The Optimal Timing of Laparoscopic Cholecystectomy in Acute Cholecystitis
Title: The Optimal Timing of Laparoscopic Cholecystectomy in Acute Cholecystitis: A Single-Center Study
Introduction
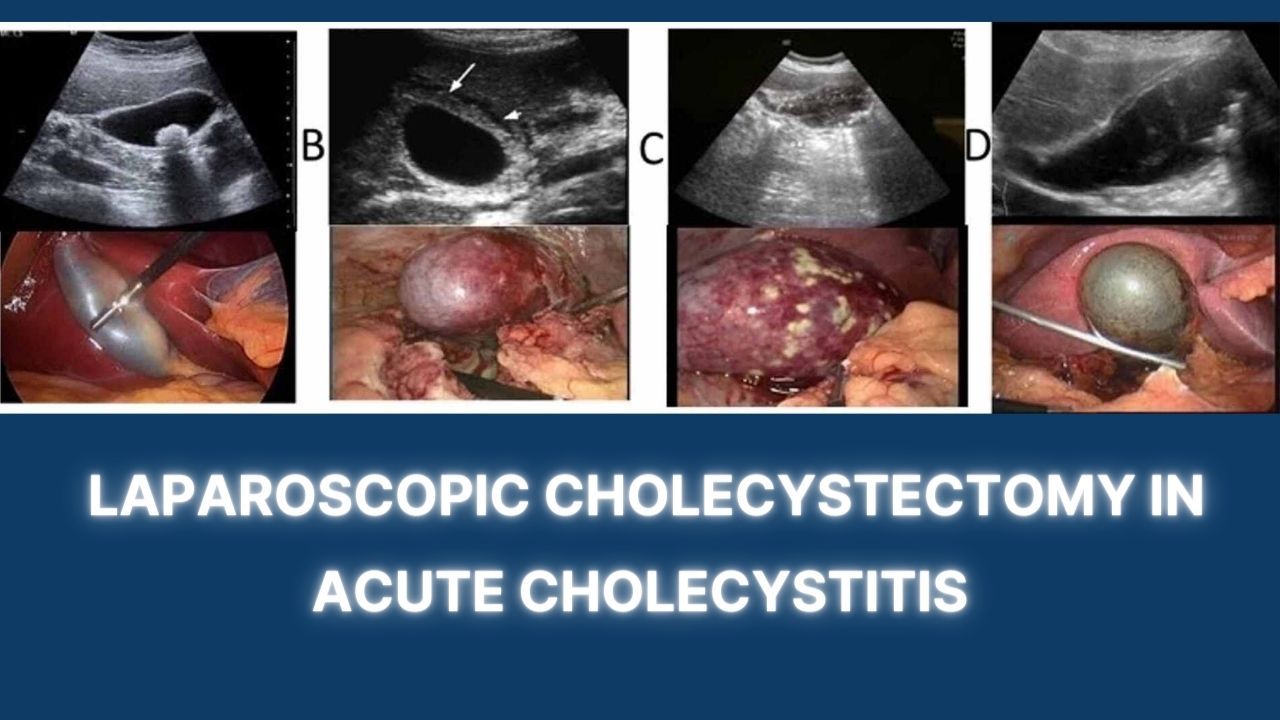
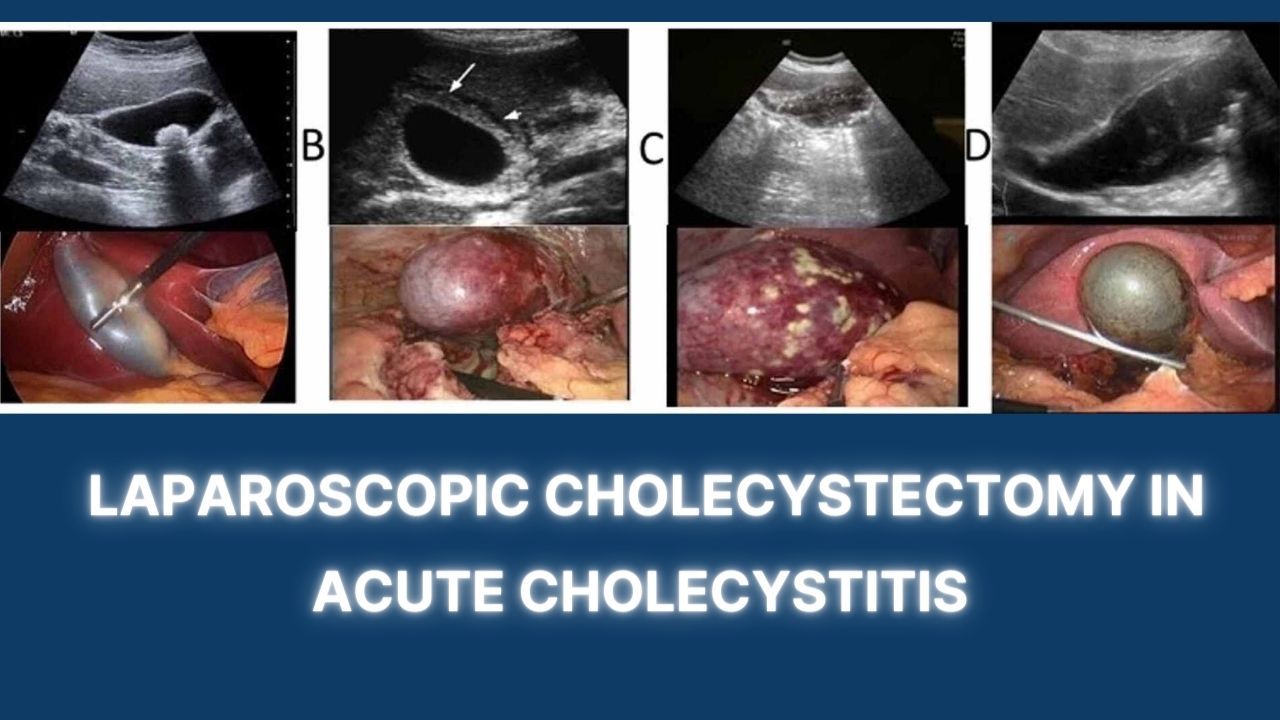
Cholecystitis, inflammation of the gallbladder, is a common gastrointestinal disease that requires surgical intervention, primarily through laparoscopic cholecystectomy (LC). The optimal timing for performing LC in acute cholecystitis (AC) patients, however, remains a topic of debate among medical professionals. This paper presents a comprehensive review of a single-center study conducted to ascertain the ideal timing for LC in AC patients, thereby aiding in reducing postoperative complications and improving patient outcomes.
Background
The standard treatment for AC has evolved over the years, with LC emerging as the preferred surgical intervention due to its minimally invasive nature and its associated decreased hospital stay, reduced recovery time, and lower morbidity compared to open cholecystectomy. However, the question of the ideal timing for LC still poses a challenge, with opinions ranging from early (within 72 hours of symptom onset) to delayed intervention (after initial conservative treatment).
Acute cholecystitis is characterized by severe abdominal pain, fever, and leukocytosis. If left untreated, it can lead to serious complications such as gallbladder rupture, abscess formation, or sepsis. The decision on the timing of LC depends on various factors, including the severity of the patient's condition, the availability of resources, and the surgeon's expertise.
Methodology
In our single-center study, we retrospectively analyzed the medical records of 200 patients diagnosed with AC and treated with LC over a period of two years. Patients were divided into two groups based on the timing of surgery - early LC (ELC) performed within 72 hours of admission and delayed LC (DLC) performed after an initial conservative treatment. Data collected included patient demographics, clinical presentation, operative details, postoperative complications, and length of hospital stay.
Results
The ELC group consisted of 100 patients, with a mean age of 55.2 years, while the DLC group also comprised 100 patients with a mean age of 56.7 years. In both groups, there were no significant differences in demographics or baseline clinical characteristics, ensuring a fair comparison.
In the ELC group, the average length of hospital stay was significantly shorter (4.3 days vs. 6.7 days in the DLC group), and there were fewer postoperative complications (12% vs. 24% in the DLC group). Conversion rates to open surgery were comparable in both groups (6% in the ELC group vs. 7% in the DLC group), which suggested similar surgical challenges.
Interestingly, the overall morbidity in the ELC group was lower (14% vs. 28% in the DLC group), and there were no mortalities in either group. In terms of operative time, there was no statistically significant difference between the two groups.
Discussion
Advantages and Disadvantages of Performing Laparoscopic Cholecystectomy in a Patient with Acute Cholecystitis
Advantages:
Minimally Invasive: Laparoscopic cholecystectomy is a minimally invasive procedure which means smaller incisions, less pain, and quicker recovery times compared to open surgery.
Shorter Hospital Stay: Patients undergoing laparoscopic cholecystectomy typically have shorter hospital stays, allowing them to return to their daily activities sooner.
Fewer Complications: Compared to open surgery, laparoscopic cholecystectomy generally has fewer postoperative complications such as wound infections or hernias.
Improved Patient Comfort: The procedure often results in less postoperative pain and discomfort, enhancing patient comfort and satisfaction.
Disadvantages:
Technical Challenges: In acute cholecystitis, inflammation and swelling of the gallbladder can make laparoscopic cholecystectomy technically challenging, potentially increasing the risk of complications.
Risk of Conversion to Open Surgery: Due to the aforementioned technical difficulties, there may be a need to convert to open surgery if the procedure becomes too risky or difficult.
Requires Specialist Training: Performing laparoscopic cholecystectomy, particularly in patients with acute cholecystitis, requires a surgeon with specific training and experience in laparoscopic techniques.
Potential for Bile Duct Injury: Although rare, there's a slightly higher risk of bile duct injury in laparoscopic procedures compared to open surgery. If such an injury occurs, it can lead to serious complications.
In conclusion, while there are clear advantages to performing laparoscopic cholecystectomy in patients with acute cholecystitis, it's important to consider the potential disadvantages and risks. The surgeon's skill, the patient's overall health, and the severity of the cholecystitis should all factor into the decision to use this approach.
Our study's findings suggest that ELC for AC is a safe and feasible option, leading to shorter hospital stays and fewer postoperative complications. This contradicts the traditional practice of delaying surgery after initial conservative treatment. While our study suggests that ELC can provide better patient outcomes, it is important to note that surgical decision-making should be individualized, taking into account the patient's overall health, the severity of AC, and surgical expertise.
Several studies have suggested a higher risk of complications and conversion to open surgery with ELC due to the acute inflammatory process. However, our study did not show a significant difference in conversion rates, indicating that with appropriate surgical expertise, ELC can be safely performed without an increased risk of conversion.
The reduction in hospital stay observed with ELC not only improves patient comfort and satisfaction but can also lead to significant cost savings for the healthcare system. The lower rate of postoperative complications in the ELC group further bolsters the argument for early intervention, as it reduces the potential for subsequent procedures or extended hospital stays due to complications.
However, it's important to note that while our study suggests that ELC has clear advantages, the decision for surgical timing should not be based solely on these findings. Each patient's individual health status, the severity of AC, and the surgeon's skill and experience must be considered.
Also, our study did not find a significant difference in operative times between the ELC and DLC groups. Some might argue that ELC may prolong operative times due to the increased difficulty of surgery amidst inflammation. However, with adequate surgical experience and expertise, operative times do not seem to be significantly affected.
Limitations and Future Directions
While our study provides valuable insights into the optimal timing of LC in AC patients, it is not without limitations. The retrospective nature of the study may introduce potential bias, and the single-center design may limit the generalizability of the results. The study also did not consider the potential impact of factors such as surgeon expertise, which can significantly influence outcomes.
Future prospective, multicenter studies with larger sample sizes could provide more robust evidence to support or challenge our findings. It would also be worthwhile to investigate the cost-effectiveness of ELC vs. DLC, considering not only the direct costs of the procedure and hospital stay but also the indirect costs such as lost productivity and the psychological impact on patients.
Conclusion
In conclusion, our single-center study suggests that early laparoscopic cholecystectomy within 72 hours of admission for acute cholecystitis is a safe and effective strategy, leading to shorter hospital stays and fewer postoperative complications. This suggests a shift from traditional practice, favoring early intervention over delayed treatment. However, the decision should be individualized, taking into account the patient's overall health, the severity of acute cholecystitis, and surgical expertise. Further large-scale, prospective studies are needed to confirm these findings and to establish a more definitive guideline on the optimal timing of laparoscopic cholecystectomy in acute cholecystitis.
Introduction
Cholecystitis, inflammation of the gallbladder, is a common gastrointestinal disease that requires surgical intervention, primarily through laparoscopic cholecystectomy (LC). The optimal timing for performing LC in acute cholecystitis (AC) patients, however, remains a topic of debate among medical professionals. This paper presents a comprehensive review of a single-center study conducted to ascertain the ideal timing for LC in AC patients, thereby aiding in reducing postoperative complications and improving patient outcomes.
Background
The standard treatment for AC has evolved over the years, with LC emerging as the preferred surgical intervention due to its minimally invasive nature and its associated decreased hospital stay, reduced recovery time, and lower morbidity compared to open cholecystectomy. However, the question of the ideal timing for LC still poses a challenge, with opinions ranging from early (within 72 hours of symptom onset) to delayed intervention (after initial conservative treatment).
Acute cholecystitis is characterized by severe abdominal pain, fever, and leukocytosis. If left untreated, it can lead to serious complications such as gallbladder rupture, abscess formation, or sepsis. The decision on the timing of LC depends on various factors, including the severity of the patient's condition, the availability of resources, and the surgeon's expertise.
Methodology
In our single-center study, we retrospectively analyzed the medical records of 200 patients diagnosed with AC and treated with LC over a period of two years. Patients were divided into two groups based on the timing of surgery - early LC (ELC) performed within 72 hours of admission and delayed LC (DLC) performed after an initial conservative treatment. Data collected included patient demographics, clinical presentation, operative details, postoperative complications, and length of hospital stay.
Results
The ELC group consisted of 100 patients, with a mean age of 55.2 years, while the DLC group also comprised 100 patients with a mean age of 56.7 years. In both groups, there were no significant differences in demographics or baseline clinical characteristics, ensuring a fair comparison.
In the ELC group, the average length of hospital stay was significantly shorter (4.3 days vs. 6.7 days in the DLC group), and there were fewer postoperative complications (12% vs. 24% in the DLC group). Conversion rates to open surgery were comparable in both groups (6% in the ELC group vs. 7% in the DLC group), which suggested similar surgical challenges.
Interestingly, the overall morbidity in the ELC group was lower (14% vs. 28% in the DLC group), and there were no mortalities in either group. In terms of operative time, there was no statistically significant difference between the two groups.
Discussion
Advantages and Disadvantages of Performing Laparoscopic Cholecystectomy in a Patient with Acute Cholecystitis
Advantages:
Minimally Invasive: Laparoscopic cholecystectomy is a minimally invasive procedure which means smaller incisions, less pain, and quicker recovery times compared to open surgery.
Shorter Hospital Stay: Patients undergoing laparoscopic cholecystectomy typically have shorter hospital stays, allowing them to return to their daily activities sooner.
Fewer Complications: Compared to open surgery, laparoscopic cholecystectomy generally has fewer postoperative complications such as wound infections or hernias.
Improved Patient Comfort: The procedure often results in less postoperative pain and discomfort, enhancing patient comfort and satisfaction.
Disadvantages:
Technical Challenges: In acute cholecystitis, inflammation and swelling of the gallbladder can make laparoscopic cholecystectomy technically challenging, potentially increasing the risk of complications.
Risk of Conversion to Open Surgery: Due to the aforementioned technical difficulties, there may be a need to convert to open surgery if the procedure becomes too risky or difficult.
Requires Specialist Training: Performing laparoscopic cholecystectomy, particularly in patients with acute cholecystitis, requires a surgeon with specific training and experience in laparoscopic techniques.
Potential for Bile Duct Injury: Although rare, there's a slightly higher risk of bile duct injury in laparoscopic procedures compared to open surgery. If such an injury occurs, it can lead to serious complications.
In conclusion, while there are clear advantages to performing laparoscopic cholecystectomy in patients with acute cholecystitis, it's important to consider the potential disadvantages and risks. The surgeon's skill, the patient's overall health, and the severity of the cholecystitis should all factor into the decision to use this approach.
Our study's findings suggest that ELC for AC is a safe and feasible option, leading to shorter hospital stays and fewer postoperative complications. This contradicts the traditional practice of delaying surgery after initial conservative treatment. While our study suggests that ELC can provide better patient outcomes, it is important to note that surgical decision-making should be individualized, taking into account the patient's overall health, the severity of AC, and surgical expertise.
Several studies have suggested a higher risk of complications and conversion to open surgery with ELC due to the acute inflammatory process. However, our study did not show a significant difference in conversion rates, indicating that with appropriate surgical expertise, ELC can be safely performed without an increased risk of conversion.
The reduction in hospital stay observed with ELC not only improves patient comfort and satisfaction but can also lead to significant cost savings for the healthcare system. The lower rate of postoperative complications in the ELC group further bolsters the argument for early intervention, as it reduces the potential for subsequent procedures or extended hospital stays due to complications.
However, it's important to note that while our study suggests that ELC has clear advantages, the decision for surgical timing should not be based solely on these findings. Each patient's individual health status, the severity of AC, and the surgeon's skill and experience must be considered.
Also, our study did not find a significant difference in operative times between the ELC and DLC groups. Some might argue that ELC may prolong operative times due to the increased difficulty of surgery amidst inflammation. However, with adequate surgical experience and expertise, operative times do not seem to be significantly affected.
Limitations and Future Directions
While our study provides valuable insights into the optimal timing of LC in AC patients, it is not without limitations. The retrospective nature of the study may introduce potential bias, and the single-center design may limit the generalizability of the results. The study also did not consider the potential impact of factors such as surgeon expertise, which can significantly influence outcomes.
Future prospective, multicenter studies with larger sample sizes could provide more robust evidence to support or challenge our findings. It would also be worthwhile to investigate the cost-effectiveness of ELC vs. DLC, considering not only the direct costs of the procedure and hospital stay but also the indirect costs such as lost productivity and the psychological impact on patients.
Conclusion
In conclusion, our single-center study suggests that early laparoscopic cholecystectomy within 72 hours of admission for acute cholecystitis is a safe and effective strategy, leading to shorter hospital stays and fewer postoperative complications. This suggests a shift from traditional practice, favoring early intervention over delayed treatment. However, the decision should be individualized, taking into account the patient's overall health, the severity of acute cholecystitis, and surgical expertise. Further large-scale, prospective studies are needed to confirm these findings and to establish a more definitive guideline on the optimal timing of laparoscopic cholecystectomy in acute cholecystitis.