endopelvic fascial sheath around the internal iliac artery and vein and its anterior branches, the pubo cervical fascia forms the floor.
Technique: ⁴Patient is evaluated for co morbid diseases, patient is encouraged to hydrate on clear liquids the day before surgery, fleet phospho soda 3oz divided in 2 doses is given at 3:00 and 7:00 p.m.
⁵After anesthesia patient is positioned in low lithotomy position, the arms are placed beside the patient to minimize the risk of brachial plexus during steep trendelenburg position , arms abduction never >90degree , hip flexion at 60-170 degree ,knee flexion 90-120degree ,hip abduction <90 degree , minimal external hip rotation.
⁶Insertion of the uterine manipulator: uterine manipulator is useful in gynecological surgeries, especially in ligating the uterine artery during hysterectomy.
1. Its raises the uterus and brings it closer to the laparoscopic surgical instruments thus facilitating the procedure.
2. By pushing the manipulator cephalad it Stretches the side being operated upon thus increases the distance between the bladder, ureters and the rectum and thereby reducing the chance of injury.
3. Facilitates identification of the utero-vesical peritoneum, the cul-de-sac, and the vaginal cuff just below the cervical attachment, maintains the pneumoperitoneum following culpotomy.
⁷Abdominal entry and trocar placement
⁷Veress needle is inserted normally infraumbilically or transumblically. Supraumblically in case of large uterus. Palmar point in case of previous surgeries. Gas tubing can be connected to the needle to reduce intra abdominal manipulation and also to check negative pressure reading on the insufflators.
As intraperitoneal pressure increase above 15 mm trocar is placed. Then 30-degree scope is introduced and whole abdomen should be evaluated for any injury during insertion and to look for the actual pathology. Under vision three other ports are inserted. Two left lower quadrant ports, 1 left lower quadrant 5mm trocar is inserted 2cm medial and above the anterior superior iliac spine another 5mm or 10 mm port is placed 5-7cm lateral to the umbilicus. Another 5mm port on the right side opposite of the left sided 10mm port. The uterine manipulator is pushed strongly on to the contra lateral side, utero ovarian ligament followed by fallopian and lastly round ligament are dissected step wise followed by uterine artery is ligated.
Uterine artery ligation can be done in 4 ways
CONVENTIONAL APPROACH OR MEDIAL APPROACH:
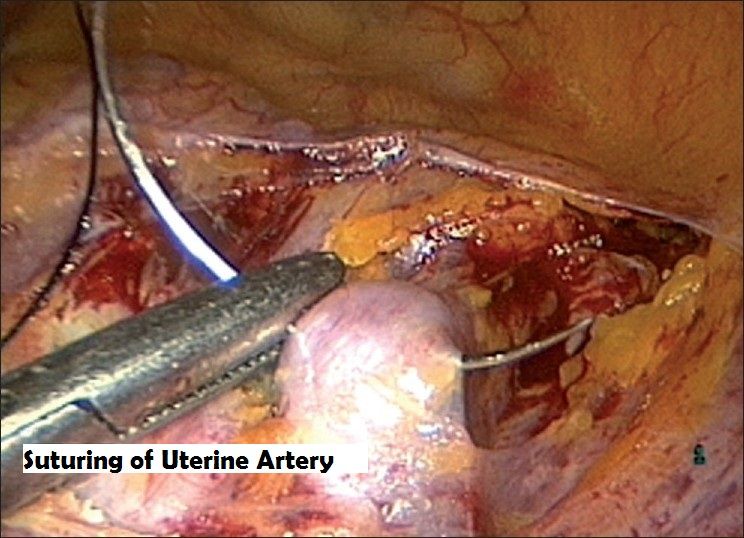
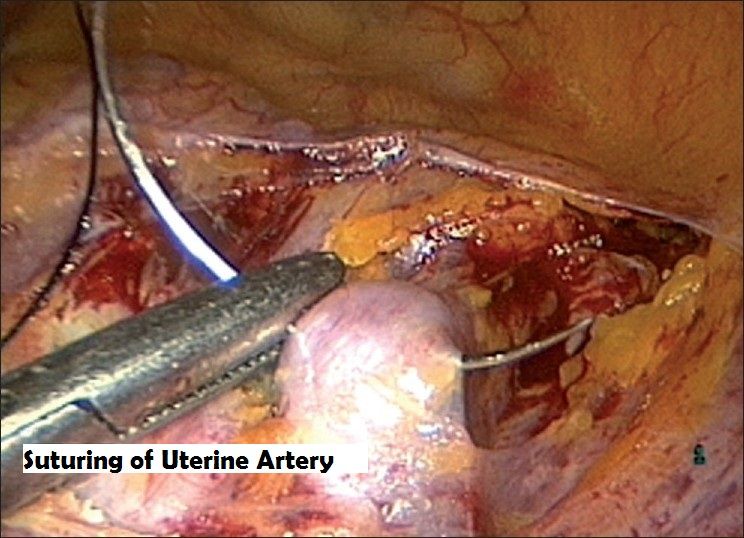
⁸´⁹´¹⁰The anterior leaf of the broad ligament is incised and vesicovaginal peritoneum is opened. Then the posterior layer of the broad ligament is dissected exposing the uterine artery. Skeletonize the uterine artery now pushing the uterine manipulator cephalad in doing so the ureters fall away from the uterine vessels. The suture is taken around the artery at the level of internal cervical os where it gives cervical branch a surgical knot is placed and tightly secured at this level, then the ascending branch is coagulated with bipolar taking care the bipolar instrument touches the fringe of the cup of the uterine manipulator, then tissue is cut give medial to the pedicle this makes the pedicle fall out laterally, thereby it gives space over the fringe of the cup for colpotomy, there by separating the uterus from vagina.
ANTERIOR APPROACH (ascending branch):
⁹Ligation of the ascending branch of uterine artery without opening the posterior peritoneum.
This approach is good for uterus with large fibroid, posterior uterine wall fibroid with poor access to culdesac and posterior broad ligament fibroid. Not so good for patients with fibrosis in parametrium from endometriosis or dense bladder adhesions from c-section.
Uterine artery is first ligated prior to hysterectomy in case of very large fibroid. UV fold of peritoneum is identified and opened from round ligament, the bladder is dissected down completely so that uterine arteries are seen clearly. A window is created in the broad ligament to visualize the posterior surface so that accidentally the bowels are not taken up in the suture. The uterine vessel is identified and ligated.
¹¹Anterior approach by Aust Thomas etal: The anterior leaf of broad ligament is opened and the uterine artery is ligated lateral to its crossing over the ureter.
POSTERIOR APPROACH:¹²Ligation of ascending branch of uterine artery prior to bladder mobilization. Once the blood vessels are secured blood loss from adhesiolysis is minimized making the procedure simpler to perform and less time consuming. Excellent in patients with extensive and dense uterine adhesions to the bladder and anterior abdominal wall.
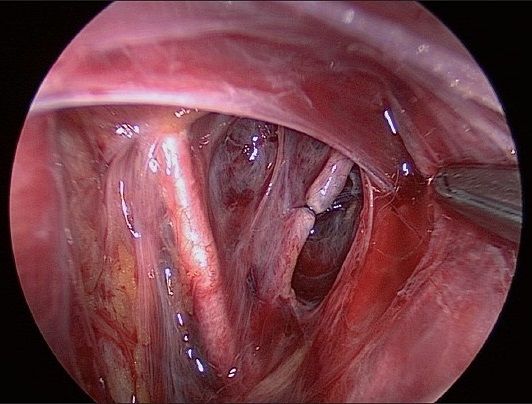
¹⁰´¹³´¹⁴LATERAL APPROACH: (Opening the retroperitoneal space) Commonly done in radical hysterectomy for cervical cancer, good for retroperitoneal fibrosis in the parametrium seen in severe endometriosis, large fibroid uterus may be difficult to visualize without angled scope in broad fibroid of uterus.
¹⁵Gate way to the retroperitoneum: line of dissection between the round ligament and the fallopian tube, and the retroperitoneal space is exfoliated using the non traumatic forceps, internal iliac artery is seen and uterine artery is identified and ligated at its origin. Retro peritoneal approach (Orady etal 2012) The line of dissection in the triangle, the round ligament anteriorly, infundibulopelvic ligament medially and pelvic side walls laterally. Para rectal space developed between the ureter and the hypogastric artery. The first medial branch of the hypogastric artery is the uterine artery. Identification of uterine artery is also done by retro grade approach retrograde tracking of the umbilical ligament. The window below the uterine artery to be opened by endo retractor and the uterine artery is ligated.
¹⁶The uterine artery can be ligated by with extracorporeal knot or by intracorporeal knot. When extracorporeal knots are applied two 10 mm trocars are required, Mishras knot, western knot, Tayside knot can be applied This knots does not over ride the other and no slippage . For intracorporeal knots surgical knots can be applied. In few cases just extracorporeal knot can be done and no need to resect the artery.
After ligating the uterine artery next, surgery can be proceeded for dissecting cervicovaginal attachments and circumferential culdotomy.
¹⁷´¹⁸Circumferential culdotomy: The cardinals ligaments are on each side are divided. Identify the anterior cervico vaginal junction at the lateral fornices, the incision is given over the fringe of the cup of uterine manipulator to complete the circumferential culdotomy . Bipolar forceps are used to coagulate the uterosacral ligament and is valuable to control bleeding from vagina branches.
¹⁹´²⁰Laparoscopic vaginal wall closure: The vaginal delineator (or) a sponge in glove is placed into the vagina for closure of the vaginal cuff, occluding to maintain the pneumoperitoneum. The uterosacral ligament is identified by bipolar desiccation markings. Anterior and the posterior vaginal wall are approximated by extracorporeal are intracorporeal suturing. Peritoneum is not closed.
⁸Cystoscopy: 10 min after IV injection 1amp of indigocaramine dye. Blue dye should be visualized through both the ureteral orifice
The bladder wall should be inspected for suture and thermal injuries; under water examination is used to detect bleeding from the vessels. The peritoneal cavity is vigorously irrigated and suctioned out. Any further bleeding is controlled under water using micro bipolar forceps to coagulate through electrolyte solution, and at least 2liters of RL are left in peritoneal cavity.
DISCUSSION: ¹Laparoscopic hysterectomy is clearly beneficial for patients in whom vaginal hysterectomy is contraindicated (or) cannot be done. When indications for the vaginal approach are equivocal, laparoscopy can be used to determine if vaginal hysterectomy is possible. TLH becomes more advantageous and safe if done with uterine artery ligation. Blood loss is less by this method. The ability to suture laparoscopically greatly enhances the surgeon’s ability to repair visceral injury Average blood loss in abdominal hysterectomy is 400ml while studies had shown in TLH it is much less. ⁹ Rakesh Sinha et al (2009) - 173 women underwent uterine artery ligation prior to hysterectomy, average size of uterus 700grms, average duration of surgery 107min, and the average intraoperative blood loss was 228ml. The data reveals that there is significant decrease in intraoperative blood loss. 9 women underwent blood transfusion where blood loss >750ml, One woman had bladder injury, one had serosal rectal tear, 2 women had delayed complication of ureteric fistula and rectovaginal fistula. Author concluded that large uterus distorts the normal anatomy and there is risk of hemorrhage, injury to ureters, bladder and bowel. These complications are directly or indirectly related to method of securing the vascular pedicles so with adequate training, TLH for large uterus is feasible.
¹¹ThomasAust et al (2O12) performed 38 myomectomy and 28 difficult TLH by anterior approach of laparoscopic uterine artery ligation with one conversion to laparotomy during hysterectomy ,one transfusion after TLH and concluded it is feasible to ligate uterine artery by anterior approach.
Endometriosis, adhesions due to previous surgeries are associated with increased complications the method of uterine artery ligation prior to the hysterectomy increase the success rate of TLH. Ligation of uterine artery at its origin needs to open the retroperitoneum space so any bleeding can be controlled by constant check on the ureters. Studies showed less complication when these procedures are done.
¹⁰J. Donnez etal 2005 In his study group 2596 patients (study period 1995-2000) underwent LAVH, LASH, LH, TLH .1236 underwent TLH there was only one case of conversion to laparotomy, complication rate 1-5%, mean duration of operation was 45min -120 min. Most of the complication in their institution occurred before 1995. In this study group uterine artery was ligated by medial, lateral and posterior approach during laparoscopic hysterectomy and the author concluded that prior ligation of the uterine artery in hysterectomy, duration of the surgery is decreased, the mean blood loss is less, injury to viscera is less and ureteric injuries less than 0.01%.
¹⁶Wen chiung etal (2007) in his study 236 patients underwent LAVH. 23 patients had unexpected extensive pelvic adhesions. In such situations uterine artery preligation was applied through retroperitoneal down steam, ureter tracking was applied to this problem. 17 patients had endometriosis 6 previous LSCS or pelvic infection. Cul de sac was partially and totally obliterated in 10 patients operating time 184 min intraoperative blood loss 146 ml.
²¹Rakesh Sinha etal (2008): In his study 350 women underwent TLH and formed into two groups. In group 175 women underwent TLH with prior bilateral suturing of the uterine arteries. In other Group B of 175 women uterine artery was ligated after cornual pedicles are coagulated the mean duration of the surgery in group A is 60 (20-210) min and group B is 70min(30-190min) and mean blood loss 50(10-2000) ml in group A and group B is 60ml (10-2500).the comparison between the two groups revealed statistically significant difference. Complication like hemorrhage and injury to bladder in group B. The size of the uterus in both the groups is 8-22 wks.
Identifying the uterine artery at its origin and coagulating the vessel during laparoscopic hysterectomy was done by Eugenio and Roman et al both of them showed similar results. These studies show the benefit of identification of the vessel at origin.
¹⁵Retro peritoneal and retrograde total laparoscopic hysterectomy was done by Eugenio Volepi (2014 ) in his study 174 patients 5 cases were exclude d as the size of the uterus was above the umbilicus and rest underwent laparoscopic hysterectomy in community health center ,the uterine artery was identified at its origin and coagulated. The mean operation time was 125min identification of uterine artery 5 min Complication rate was 4.5 % conversion 2.5 % .1.2 % of ureteric injuries.
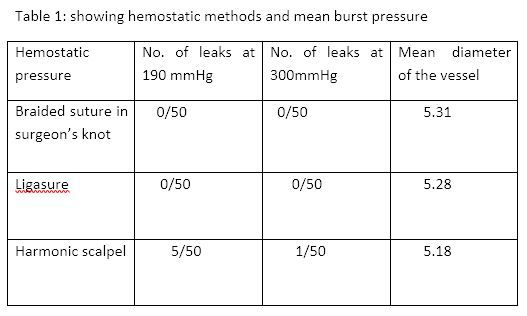
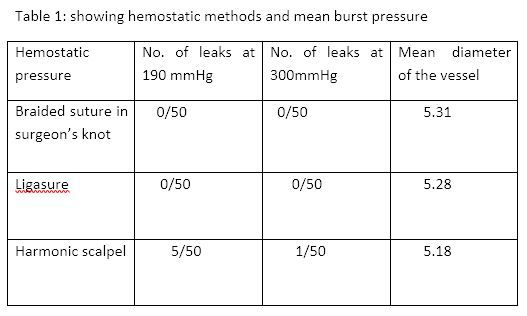
Ligating the uterine artery is better than coagulation because most of the injuries during hysterectomy are due to thermal spread injuries at the level where ureter is crossed by the uterine artery. Thermal spread of bipolar is 6mm.Normally the uterine artery is 2 cm away from the ureter at the level of internal os. In case of pathology like fibroid and adhesion the distance is just 0.5mm. None of the advanced available energy source are ideal for sealing the vessels. The anatomy of uterine artery is varied, in few it is tortures and dilated especially in case of pathology(fibroid). Studies show the energy sources (ligasure) seal the vessel artery upto 7mm and vein up to 12mm, while harmonic scalpel can safely secure hemostasis up to 3mm.So suturing a vessel is the best method of securing the hemostasis . The ability to suture greatly enhance the surgeon´s ability to repair visceral injury.
²³k.Raja babu .N J Barber etal,(2007) in article To knot or not to knot ? sutureless haemostasis compared to the surgeons knot.Table 1 showing .The author concluded that all haemostatic methods when used were success at 190 and 300mmHg when vessel is 5mm ( study done:ligation model devised used fresh ex vivo porcine internal carotid arteries )except harmonic which showed leaks at 190mmHg.
Increased risk of hemorrhage and injury to ureters and bowel with use of Endo GIA stapler. ²⁵(Nezhat etal) instrument failure is 3%²⁴ (B. Patsner )
Laparoscopic hysterectomy has advantage of reduced duration of hospital stay, avoidance of painful large incision, low rate of infection, less intraoperative blood loss. Laparoscopic hysterectomy has less rate of complications when compared to other approach to hysterectomy. MICHEAL et al in his study where 993 underwent AH ,642 VH, AND143 TLH Statistically lower rate of complication in LH9.3. %, AH (15.8%), VH (11. 2%).The ability to suture greatly enhance the surgeon ´s ability to repaired visceral injury.
Most of the complications caused due to uterine artery ligation are injury to ureters in anterior and posterior approach. In lateral approach there may be obturator nerve injury. Ureter injuries are more common at the level where uterine artery crosses the ureters .80% of injuries occur at this site. ²⁶J E ric Jelovsek in retrospective study the incidence of lower urinary tract injury was 4% only 40 % of injuries were identified without using cystoscopy and indigo caramine and so the need of intraoperative cystoscopy in early identifying the injury and repair, thereby preventing morbidity. Gao JS et al in this study from 1999-2005 1286 laparoscopic gynecological surgeries, the incidence of ureteric injuries 0.093%,0.4% in LAVH/TLH 0.01% in non LAVH, most injuries occur with TLH than other lap surgeries.
²⁷Elmera et al in 2012 in their review article found the ureteric injuries in LH 1-2%. The injuries can be decreased properly skeletonizing the uterine artery, pushing the UV fold of peritoneum down to 2.5 cm, this ensures the ureters fall apart from the vessel. At the same time maintain the cranial deviation for the uterus by firm pressure over the uterine manipulator, this also pushes ureters away after ligating the uterine, the pedicle is created so it laterises away from the cup. But with experience and improved skills the complications reduce as shown in the study conducted by¹⁰ Donez ureteric injuries were <0.01%.
Most of the surgeons had done cystoscopy after gynecological laparoscopic surgeries. ²⁸Advancing Minimally Invasive Gynecology Worldwide practice report: The guidelines recommend performance of intraoperative cystoscopy in laparoscopy. Most cases and not all can be detected by cystoscopy. Data suggest sensitivity of 80 -90 %. Among the injuries that may be missed are those related to the use of energy based surgical tools that include ultrasound and radiofrequency electricity.
Other benefits of uterine artery. Symptomatic myomas are treated by hysterectomy, laparoscopic myomectomy or hysteroscopic myomectomy. Few patients who wants to preserve the uterus or to preserve fertility laparoscopic myomectomy can be done but in such cases there can be risk of conversion to laparotomy and hysterectomy. Since there is risk of intraoperative blood loss, conversion rate so high in laparoscopic myomectomy other treatment of choice like uterine artery ligation (LUAL) and uterine artery embolization (UAE) have become the method of choice in most of the cases.
²⁹Uterine artery embolization has 2 main complications fertility and pregnancy outcomes as evidence of various studies there is diminished ovarian reserve, increased risk of spontaneous abortion, preterm deliveries PPH (DUE TO PLACENTA ACCRETA) and other complication is pain after the procedure which is confused between post ovarian syndrome and infection.
The embolic agents used in UAE block not only uterine artery but also ovarian vessels, but with selective uterine artery ligation blood supply to uterus is affected while ovarian vascular supply is not affected. So the LUAL theoretically has better advantage over UAE in fertility and pregnancy outcome, there is no complication of secondary infection and post embolization syndrome in LUAL. The interventional radiological society of Europe considered the desire to maintain child bearing to be relative contraindication to UAE.
³⁰Many studies of fertility and pregnancy outcome after uterine artery ligation and internal artery ligation in post-partum hemorrhage are similar to others where uterine artery ligation was not done. There are only few articles on fertility and pregnancy out come after LUAL for symptomatic fibroid. ³¹Ki-Hyun Park etal 2003 evaluated the treatment outcome of UAE and LUAL. The volume of the uteri and the myoma was obtained before the procedure and 3,6 and 12 months after each procedure. Of 40 patients ,23 underwent UAE 17 underwent LUAL. Reduction in size of the uterus was 58.5% in UAE and 56% in LUAL. ³²Abel Helal et al 2010 compared the effectiveness and safety of uterine artery occlusion by laparoscopy and uterine artery embolism .90 patients were followed for 1,3,6,12 months after the procedure .45 patients underwent LUAL ,45 patients underwent UAE, 6patients of LUAL and 5patients of UAE had clinical failures. Bleeding reduction at 12 months was 91% in LUAL and 93% in UAE. Significantly there was more pain with UAE than LUAL.³³Holub Z etal 2008 in prospective study of pregnancy outcome after uterine artery occlusion(LUAO) and UAE .Pregnancies after uterine embolization had a statistically significant higher rate for spontaneous abortion(56%) than did pregnancies after uterine artery occlusion (10%) no significant difference between the groups in preterm deliveries ,(15.3%IN LUAO vs 20 % in UAE) ³⁸Peng –Hui Wang 2008 of 163 patients with symptomatic fibroid 95 underwent LUVO and 68 underwent LUVO +LM pregnancy outcome in both the groups were 58% and 66% .
³⁴Therapeutic benefits of uterine artery ligation is observed in a study where there is discrepancy of uterine leiomyoma and myometrium to hypoxic –induced endoplasmic reticulum stress after uterine occlusion therapy, these stress related molecules are more in the myoma than in the myometrium .ER stress related apoptosis accounts the effect of UAL therapy on myoma which leads to the death of fibroid while maintaining the survival of the uterus itself.
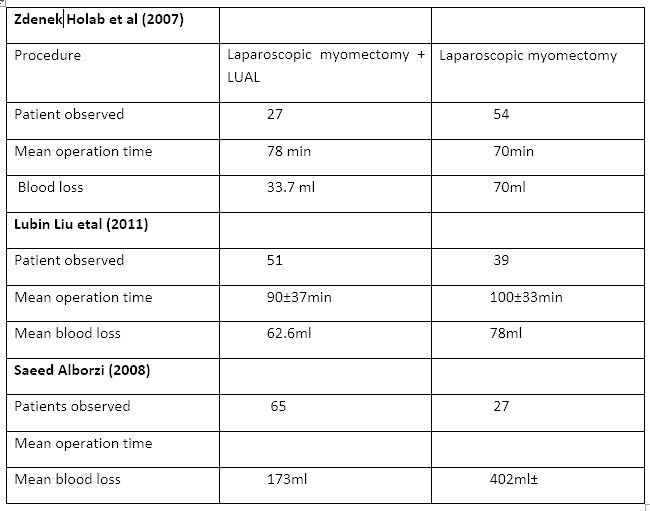
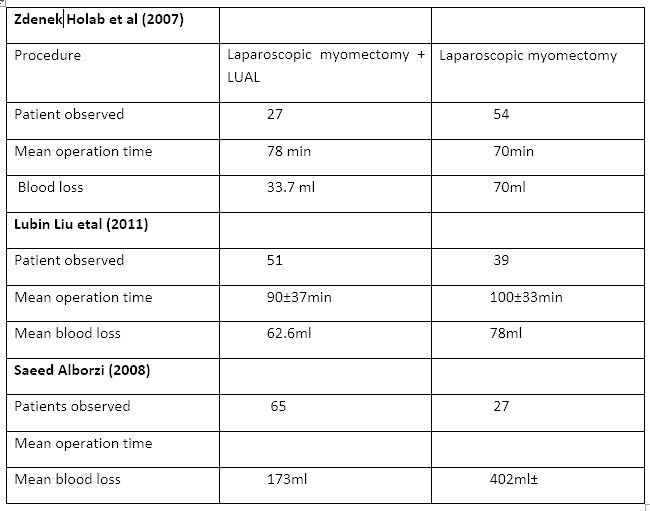
Several studies showed that uterine artery ligation when combined with myomectomy had advantage over only myomectomy with less intraoperative blood loss, the reduced recurrence rate and good response from symptoms. ³⁵Saeed Alborzi 2009 in evaluating the efficiency of laparoscopic uterine artery ligation studied in 152 patients with symptomatic fibroid ,65 patient underwent laparoscopic uterine artery ligation and myomectomy and 27 received LM. A average blood loss was 1 73 ±91 ml for LUAL +LM and 402±131ml for LM only. Recurrence rate is and reported symptom improvement 6.2 % and 98.1% for LUAL+LM and 20.7% and 83.1% respectively in LM. Pregnancy rates were35% in both the groups.
³⁶Zdenek Holab et al 2005 :81 patients 27 patients underwent laparoscopic myomectomy (LM group A) and 54 laparoscopic myomectomy with uterine artery ligation (LM with UAL group B). Mean operating time was 70 min in group A and 78min in group Intraoperative blood loss was 70 ml and 33.9ml
³⁷Lubin Liu et al in 2011 in an observational study 167 patients with symptomatic fibroid, 84 underwent LUAL and LM 83 patient underwent LM. No significant difference was found in the resistance index of the uterine blood flow, the recurrence rate, and the fertility rate between the LUAL + myomectomy and myomectomy alone. There by concluding that LUAL will not affect fertility and pregnancy outcome.
³⁸Ji Hae Bae et al 2011 in non-randomized comparative study recurrence rate with LUAL + LM IS 2% and LM IS 13% and blood loss with the both groups is similar. Mean operation time (LM)100±33and 9o ±39min, (LUAL+LM) blood loss 72.3ml±109mland 62±77.2ml(LUAL+LM).
Table 2: Comparison between uterine artery ligation and laparoscopic myomectomy with laparoscopic myomectomy.
Cervical myomas distort the anatomy displacing the ureters technically it is difficult to do myomectomy or hysterectomy and there is also risk of hemorrhage, injury to bowel, bladder and ureter. Uterine artery ligation in cervical fibroid ³⁹ Rakesh Sinha et al in comparative analysis included 12 patients with cervical myoma who underwent uterine artery ligation plus myomectomy and 12 patients underwent myomectomy without LUAL. Median weight of uterus 200grms-500grms, duration of surgery 60-120 min, morcellation time 15-40 min. total blood loss 100ml. only one patient received 2 units of blood postoperatively. Of 12 patients 6 had delivered vaginally and 6 had cesarean section.
The author concluded that since cervix receives blood both from ascending and descending branch of the uterine arteries, bilateral uterine artery ligation at the origin from the internal iliac artery is feasible and safe in expert hands in well equipped and established surgical setting.
Another advantage of uterine artery ligation in laparoscopic myomectomy is in situ morcellation, with this procedure a large fibroid can be removed by morcellation with fibroid still attached to uterus, where enucleation would be difficult and at times complicated by excess blood loss .Wen –Chun Chang etal 2011 in a prospective 106 with symptomatic fibroid underwent LUAL ,51 LUAL + myomectomy (enucleation) and 55 patients underwent LUAL+ myomectomy with insitu morcellation (in this study group the size of the fibroid is larger).the two groups were followed for three years ,the patients were followed at 6 12,18,24 and 36 months of the surgery. Blood loss between the groups 80-63ml vs 82-122ml.2 patients had excessive blood loss. Pregnancy and live birth rates were 76.5 and 92.4%. Recurrence rate for both groups 9.8%, symptoms improvement >90% after 3 years of follow-up in both the groups.
In the review article by the Rakesh sinha etal laparoscopic myomectomy with uterine artery ligation is technically feasible, it considerably reduces blood loss during myomectomy it also shrinks the small fibroids and prevents the recurrence of the fibroid.
Zdenek Holab etel 2005 :81 patients 27 patients underwent laparoscopic myomectomy (LM –group A) and 54 laparoscopic myomectomies with uterine artery ligation (LM with UAL –group B). Mean operating time was 70 min in group A and 78min in group B, intraoperative blood loss 70 ml and 33.9ml respectively.
There are studies where the uterine artery occlusion was done for symptomatic fibroid. Mehmet Simsek etal laparoscopic uterine artery occlusion for myoma was done in 21 patients and they are followed by ultrasound and MRI for determining the uterine volume.The mean reduction in volume 195 cm3 ,average intraoperative blood loss 65.6 dl ,57% reduction in symptoms. No patient had any complication. Peng –Hui Wang 2008 of 163 patients with symptomatic fibroid 95 underwent LUVO and 68 underwent LUVO +LM pregnancy outcome in both the groups were 58% and 66%.
Fertility and pregnancy outcomes after uterine artery occlusion in review article by ⁴⁰Chang KM etal 2012 concluded that conception and term pregnancy are possible after these procedures but evidence on whether risks of abortion and preterm birth have been increasing simultaneously remains inconclusive.
Conclusion: The success rate of laparoscopic hysterectomy increases when the uterine artery is ligated, this is true in cases where there are extensive adhesions, large fibroid, cervical fibroid, broad ligament fibroid.
Uterine artery ligation can be beneficial in symptomatic fibroids. Either it can be associated with laparoscopic myomectomy or just laparoscopic uterine artery ligation for management of the symptomatic fibroid. It shrinks the size and recurrence of the fibroid.
Where retroperitoneal dissection done routinely for identification of uterine artery at the level of its origin from internal iliac artery ureter is also exposed and there by reduces the chance of accidental injuries.
When uterine artery can be identified and sutured, gynecological laparoscopic surgeries can be done with basic equipment of laparoscopy, where there is lack of advanced energy sources. Volipi etal 2014 had done 174 laparoscopic hysterectomies by coagulating uterine artery at the origin at community level hospital.
Disadvantage of this procedure: After an observation of all the above findings, it can be said that the procedure needs skill and experience of the surgeon undertaking the procedure. All the anticipated advantage of laparoscopy is lost if surgeon ventures beyond the level of his comfort.
REFERENCES
1.Cochrane summeries Nieboer TE etal (2010)surgical approach to hysterectomy for benign gynecological diseases.
2.J.Florea Armnta MD ,Arif Iqbal,Alex .Resolution and Magnification of laparoscope :An observation analysis.Associan Mexicade Cirugia Endoscopica vol 5,no:2,104-106.
3.Cem Celik,Remzi Abali,Nicel ,Erson Aksu.Total Laparoscopic Hysterectomy compared with abdominal hysterectomy ;clinical outcomes.Journal of clinical and analytical medicine .pg no2014) ;596) :490-494.
4. Sarah L C ohen,MD, Jon E inarsson,MD .The role of mechanical bowel preparation in gynecological laparoscopy.obstetrics gynecology 2011 , 4 (1) , 28-31.
5. J. Cory Barnett ,MD,William W .Hurd, MD, Robert M,Roger Jr ,MD. Laparoscopic positioning and nerve injuries .The journal of minimally invasive gynecology ,2007 ,14 664-672
6. Gamal H Eltabbakh ,MD ,uterine manipulation in laparoscopic hysterectomy ,The Female patient ,vol 35, 2010.
7. George A Vilos MD, Arthin Ternamian , Jeffrey Dempster . Laparoscopic entry :A review of techniques, technologies and complications. JOGC 2007 vol 193: pg 433-444.
8. Jon l E nersson MD ,Yoko Suzuki, The laparoscopic hysterectomy : 10 steps toward a successful procedure ,obstetrics and gynecology (2009 ),291 ,57 -64.
9.Rakesh sinha, meenakhi sundarum , smitha lokhathia, Chaitali mahajan.Total laparoscopic hysterectomy for large uterus ,journal gynecological endoscopic surgeons ,vol.1(1) 34-39.
10. J D onnez , p. Ja doul, O. Donnez , J. Squifflet.What is the pref erred route for hysterectomy ? –proposition : most uteri can be removed by laparoscopy.comtecmed .com
11. Thomas Aust MB, MD, MRCOG , Lionel Reftmann , David Rosen ,Gregory Cario, Anterior approach to laparoscopic, uterine artery ligation ,journal of minimally invasive gynecology 2011 VOL 18(6), 792(4).
12. Chamsy DJ,Lee, Posterir approach to uterine artery ligation for anterior cul-de sac obliteration ,Abstracts / journal of minimally invasive gynecology 19 (2012)s31 –S35.
13.Rakesh sinha ,Meenakshi Sundaram,Chaitali Mahajan, Shwetaraje,Laparoscopic myomectomy with uterine artery ligation : review article and comparative analysis journal of gynecological endoscopic surgery ,(2011) 2 (1):3-10.
14. Rakesh sinha ,MD,Meenakshi Sundaram, MD, smitha ,aparna ,instruments and technique cervical myomectomy with uterine artery ligation at its origin, The journal of minimally invasive gynecology,2009 vol,16, No 5 602 -608.
15. Eugenio Volpi ,Luca Bernardini, Maira Angelonia, Retro peritoneal and retrograde total laparoscopic hysterectomyas a standerd treatment in a community hospital.European journal of obstetrics and gynecology and reproductive biology 172, (2014)97-101.
16. Wen –Chun Chang, Li-Yun , Daw –yuan Chang , simultaneous laparoscopic uterine artey ligation and laparoscopic myomectomy for symptomatic uterine myoma with and without insitu morcellation , Human reproduction vol 26, issue 7 1735-1740.
17. Marc L winter MD ,Suan A Mendelshon MD ,Total laparoscopic hysterectomy using the harmonic scalpel , journal of society of the laparoendoscopic surgeons 1999, 3 : 185-186.
18. Ib rahim Alka tout MD, liselotte Mettler , goentji , Gunter Noe, laparoscopic hysterectomy and prolapse : A multiprocedural concept. Journal of society of laparoendoscopic surgeons 2014 18 : 89 -101.
19. Micheal K Hohl, Nik Hauser . Safe tatal intrafascial laparoscopic hysterectomy a prospective cohort study . gynecological surgery 2010 7 ; 231-239.
20.. S .P. Putambeker , G.N Wagh, S S Putambeker , G.n. Wagh, S.S. Putambeker ,M.A kulkerni .A novel technique of total laparoscopic hysterectomy for routine use : evaluation of 140 cases , international journal of biomedical science 2008 ,vol 4 .no;1 38-42.
21.Rakesh sinha ,Meenakshi Sundarum , Yogesh A. Nikam, Chaitali Mahajan.Total laparoscopic hysterectomy with earlier uterine artery ligation.Journal of minimally invasive gynecology.(2008) vol.15;3:354-359
22. Horace Roman, MD, Joel Zanati MD , Ludovic friederich,MD,Laparoscopic hysterectomy of large uteri with uterine artey coagulation at its origin ,journal of the society of laparoendoscopic surgeons 2008 ,jan –mar,12(1):25-29.
23.K.RajaBabu .N.J.BARBER and G H Muir.To knot or not to knot?sutureless haemostasis compared to the surgeons knot. Am R SurgEngl.2007 ,89(4):359-362.
24.B Patsner ,Radical abdominal hysterectomy using the EndoGIA stapler.European journal of gynecological oncology 1998,19(3):215-219.
25.Nezhat etal Injuries Associated with the use of a linear stapler during operative laparoscopy:review of diagnosis,management, and prevention.Journal of gynecologic surgery.vol.9;issue 3:page 145-150.
26. J. Eric jolosek. MD Chiung Chiu , Grace Chen,. Incidence of lower urinary tract injury at the time of total laparoscopic hysterectomy . journal of society of lapaendoscopic surgeons 2007 ,11: 422-427.
27. Elmira Manoucheri, MD, Sarah L cohen , MD , ureteral injuriy in laparoscopic gynecologic surgery Obstetrics and gynecology 2012 ; 592) : 106 -111.
28 AAGL (advancing minimally invasive ,gynecology world wide)AAGL practice report : practice guidelines for intraoperative cystoscopy in laparoscopic hysterectomy.The journal of iminimally invasive gynecology, special article vol 19(4),2012, 401..
29. Hehenkamp WJ1, Volkers NA, Broekmans FJ, de Jong FH, Themmen AP, Birnie E, Reekers JA, Ankum WM Loss of ovarian reserve after uterine artery embolization: a randomized comparison with hysterectomy Hum Reprod. 2007 Jul;22(7):1996-2005.
30. Loic Sentihes, Caroline Tricot,Benoit resch, Fabrice Sergent, Fertility and pregnancy outcomes following uterine devascularization for severe post partum haemorrage,Human Reproduction vol.23,No.5,pp,1087-1092,2008.
31. K I-Hyun Park, Jeong- Yeon Kim, Jong –Seung Shin, Treatment outcomes of UAE and LUAL for uterine myoma , Yonsei medical journal ,vol.444 ($) , 694-702.
32. A del Helal ,MD, Abd El Mageed Mashaly MD,Uterine artery occlusion for symptomatic uterine mysoma ,journal of society of laparoendoscopic surgeons(2010)14: 386-390.
33. Holub Z, Mara M ,kuzel D Jobar A Pregnancy outcomes after uterine artey occlution : prospective multicentric study ,fertility and sterility vol 90(50 2007 Dec pg 1886-91
34. Yan Xie, Xiang Tao, Zhongping, Qiyu Guan,Yu Zhu.Discrepancy of uterine leiomyoma and myometrium to hypoxia-induced endoplasmic reticulum stress after uterine occlution therapy accounts for therapeutic effect.Archieves of gynecology and obstetrics ,2014,vol.289,(5) 1039-1045.
35. Saeed AlborziMD, Elmira GhannadanMD ,Soroosh Alborzi,A comparison of combined laparoscopic uterine artey ligation and mtomectomy vs laparoscopic myomectomy in treatment of symptomatic fibroid . Fertility and sterility ,vol92, issue 2 page 742 -747 ,Aug 2009.
36. Zdenek Holub,MD, Michal maraMD phD, David Kuzel MD ,phD, Pregnancy outcome and uterine artey occlution prosective multicentric study . Fertility And Sterility ,vol 90, issue 5 ,Nov -2008 1886-1891.
37. Lubin Liu, Yayan Li md , Yong Chen, laparoscopic transient uterine artery occlution and myomectomy for symptomatic uterine myoma ,Fertility and sterility, vol 95, (1) jan 2011 :254-258.
38. Peng –Hui Wang 2008 of 163 patients with symptomatic fibroid 95 underwent LUVO and 68 underwent LUVO +LM pregnancy outcome in both the groups were 58% and 66% .
39. Rakesh sinha ,Meenakshi Sundaram,Chaitali Mahajan, Shwetaraje,Laparoscopic myomectomy with uterine artery ligation : review article and comparative analysis journal of gynecological endoscopic surgery ,(2011) 2 (1):3-10.
40. Chang KM, Chen MJ, Lee MH, Huang YD,Fertility and pregnancy outcomes after uterine artery occlution with or without myomectomy. Taiwan journal of obsteritics and gynecology 2012 , vol.51,930 :331 -335.
MATERIALS AND METHODS: From literature published in Pub Med, Medline biomedicine data base, obstetrics and gynecology journal, Journal of the society of laparoendoscopic surgeons, Journal of Minimally invasive gynecology, Journal of Minimally invasive surgery, Google images.
RESULTS: Uterine artery being a large vessel with varied anatomy and high pressure artery it is good to ligate the artery during laparoscopic hysterectomy. This technique which resulted in reduced intraoperative blood loss and increases the success rate of laparoscopic surgeries. Laparoscopic uterine artery ligation can also be done in association with laparoscopic myomectomy, or just laparoscopic uterine artery ligation (LUAL) in symptomatic fibroid. Studies show decreased intraoperative bloodloss, reduced recurrence of myoma, and good response from symptoms. Better alternative to uterine artery embolism (UAE) in patients who wants preserve fertility in symptomatic fibroid.
Conclusion: It is feasible to ligate the uterine artery during the laparoscopic hysterectomy and laparoscopic myomectomy. Any complications of the surgery can be minimized without conversion to laparotomy by sufficiently developed suturing technique and knowledge of retroperitoneal anatomy.
¹Hysterectomy is most common gynecologic surgery. The appropriate route to surgery is determined by the type of the pathology expected, anatomical considerations, patient’s preference, surgeons experience and training.
²Laparoscopic approach with appropriate surgical technique has advantages like magnification of anatomy and pathology by 7-10 fold easy access to retroperitoneal space to ligate the uterine artery because of the pneumoperitoneum. Pneumoperitoneum facilitates development of the pelvic spaces, decreases the venous bleeding, there by maintaining a clean operative field while dissecting, access to vagina and rectum and bility to achieve complete hemostasis and clot evacuation.
³Other advantages are avoidance of painful large incision, reduced duration of hospital stays, low rate of infection and ileus and recuperation time. Having many advantages of laparoscopic surgeries, uterine artery ligation increases the success rate of laparoscopic surgery. Total laparoscopic hysterectomy (TLH) includes uterine artery ligation and complete dissection of the uterus from its attachments. Technique and benefits of identifying and ligating the uterine artery in TLH and laparoscopic myomectomy.
Surgeon should know precise anatomy of the pelvis. Uterine artery can be ligated at the origin of the artery, or lateral to where it crosses over the ureter, or just at the level of internal os where uterine artery gives of ascending branch and cervical branch just beside the uterus.
ANATOMY OF UTERINE ARTERY:
Uterine artery is a branch of anterior division of the internal iliac artery. It is the first medial branch of internal iliac artery. It arises below the Obturator artery on the lateral pelvic wall and runs inferomedially into the broad ligament. Umbilical artery also a branch of the anterior division of internal iliac artery is the surgical land mark that leads to the origin of uterine artery and superior vesical artery. It is studied in three segments.
- Parietal segment –up to the ischiatic spine
- Parametrial segment
- Mesometrial segment
In the broad ligament It course is first downwards and forwards until it reaches the parametrium when it turns medially to the level of internal os then it crosses the ureter anteriorly before it branches. It reaches the uterus at the level of cervicouterine junction, it gives one major branch which ascends along the lateral border of the uterus tortuously within the broad ligament until it reaches the region of the ovarian hilum, where it anastomoses with the branch of ovarian artery. Another branch descends to supply the cervix and anastomose with branches of the vaginal artery. These branches are 2-6 mm in diameter. The ascending branch and ovarian arteries anastomose to perfuse the uterus. Arcuate arteries arise from ascending branch, runs transversely within the wall of uterus and radial arteries penetrate deeply into the myometrium. The presence of leiomyomas in the uterus distorts the normal vascular architecture.
Branches of uterine artery - Vesicovaginal artery, Cervico vaginal artery, Sinuous cervical artery, corporeal artery, Vaginal artery and Round ligament artery.
ANATOMY OF URETER: It is 25-30 cm long and has thickened wall and narrow lumen (3mm) continuous with renal shape pelvis extending from pelviureteric junction to bladder. It is a retroperitoneal structure in the posterior abdominal wall and lateral pelvic wall, each ureter descends slightly medially and anterior to psoas major and enters the pelvic cavity where it curves initially laterally and then medially, to open into the base of the bladder. It is narrow at renal pelvis, brim of the lesser pelvis and within wall of urinary bladder.
Abdominal ureter: Passes downwards and medially to lie on the medial edge of the psoas major, at this level, anteriorly the ureter is covered at its origin by the second part of the duodenum and then lies lateral to the inferior vena cava and behind the posterior peritoneum Right ureter is crossed by the ovarian, right colic, and iliocolic vessels. The left ureter is crossed by the ovarian and the left colic vessels. Then enters into the pelvis at the bifurcation of the common iliac artery in front of the sacroiliac joint. Then it enters the true pelvis where it is crossed by the ovarian vessels, behind the mesosigmoid and sigmoid colon.
In the pelvis the ureter lies is anterior to the internal iliac artery it is behind the ovary forming the posterior boundary of the ovarian fossa. Laterally it lies on the fascia of obturator internus progressively crosses to become medial to umbilical, medial sacral artery, inferior vesical artery.
It Descends to opposite the ischial spine it turns anteromedially to reach the base of the bladder in the broad ligament. On the pelvic floor, the ureter pierces Mackenrodt´s ligament where the ureteric canal is developed. It is here that the uterine artery crosses the ureter, below it is related to uterine plexus of veins thus ureter being forked between the vessels. After leaving the ureteric canal it runs medially to pierce the posterior aspect of the bladder, being separated from the cervix by a distance of 2cm.It is here that the ureters get damaged in hysterectomy. The ureter pierces the posterior aspect of the bladder and runs obliquely through its wall for a distance of 1.5 cm before terminating at the ureteric orifice. Its vascular supply is from common, internal and external arteries, uterine artery and inferior vesical artery.
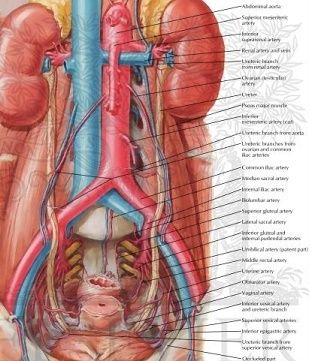
Pararectal space: It is a triangular space, with the base of the cardinal ligament representing the anterior border, the medial border is the ureter and the lateral border is the internal iliac artery. It is important to dissect this space for uterine artery ligation.
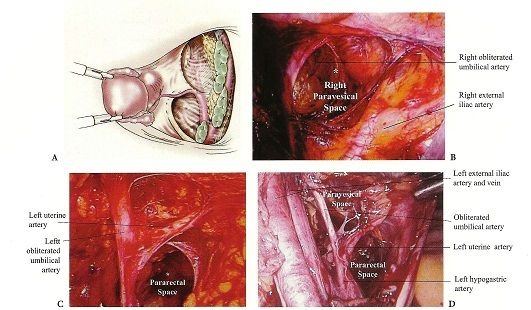
Paravesical space: Laterally, the retropubic space is contiguous with the paravesical spaces, their point of separation being the medial umbilical ligaments (obliterated umbilical arteries). The paired paravesical space is bounded laterally by the obturator internus muscle and the obturator nerve, artery and vein. The posterior border is the endopelvic fascial sheath around the internal iliac artery and vein and its anterior branches, the pubo cervical fascia forms the floor.
Technique: ⁴Patient is evaluated for co morbid diseases, patient is encouraged to hydrate on clear liquids the day before surgery, fleet phospho soda 3oz divided in 2 doses is given at 3:00 and 7:00 p.m.
⁵After anesthesia patient is positioned in low lithotomy position, the arms are placed beside the patient to minimize the risk of brachial plexus during steep trendelenburg position , arms abduction never >90degree , hip flexion at 60-170 degree ,knee flexion 90-120degree ,hip abduction <90 degree , minimal external hip rotation.
⁶Insertion of the uterine manipulator: uterine manipulator is useful in gynecological surgeries, especially in ligating the uterine artery during hysterectomy.
1. Its raises the uterus and brings it closer to the laparoscopic surgical instruments thus facilitating the procedure.
2. By pushing the manipulator cephalad it Stretches the side being operated upon thus increases the distance between the bladder, ureters and the rectum and thereby reducing the chance of injury.
3. Facilitates identification of the utero-vesical peritoneum, the cul-de-sac, and the vaginal cuff just below the cervical attachment, maintains the pneumoperitoneum following culpotomy.
⁷Abdominal entry and trocar placement
⁷Veress needle is inserted normally infraumbilically or transumblically. Supraumblically in case of large uterus. Palmar point in case of previous surgeries. Gas tubing can be connected to the needle to reduce intra abdominal manipulation and also to check negative pressure reading on the insufflators.
As intraperitoneal pressure increase above 15 mm trocar is placed. Then 30-degree scope is introduced and whole abdomen should be evaluated for any injury during insertion and to look for the actual pathology. Under vision three other ports are inserted. Two left lower quadrant ports, 1 left lower quadrant 5mm trocar is inserted 2cm medial and above the anterior superior iliac spine another 5mm or 10 mm port is placed 5-7cm lateral to the umbilicus. Another 5mm port on the right side opposite of the left sided 10mm port. The uterine manipulator is pushed strongly on to the contra lateral side, utero ovarian ligament followed by fallopian and lastly round ligament are dissected step wise followed by uterine artery is ligated.
Uterine artery ligation can be done in 4 ways
CONVENTIONAL APPROACH OR MEDIAL APPROACH:
⁸´⁹´¹⁰The anterior leaf of the broad ligament is incised and vesicovaginal peritoneum is opened. Then the posterior layer of the broad ligament is dissected exposing the uterine artery. Skeletonize the uterine artery now pushing the uterine manipulator cephalad in doing so the ureters fall away from the uterine vessels. The suture is taken around the artery at the level of internal cervical os where it gives cervical branch a surgical knot is placed and tightly secured at this level, then the ascending branch is coagulated with bipolar taking care the bipolar instrument touches the fringe of the cup of the uterine manipulator, then tissue is cut give medial to the pedicle this makes the pedicle fall out laterally, thereby it gives space over the fringe of the cup for colpotomy, there by separating the uterus from vagina.
ANTERIOR APPROACH (ascending branch):
⁹Ligation of the ascending branch of uterine artery without opening the posterior peritoneum.
This approach is good for uterus with large fibroid, posterior uterine wall fibroid with poor access to culdesac and posterior broad ligament fibroid. Not so good for patients with fibrosis in parametrium from endometriosis or dense bladder adhesions from c-section.
Uterine artery is first ligated prior to hysterectomy in case of very large fibroid. UV fold of peritoneum is identified and opened from round ligament, the bladder is dissected down completely so that uterine arteries are seen clearly. A window is created in the broad ligament to visualize the posterior surface so that accidentally the bowels are not taken up in the suture. The uterine vessel is identified and ligated.
¹¹Anterior approach by Aust Thomas etal: The anterior leaf of broad ligament is opened and the uterine artery is ligated lateral to its crossing over the ureter.
POSTERIOR APPROACH:¹²Ligation of ascending branch of uterine artery prior to bladder mobilization. Once the blood vessels are secured blood loss from adhesiolysis is minimized making the procedure simpler to perform and less time consuming. Excellent in patients with extensive and dense uterine adhesions to the bladder and anterior abdominal wall.
¹⁰´¹³´¹⁴LATERAL APPROACH: (Opening the retroperitoneal space) Commonly done in radical hysterectomy for cervical cancer, good for retroperitoneal fibrosis in the parametrium seen in severe endometriosis, large fibroid uterus may be difficult to visualize without angled scope in broad fibroid of uterus.
¹⁵Gate way to the retroperitoneum: line of dissection between the round ligament and the fallopian tube, and the retroperitoneal space is exfoliated using the non traumatic forceps, internal iliac artery is seen and uterine artery is identified and ligated at its origin. Retro peritoneal approach (Orady etal 2012) The line of dissection in the triangle, the round ligament anteriorly, infundibulopelvic ligament medially and pelvic side walls laterally. Para rectal space developed between the ureter and the hypogastric artery. The first medial branch of the hypogastric artery is the uterine artery. Identification of uterine artery is also done by retro grade approach retrograde tracking of the umbilical ligament. The window below the uterine artery to be opened by endo retractor and the uterine artery is ligated.
¹⁶The uterine artery can be ligated by with extracorporeal knot or by intracorporeal knot. When extracorporeal knots are applied two 10 mm trocars are required, Mishras knot, western knot, Tayside knot can be applied This knots does not over ride the other and no slippage . For intracorporeal knots surgical knots can be applied. In few cases just extracorporeal knot can be done and no need to resect the artery.
After ligating the uterine artery next, surgery can be proceeded for dissecting cervicovaginal attachments and circumferential culdotomy.
¹⁷´¹⁸Circumferential culdotomy: The cardinals ligaments are on each side are divided. Identify the anterior cervico vaginal junction at the lateral fornices, the incision is given over the fringe of the cup of uterine manipulator to complete the circumferential culdotomy . Bipolar forceps are used to coagulate the uterosacral ligament and is valuable to control bleeding from vagina branches.
¹⁹´²⁰Laparoscopic vaginal wall closure: The vaginal delineator (or) a sponge in glove is placed into the vagina for closure of the vaginal cuff, occluding to maintain the pneumoperitoneum. The uterosacral ligament is identified by bipolar desiccation markings. Anterior and the posterior vaginal wall are approximated by extracorporeal are intracorporeal suturing. Peritoneum is not closed.
⁸Cystoscopy: 10 min after IV injection 1amp of indigocaramine dye. Blue dye should be visualized through both the ureteral orifice
The bladder wall should be inspected for suture and thermal injuries; under water examination is used to detect bleeding from the vessels. The peritoneal cavity is vigorously irrigated and suctioned out. Any further bleeding is controlled under water using micro bipolar forceps to coagulate through electrolyte solution, and at least 2liters of RL are left in peritoneal cavity.
DISCUSSION: ¹Laparoscopic hysterectomy is clearly beneficial for patients in whom vaginal hysterectomy is contraindicated (or) cannot be done. When indications for the vaginal approach are equivocal, laparoscopy can be used to determine if vaginal hysterectomy is possible. TLH becomes more advantageous and safe if done with uterine artery ligation. Blood loss is less by this method. The ability to suture laparoscopically greatly enhances the surgeon’s ability to repair visceral injury Average blood loss in abdominal hysterectomy is 400ml while studies had shown in TLH it is much less. ⁹ Rakesh Sinha et al (2009) - 173 women underwent uterine artery ligation prior to hysterectomy, average size of uterus 700grms, average duration of surgery 107min, and the average intraoperative blood loss was 228ml. The data reveals that there is significant decrease in intraoperative blood loss. 9 women underwent blood transfusion where blood loss >750ml, One woman had bladder injury, one had serosal rectal tear, 2 women had delayed complication of ureteric fistula and rectovaginal fistula. Author concluded that large uterus distorts the normal anatomy and there is risk of hemorrhage, injury to ureters, bladder and bowel. These complications are directly or indirectly related to method of securing the vascular pedicles so with adequate training, TLH for large uterus is feasible.
¹¹ThomasAust et al (2O12) performed 38 myomectomy and 28 difficult TLH by anterior approach of laparoscopic uterine artery ligation with one conversion to laparotomy during hysterectomy ,one transfusion after TLH and concluded it is feasible to ligate uterine artery by anterior approach.
Endometriosis, adhesions due to previous surgeries are associated with increased complications the method of uterine artery ligation prior to the hysterectomy increase the success rate of TLH. Ligation of uterine artery at its origin needs to open the retroperitoneum space so any bleeding can be controlled by constant check on the ureters. Studies showed less complication when these procedures are done.
¹⁰J. Donnez etal 2005 In his study group 2596 patients (study period 1995-2000) underwent LAVH, LASH, LH, TLH .1236 underwent TLH there was only one case of conversion to laparotomy, complication rate 1-5%, mean duration of operation was 45min -120 min. Most of the complication in their institution occurred before 1995. In this study group uterine artery was ligated by medial, lateral and posterior approach during laparoscopic hysterectomy and the author concluded that prior ligation of the uterine artery in hysterectomy, duration of the surgery is decreased, the mean blood loss is less, injury to viscera is less and ureteric injuries less than 0.01%.
¹⁶Wen chiung etal (2007) in his study 236 patients underwent LAVH. 23 patients had unexpected extensive pelvic adhesions. In such situations uterine artery preligation was applied through retroperitoneal down steam, ureter tracking was applied to this problem. 17 patients had endometriosis 6 previous LSCS or pelvic infection. Cul de sac was partially and totally obliterated in 10 patients operating time 184 min intraoperative blood loss 146 ml.
²¹Rakesh Sinha etal (2008): In his study 350 women underwent TLH and formed into two groups. In group 175 women underwent TLH with prior bilateral suturing of the uterine arteries. In other Group B of 175 women uterine artery was ligated after cornual pedicles are coagulated the mean duration of the surgery in group A is 60 (20-210) min and group B is 70min(30-190min) and mean blood loss 50(10-2000) ml in group A and group B is 60ml (10-2500).the comparison between the two groups revealed statistically significant difference. Complication like hemorrhage and injury to bladder in group B. The size of the uterus in both the groups is 8-22 wks.
Identifying the uterine artery at its origin and coagulating the vessel during laparoscopic hysterectomy was done by Eugenio and Roman et al both of them showed similar results. These studies show the benefit of identification of the vessel at origin.
¹⁵Retro peritoneal and retrograde total laparoscopic hysterectomy was done by Eugenio Volepi (2014 ) in his study 174 patients 5 cases were exclude d as the size of the uterus was above the umbilicus and rest underwent laparoscopic hysterectomy in community health center ,the uterine artery was identified at its origin and coagulated. The mean operation time was 125min identification of uterine artery 5 min Complication rate was 4.5 % conversion 2.5 % .1.2 % of ureteric injuries.
Ligating the uterine artery is better than coagulation because most of the injuries during hysterectomy are due to thermal spread injuries at the level where ureter is crossed by the uterine artery. Thermal spread of bipolar is 6mm.Normally the uterine artery is 2 cm away from the ureter at the level of internal os. In case of pathology like fibroid and adhesion the distance is just 0.5mm. None of the advanced available energy source are ideal for sealing the vessels. The anatomy of uterine artery is varied, in few it is tortures and dilated especially in case of pathology(fibroid). Studies show the energy sources (ligasure) seal the vessel artery upto 7mm and vein up to 12mm, while harmonic scalpel can safely secure hemostasis up to 3mm.So suturing a vessel is the best method of securing the hemostasis . The ability to suture greatly enhance the surgeon´s ability to repair visceral injury.
²³k.Raja babu .N J Barber etal,(2007) in article To knot or not to knot ? sutureless haemostasis compared to the surgeons knot.Table 1 showing .The author concluded that all haemostatic methods when used were success at 190 and 300mmHg when vessel is 5mm ( study done:ligation model devised used fresh ex vivo porcine internal carotid arteries )except harmonic which showed leaks at 190mmHg.
Increased risk of hemorrhage and injury to ureters and bowel with use of Endo GIA stapler. ²⁵(Nezhat etal) instrument failure is 3%²⁴ (B. Patsner )
Laparoscopic hysterectomy has advantage of reduced duration of hospital stay, avoidance of painful large incision, low rate of infection, less intraoperative blood loss. Laparoscopic hysterectomy has less rate of complications when compared to other approach to hysterectomy. MICHEAL et al in his study where 993 underwent AH ,642 VH, AND143 TLH Statistically lower rate of complication in LH9.3. %, AH (15.8%), VH (11. 2%).The ability to suture greatly enhance the surgeon ´s ability to repaired visceral injury.
Most of the complications caused due to uterine artery ligation are injury to ureters in anterior and posterior approach. In lateral approach there may be obturator nerve injury. Ureter injuries are more common at the level where uterine artery crosses the ureters .80% of injuries occur at this site. ²⁶J E ric Jelovsek in retrospective study the incidence of lower urinary tract injury was 4% only 40 % of injuries were identified without using cystoscopy and indigo caramine and so the need of intraoperative cystoscopy in early identifying the injury and repair, thereby preventing morbidity. Gao JS et al in this study from 1999-2005 1286 laparoscopic gynecological surgeries, the incidence of ureteric injuries 0.093%,0.4% in LAVH/TLH 0.01% in non LAVH, most injuries occur with TLH than other lap surgeries.
²⁷Elmera et al in 2012 in their review article found the ureteric injuries in LH 1-2%. The injuries can be decreased properly skeletonizing the uterine artery, pushing the UV fold of peritoneum down to 2.5 cm, this ensures the ureters fall apart from the vessel. At the same time maintain the cranial deviation for the uterus by firm pressure over the uterine manipulator, this also pushes ureters away after ligating the uterine, the pedicle is created so it laterises away from the cup. But with experience and improved skills the complications reduce as shown in the study conducted by¹⁰ Donez ureteric injuries were <0.01%.
Most of the surgeons had done cystoscopy after gynecological laparoscopic surgeries. ²⁸Advancing Minimally Invasive Gynecology Worldwide practice report: The guidelines recommend performance of intraoperative cystoscopy in laparoscopy. Most cases and not all can be detected by cystoscopy. Data suggest sensitivity of 80 -90 %. Among the injuries that may be missed are those related to the use of energy based surgical tools that include ultrasound and radiofrequency electricity.
Other benefits of uterine artery. Symptomatic myomas are treated by hysterectomy, laparoscopic myomectomy or hysteroscopic myomectomy. Few patients who wants to preserve the uterus or to preserve fertility laparoscopic myomectomy can be done but in such cases there can be risk of conversion to laparotomy and hysterectomy. Since there is risk of intraoperative blood loss, conversion rate so high in laparoscopic myomectomy other treatment of choice like uterine artery ligation (LUAL) and uterine artery embolization (UAE) have become the method of choice in most of the cases.
²⁹Uterine artery embolization has 2 main complications fertility and pregnancy outcomes as evidence of various studies there is diminished ovarian reserve, increased risk of spontaneous abortion, preterm deliveries PPH (DUE TO PLACENTA ACCRETA) and other complication is pain after the procedure which is confused between post ovarian syndrome and infection.
The embolic agents used in UAE block not only uterine artery but also ovarian vessels, but with selective uterine artery ligation blood supply to uterus is affected while ovarian vascular supply is not affected. So the LUAL theoretically has better advantage over UAE in fertility and pregnancy outcome, there is no complication of secondary infection and post embolization syndrome in LUAL. The interventional radiological society of Europe considered the desire to maintain child bearing to be relative contraindication to UAE.
³⁰Many studies of fertility and pregnancy outcome after uterine artery ligation and internal artery ligation in post-partum hemorrhage are similar to others where uterine artery ligation was not done. There are only few articles on fertility and pregnancy out come after LUAL for symptomatic fibroid. ³¹Ki-Hyun Park etal 2003 evaluated the treatment outcome of UAE and LUAL. The volume of the uteri and the myoma was obtained before the procedure and 3,6 and 12 months after each procedure. Of 40 patients ,23 underwent UAE 17 underwent LUAL. Reduction in size of the uterus was 58.5% in UAE and 56% in LUAL. ³²Abel Helal et al 2010 compared the effectiveness and safety of uterine artery occlusion by laparoscopy and uterine artery embolism .90 patients were followed for 1,3,6,12 months after the procedure .45 patients underwent LUAL ,45 patients underwent UAE, 6patients of LUAL and 5patients of UAE had clinical failures. Bleeding reduction at 12 months was 91% in LUAL and 93% in UAE. Significantly there was more pain with UAE than LUAL.³³Holub Z etal 2008 in prospective study of pregnancy outcome after uterine artery occlusion(LUAO) and UAE .Pregnancies after uterine embolization had a statistically significant higher rate for spontaneous abortion(56%) than did pregnancies after uterine artery occlusion (10%) no significant difference between the groups in preterm deliveries ,(15.3%IN LUAO vs 20 % in UAE) ³⁸Peng –Hui Wang 2008 of 163 patients with symptomatic fibroid 95 underwent LUVO and 68 underwent LUVO +LM pregnancy outcome in both the groups were 58% and 66% .
³⁴Therapeutic benefits of uterine artery ligation is observed in a study where there is discrepancy of uterine leiomyoma and myometrium to hypoxic –induced endoplasmic reticulum stress after uterine occlusion therapy, these stress related molecules are more in the myoma than in the myometrium .ER stress related apoptosis accounts the effect of UAL therapy on myoma which leads to the death of fibroid while maintaining the survival of the uterus itself.
Several studies showed that uterine artery ligation when combined with myomectomy had advantage over only myomectomy with less intraoperative blood loss, the reduced recurrence rate and good response from symptoms. ³⁵Saeed Alborzi 2009 in evaluating the efficiency of laparoscopic uterine artery ligation studied in 152 patients with symptomatic fibroid ,65 patient underwent laparoscopic uterine artery ligation and myomectomy and 27 received LM. A average blood loss was 1 73 ±91 ml for LUAL +LM and 402±131ml for LM only. Recurrence rate is and reported symptom improvement 6.2 % and 98.1% for LUAL+LM and 20.7% and 83.1% respectively in LM. Pregnancy rates were35% in both the groups.
³⁶Zdenek Holab et al 2005 :81 patients 27 patients underwent laparoscopic myomectomy (LM group A) and 54 laparoscopic myomectomy with uterine artery ligation (LM with UAL group B). Mean operating time was 70 min in group A and 78min in group Intraoperative blood loss was 70 ml and 33.9ml
³⁷Lubin Liu et al in 2011 in an observational study 167 patients with symptomatic fibroid, 84 underwent LUAL and LM 83 patient underwent LM. No significant difference was found in the resistance index of the uterine blood flow, the recurrence rate, and the fertility rate between the LUAL + myomectomy and myomectomy alone. There by concluding that LUAL will not affect fertility and pregnancy outcome.
³⁸Ji Hae Bae et al 2011 in non-randomized comparative study recurrence rate with LUAL + LM IS 2% and LM IS 13% and blood loss with the both groups is similar. Mean operation time (LM)100±33and 9o ±39min, (LUAL+LM) blood loss 72.3ml±109mland 62±77.2ml(LUAL+LM).
Table 2: Comparison between uterine artery ligation and laparoscopic myomectomy with laparoscopic myomectomy.
Cervical myomas distort the anatomy displacing the ureters technically it is difficult to do myomectomy or hysterectomy and there is also risk of hemorrhage, injury to bowel, bladder and ureter. Uterine artery ligation in cervical fibroid ³⁹ Rakesh Sinha et al in comparative analysis included 12 patients with cervical myoma who underwent uterine artery ligation plus myomectomy and 12 patients underwent myomectomy without LUAL. Median weight of uterus 200grms-500grms, duration of surgery 60-120 min, morcellation time 15-40 min. total blood loss 100ml. only one patient received 2 units of blood postoperatively. Of 12 patients 6 had delivered vaginally and 6 had cesarean section.
The author concluded that since cervix receives blood both from ascending and descending branch of the uterine arteries, bilateral uterine artery ligation at the origin from the internal iliac artery is feasible and safe in expert hands in well equipped and established surgical setting.
Another advantage of uterine artery ligation in laparoscopic myomectomy is in situ morcellation, with this procedure a large fibroid can be removed by morcellation with fibroid still attached to uterus, where enucleation would be difficult and at times complicated by excess blood loss .Wen –Chun Chang etal 2011 in a prospective 106 with symptomatic fibroid underwent LUAL ,51 LUAL + myomectomy (enucleation) and 55 patients underwent LUAL+ myomectomy with insitu morcellation (in this study group the size of the fibroid is larger).the two groups were followed for three years ,the patients were followed at 6 12,18,24 and 36 months of the surgery. Blood loss between the groups 80-63ml vs 82-122ml.2 patients had excessive blood loss. Pregnancy and live birth rates were 76.5 and 92.4%. Recurrence rate for both groups 9.8%, symptoms improvement >90% after 3 years of follow-up in both the groups.
In the review article by the Rakesh sinha etal laparoscopic myomectomy with uterine artery ligation is technically feasible, it considerably reduces blood loss during myomectomy it also shrinks the small fibroids and prevents the recurrence of the fibroid.
Zdenek Holab etel 2005 :81 patients 27 patients underwent laparoscopic myomectomy (LM –group A) and 54 laparoscopic myomectomies with uterine artery ligation (LM with UAL –group B). Mean operating time was 70 min in group A and 78min in group B, intraoperative blood loss 70 ml and 33.9ml respectively.
There are studies where the uterine artery occlusion was done for symptomatic fibroid. Mehmet Simsek etal laparoscopic uterine artery occlusion for myoma was done in 21 patients and they are followed by ultrasound and MRI for determining the uterine volume.The mean reduction in volume 195 cm3 ,average intraoperative blood loss 65.6 dl ,57% reduction in symptoms. No patient had any complication. Peng –Hui Wang 2008 of 163 patients with symptomatic fibroid 95 underwent LUVO and 68 underwent LUVO +LM pregnancy outcome in both the groups were 58% and 66%.
Fertility and pregnancy outcomes after uterine artery occlusion in review article by ⁴⁰Chang KM etal 2012 concluded that conception and term pregnancy are possible after these procedures but evidence on whether risks of abortion and preterm birth have been increasing simultaneously remains inconclusive.
Conclusion: The success rate of laparoscopic hysterectomy increases when the uterine artery is ligated, this is true in cases where there are extensive adhesions, large fibroid, cervical fibroid, broad ligament fibroid.
Uterine artery ligation can be beneficial in symptomatic fibroids. Either it can be associated with laparoscopic myomectomy or just laparoscopic uterine artery ligation for management of the symptomatic fibroid. It shrinks the size and recurrence of the fibroid.
Where retroperitoneal dissection done routinely for identification of uterine artery at the level of its origin from internal iliac artery ureter is also exposed and there by reduces the chance of accidental injuries.
When uterine artery can be identified and sutured, gynecological laparoscopic surgeries can be done with basic equipment of laparoscopy, where there is lack of advanced energy sources. Volipi etal 2014 had done 174 laparoscopic hysterectomies by coagulating uterine artery at the origin at community level hospital.
Disadvantage of this procedure: After an observation of all the above findings, it can be said that the procedure needs skill and experience of the surgeon undertaking the procedure. All the anticipated advantage of laparoscopy is lost if surgeon ventures beyond the level of his comfort.
REFERENCES
1.Cochrane summeries Nieboer TE etal (2010)surgical approach to hysterectomy for benign gynecological diseases.
2.J.Florea Armnta MD ,Arif Iqbal,Alex .Resolution and Magnification of laparoscope :An observation analysis.Associan Mexicade Cirugia Endoscopica vol 5,no:2,104-106.
3.Cem Celik,Remzi Abali,Nicel ,Erson Aksu.Total Laparoscopic Hysterectomy compared with abdominal hysterectomy ;clinical outcomes.Journal of clinical and analytical medicine .pg no2014) ;596) :490-494.
4. Sarah L C ohen,MD, Jon E inarsson,MD .The role of mechanical bowel preparation in gynecological laparoscopy.obstetrics gynecology 2011 , 4 (1) , 28-31.
5. J. Cory Barnett ,MD,William W .Hurd, MD, Robert M,Roger Jr ,MD. Laparoscopic positioning and nerve injuries .The journal of minimally invasive gynecology ,2007 ,14 664-672
6. Gamal H Eltabbakh ,MD ,uterine manipulation in laparoscopic hysterectomy ,The Female patient ,vol 35, 2010.
7. George A Vilos MD, Arthin Ternamian , Jeffrey Dempster . Laparoscopic entry :A review of techniques, technologies and complications. JOGC 2007 vol 193: pg 433-444.
8. Jon l E nersson MD ,Yoko Suzuki, The laparoscopic hysterectomy : 10 steps toward a successful procedure ,obstetrics and gynecology (2009 ),291 ,57 -64.
9.Rakesh sinha, meenakhi sundarum , smitha lokhathia, Chaitali mahajan.Total laparoscopic hysterectomy for large uterus ,journal gynecological endoscopic surgeons ,vol.1(1) 34-39.
10. J D onnez , p. Ja doul, O. Donnez , J. Squifflet.What is the pref erred route for hysterectomy ? –proposition : most uteri can be removed by laparoscopy.comtecmed .com
11. Thomas Aust MB, MD, MRCOG , Lionel Reftmann , David Rosen ,Gregory Cario, Anterior approach to laparoscopic, uterine artery ligation ,journal of minimally invasive gynecology 2011 VOL 18(6), 792(4).
12. Chamsy DJ,Lee, Posterir approach to uterine artery ligation for anterior cul-de sac obliteration ,Abstracts / journal of minimally invasive gynecology 19 (2012)s31 –S35.
13.Rakesh sinha ,Meenakshi Sundaram,Chaitali Mahajan, Shwetaraje,Laparoscopic myomectomy with uterine artery ligation : review article and comparative analysis journal of gynecological endoscopic surgery ,(2011) 2 (1):3-10.
14. Rakesh sinha ,MD,Meenakshi Sundaram, MD, smitha ,aparna ,instruments and technique cervical myomectomy with uterine artery ligation at its origin, The journal of minimally invasive gynecology,2009 vol,16, No 5 602 -608.
15. Eugenio Volpi ,Luca Bernardini, Maira Angelonia, Retro peritoneal and retrograde total laparoscopic hysterectomyas a standerd treatment in a community hospital.European journal of obstetrics and gynecology and reproductive biology 172, (2014)97-101.
16. Wen –Chun Chang, Li-Yun , Daw –yuan Chang , simultaneous laparoscopic uterine artey ligation and laparoscopic myomectomy for symptomatic uterine myoma with and without insitu morcellation , Human reproduction vol 26, issue 7 1735-1740.
17. Marc L winter MD ,Suan A Mendelshon MD ,Total laparoscopic hysterectomy using the harmonic scalpel , journal of society of the laparoendoscopic surgeons 1999, 3 : 185-186.
18. Ib rahim Alka tout MD, liselotte Mettler , goentji , Gunter Noe, laparoscopic hysterectomy and prolapse : A multiprocedural concept. Journal of society of laparoendoscopic surgeons 2014 18 : 89 -101.
19. Micheal K Hohl, Nik Hauser . Safe tatal intrafascial laparoscopic hysterectomy a prospective cohort study . gynecological surgery 2010 7 ; 231-239.
20.. S .P. Putambeker , G.N Wagh, S S Putambeker , G.n. Wagh, S.S. Putambeker ,M.A kulkerni .A novel technique of total laparoscopic hysterectomy for routine use : evaluation of 140 cases , international journal of biomedical science 2008 ,vol 4 .no;1 38-42.
21.Rakesh sinha ,Meenakshi Sundarum , Yogesh A. Nikam, Chaitali Mahajan.Total laparoscopic hysterectomy with earlier uterine artery ligation.Journal of minimally invasive gynecology.(2008) vol.15;3:354-359
22. Horace Roman, MD, Joel Zanati MD , Ludovic friederich,MD,Laparoscopic hysterectomy of large uteri with uterine artey coagulation at its origin ,journal of the society of laparoendoscopic surgeons 2008 ,jan –mar,12(1):25-29.
23.K.RajaBabu .N.J.BARBER and G H Muir.To knot or not to knot?sutureless haemostasis compared to the surgeons knot. Am R SurgEngl.2007 ,89(4):359-362.
24.B Patsner ,Radical abdominal hysterectomy using the EndoGIA stapler.European journal of gynecological oncology 1998,19(3):215-219.
25.Nezhat etal Injuries Associated with the use of a linear stapler during operative laparoscopy:review of diagnosis,management, and prevention.Journal of gynecologic surgery.vol.9;issue 3:page 145-150.
26. J. Eric jolosek. MD Chiung Chiu , Grace Chen,. Incidence of lower urinary tract injury at the time of total laparoscopic hysterectomy . journal of society of lapaendoscopic surgeons 2007 ,11: 422-427.
27. Elmira Manoucheri, MD, Sarah L cohen , MD , ureteral injuriy in laparoscopic gynecologic surgery Obstetrics and gynecology 2012 ; 592) : 106 -111.
28 AAGL (advancing minimally invasive ,gynecology world wide)AAGL practice report : practice guidelines for intraoperative cystoscopy in laparoscopic hysterectomy.The journal of iminimally invasive gynecology, special article vol 19(4),2012, 401..
29. Hehenkamp WJ1, Volkers NA, Broekmans FJ, de Jong FH, Themmen AP, Birnie E, Reekers JA, Ankum WM Loss of ovarian reserve after uterine artery embolization: a randomized comparison with hysterectomy Hum Reprod. 2007 Jul;22(7):1996-2005.
30. Loic Sentihes, Caroline Tricot,Benoit resch, Fabrice Sergent, Fertility and pregnancy outcomes following uterine devascularization for severe post partum haemorrage,Human Reproduction vol.23,No.5,pp,1087-1092,2008.
31. K I-Hyun Park, Jeong- Yeon Kim, Jong –Seung Shin, Treatment outcomes of UAE and LUAL for uterine myoma , Yonsei medical journal ,vol.444 ($) , 694-702.
32. A del Helal ,MD, Abd El Mageed Mashaly MD,Uterine artery occlusion for symptomatic uterine mysoma ,journal of society of laparoendoscopic surgeons(2010)14: 386-390.
33. Holub Z, Mara M ,kuzel D Jobar A Pregnancy outcomes after uterine artey occlution : prospective multicentric study ,fertility and sterility vol 90(50 2007 Dec pg 1886-91
34. Yan Xie, Xiang Tao, Zhongping, Qiyu Guan,Yu Zhu.Discrepancy of uterine leiomyoma and myometrium to hypoxia-induced endoplasmic reticulum stress after uterine occlution therapy accounts for therapeutic effect.Archieves of gynecology and obstetrics ,2014,vol.289,(5) 1039-1045.
35. Saeed AlborziMD, Elmira GhannadanMD ,Soroosh Alborzi,A comparison of combined laparoscopic uterine artey ligation and mtomectomy vs laparoscopic myomectomy in treatment of symptomatic fibroid . Fertility and sterility ,vol92, issue 2 page 742 -747 ,Aug 2009.
36. Zdenek Holub,MD, Michal maraMD phD, David Kuzel MD ,phD, Pregnancy outcome and uterine artey occlution prosective multicentric study . Fertility And Sterility ,vol 90, issue 5 ,Nov -2008 1886-1891.
37. Lubin Liu, Yayan Li md , Yong Chen, laparoscopic transient uterine artery occlution and myomectomy for symptomatic uterine myoma ,Fertility and sterility, vol 95, (1) jan 2011 :254-258.
38. Peng –Hui Wang 2008 of 163 patients with symptomatic fibroid 95 underwent LUVO and 68 underwent LUVO +LM pregnancy outcome in both the groups were 58% and 66% .
39. Rakesh sinha ,Meenakshi Sundaram,Chaitali Mahajan, Shwetaraje,Laparoscopic myomectomy with uterine artery ligation : review article and comparative analysis journal of gynecological endoscopic surgery ,(2011) 2 (1):3-10.
40. Chang KM, Chen MJ, Lee MH, Huang YD,Fertility and pregnancy outcomes after uterine artery occlution with or without myomectomy. Taiwan journal of obsteritics and gynecology 2012 , vol.51,930 :331 -335.