Page 9 - Journal of Laparoscopic Surgery
P. 9
WJOLS
Rising Trend of Laparoscopic Hysterectomy Over Abdominal Hysterectomy: A Comparative Study
through the vagina. The vault was closed vaginally in Peroperative and postoperative complications are
all the cases. Hemostasis was checked and port sites shown in Table 3. Mean duration of hospital stay was
were closed. lesser in group II with mean values of 6.93 ± 2.1 days and
Abdominal hysterectomy was performed according 4.68 ± 1.3 days in group I and group II respectively, with
1
to the technique described by Mattingly and Thompson difference being statistically significant. Postoperative
for benign disease. was also found less in women who underwent TLH. Most
of the patients did not require intravenous analgesics
RESULTS after 2 days of laparoscopic surgery and were comfortably
The demographic profile of patients has been shown in discharged on day 4/5.
Table 1. The mean age of women undergoing TAH and It was found that bladder injury occurred in two cases;
TLH was 46.8 ± 6.3 years and 46.4 ± 7.6 years, respectively. both of them were operated by open technique (TAH).
In 41% of cases with previous surgery, TAH was done In both of these cases, there was history of previous two
while TLH was done with 50% of women with a history caesarean sections and bladder was completely adherent
of prior surgery. No significant difference was found in over the uterus. Bowel injury occurred in two women
demographic profile among two groups. Average BMI was who underwent TAH. No visceral injury was reported
higher in women undergoing TAH than TLH. However, no in group II (TLH).
significant difference was found. Although no significant Among postoperative complications, it has been
difference was found in BMI among the two groups, but observed that postoperative fever and abdominal dis-
after developing good expertise in surgery, the authors tension was found in more number of women who
here started to prefer TLH in women with morbid obesity. underwent TAH. This might be explained on basis of
Indication of surgery is shown in Table 2. It was found more tissue handling and prolonged environmental
that most common indication of hysterectomy was fibroid exposure during open surgery as compare to minimal
uterus in both the groups. However, it was found that in invasive surgery.
women with ovarian cyst, more commonly TAH was per- Stitch line sepsis occurred in seven cases (5.1%), all of
formed. This can be explained on basis of size of ovarian which occur after TAH. No wound sepsis occurred after
cyst, making laparoscopic surgery difficult and secondly TLH showing better wound healing after laparoscopic
could be due to suspicion of malignancy in such cases. surgery.
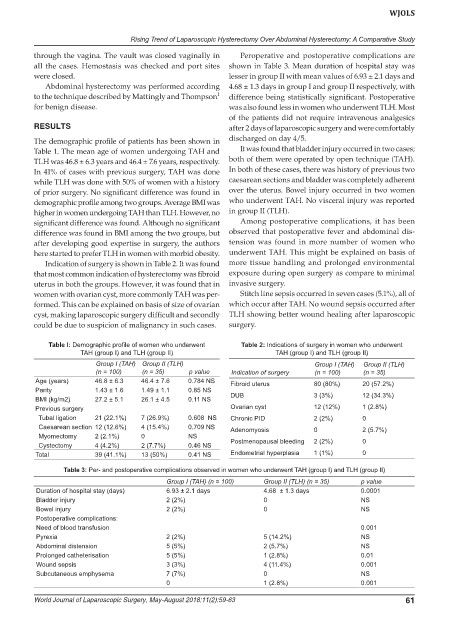
Table I: Demographic profile of women who underwent Table 2: Indications of surgery in women who underwent
TAH (group I) and TLH (group II) TAH (group I) and TLH (group II)
Group I (TAH) Group II (TLH) Group I (TAH) Group II (TLH)
(n = 100) (n = 35) p value Indication of surgery (n = 100) (n = 35)
Age (years) 46.8 ± 6.3 46.4 ± 7.6 0.784 NS Fibroid uterus 80 (80%) 20 (57.2%)
Parity 1.43 ± 1.6 1.49 ± 1.1 0.85 NS
BMI (kg/m2) 27.2 ± 5.1 26.1 ± 4.5 0.11 NS DUB 3 (3%) 12 (34.3%)
Previous surgery Ovarian cyst 12 (12%) 1 (2.8%)
Tubal ligation 21 (22.1%) 7 (26.9%) 0.608 NS Chronic PID 2 (2%) 0
Caesarean section 12 (12.6%) 4 (15.4%) 0.709 NS Adenomyosis 0 2 (5.7%)
Myomectomy 2 (2.1%) 0 NS
Cystectomy 4 (4.2%) 2 (7.7%) 0.46 NS Postmenopausal bleeding 2 (2%) 0
Total 39 (41.1%) 13 (50%) 0.41 NS Endometrial hyperplasia 1 (1%) 0
Table 3: Per- and postoperative complications observed in women who underwent TAH (group I) and TLH (group II)
Group I (TAH) (n = 100) Group II (TLH) (n = 35) p value
Duration of hospital stay (days) 6.93 ± 2.1 days 4.68 ± 1.3 days 0.0001
Bladder injury 2 (2%) 0 NS
Bowel injury 2 (2%) 0 NS
Postoperative complications:
Need of blood transfusion 0.001
Pyrexia 2 (2%) 5 (14.2%) NS
Abdominal distension 5 (5%) 2 (5.7%) NS
Prolonged catheterisation 5 (5%) 1 (2.8%) 0.01
Wound sepsis 3 (3%) 4 (11.4%) 0.001
Subcutaneous emphysema 7 (7%) 0 NS
0 1 (2.8%) 0.001
World Journal of Laparoscopic Surgery, May-August 2018;11(2):59-63 61