Page 33 - WJOLS - Journal of Laparoscopic Surgery
P. 33
Balachandran Premkumar, Subhankar Paul
procedure argue that it is easy to perform and can be used
to protect the esophagus following myotomy. 27
Additionally, it has been suggested that the retro-
esophageal dissection required for a Toupet procedure
may increase the incidence of postoperative dysphagia.
Despite the controversy, laparoscopic Heller’s myotomy
is most often accompanied by an anterior fundoplication.
Laparoscopic Heller’s myotomy with anterior fundo-
plication significantly relieves the symptoms of achalasia
without causing the symptoms of GERD and results in
excellent overall patient satisfaction. 28,29
Laparoscopic Heller-Dor operation has the advantages
of reduced compromise of the cardiopulmonary func-
tion, with less disruption of the supporting structures
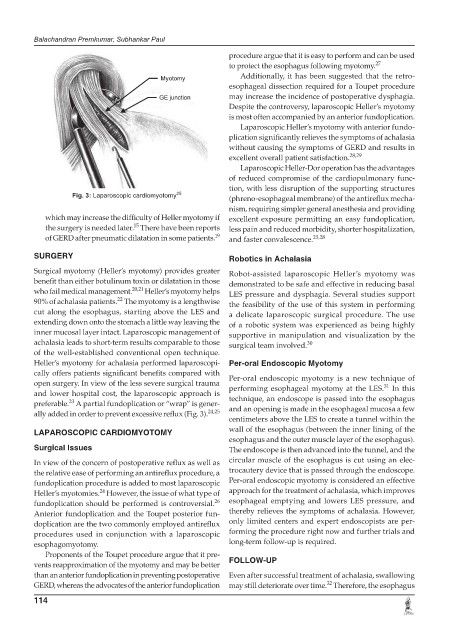
Fig. 3: Laparoscopic cardiomyotomy 25 (phreno-esophageal membrane) of the antireflux mecha-
nism, requiring simpler general anesthesia and providing
which may increase the difficulty of Heller myotomy if excellent exposure permitting an easy fundoplication,
15
the surgery is needed later. There have been reports less pain and reduced morbidity, shorter hospitalization,
of GERD after pneumatic dilatation in some patients. 19 and faster convalescence. 23,28
SURGERY Robotics in Achalasia
Surgical myotomy (Heller’s myotomy) provides greater Robot-assisted laparoscopic Heller’s myotomy was
benefit than either botulinum toxin or dilatation in those demonstrated to be safe and effective in reducing basal
who fail medical management. 20,21 Heller’s myotomy helps LES pressure and dysphagia. Several studies support
22
90% of achalasia patients. The myotomy is a lengthwise the feasibility of the use of this system in performing
cut along the esophagus, starting above the LES and a delicate laparoscopic surgical procedure. The use
extending down onto the stomach a little way leaving the of a robotic system was experienced as being highly
inner mucosal layer intact. Laparoscopic management of supportive in manipulation and visualization by the
achalasia leads to short-term results comparable to those surgical team involved. 30
of the well-established conventional open technique.
Heller’s myotomy for achalasia performed laparoscopi- Per-oral Endoscopic Myotomy
cally offers patients significant benefits compared with Per-oral endoscopic myotomy is a new technique of
open surgery. In view of the less severe surgical trauma 31
and lower hospital cost, the laparoscopic approach is performing esophageal myotomy at the LES. In this
technique, an endoscope is passed into the esophagus
23
preferable. A partial fundoplication or “wrap” is gener-
ally added in order to prevent excessive reflux (Fig. 3). 24,25 and an opening is made in the esophageal mucosa a few
centimeters above the LES to create a tunnel within the
LAPAROSCOPIC CARDIOMYOTOMY wall of the esophagus (between the inner lining of the
esophagus and the outer muscle layer of the esophagus).
Surgical Issues The endoscope is then advanced into the tunnel, and the
In view of the concern of postoperative reflux as well as circular muscle of the esophagus is cut using an elec-
the relative ease of performing an antireflux procedure, a trocautery device that is passed through the endoscope.
fundoplication procedure is added to most laparoscopic Per-oral endoscopic myotomy is considered an effective
24
Heller’s myotomies. However, the issue of what type of approach for the treatment of achalasia, which improves
26
fundoplication should be performed is controversial. esophageal emptying and lowers LES pressure, and
Anterior fundoplication and the Toupet posterior fun- thereby relieves the symptoms of achalasia. However,
doplication are the two commonly employed antireflux only limited centers and expert endoscopists are per-
procedures used in conjunction with a laparoscopic forming the procedure right now and further trials and
esophagomyotomy. long-term follow-up is required.
Proponents of the Toupet procedure argue that it pre-
vents reapproximation of the myotomy and may be better FOLLOW-UP
than an anterior fundoplication in preventing postoperative Even after successful treatment of achalasia, swallowing
32
GERD, whereas the advocates of the anterior fundoplication may still deteriorate over time. Therefore, the esophagus
114