Page 46 - World Journal of Laparoscopic Surgery
P. 46
Use of Laparoscopic vs Open Repair for Perforated Peptic Ulcers
Table 4: (Contd...)
Group = “Laparoscopic” Group = “Laparoscopic”
Predictors Odds ratios CI p Odds ratios CI p
Time visit: Nighttime vs Daytime 0.69 0.33–1.41 0.304
Observations 219 219
Tjur’s R 2 0.169 0.128
BMI, body mass index; DBP, diastolic blood; Bold value indicate statistically significant variables
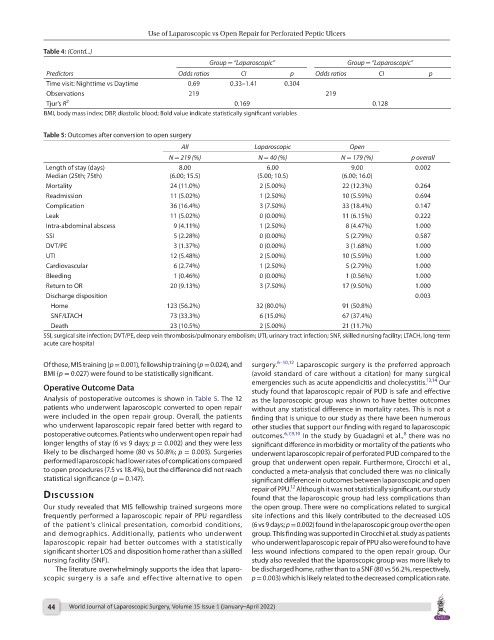
Table 5: Outcomes after conversion to open surgery
All Laparoscopic Open
N = 219 (%) N = 40 (%) N = 179 (%) p overall
Length of stay (days) 8.00 6.00 9.00 0.002
Median (25th; 75th) (6.00; 15.5) (5.00; 10.5) (6.00; 16.0)
Mortality 24 (11.0%) 2 (5.00%) 22 (12.3%) 0.264
Readmission 11 (5.02%) 1 (2.50%) 10 (5.59%) 0.694
Complication 36 (16.4%) 3 (7.50%) 33 (18.4%) 0.147
Leak 11 (5.02%) 0 (0.00%) 11 (6.15%) 0.222
Intra-abdominal abscess 9 (4.11%) 1 (2.50%) 8 (4.47%) 1.000
SSI 5 (2.28%) 0 (0.00%) 5 (2.79%) 0.587
DVT/PE 3 (1.37%) 0 (0.00%) 3 (1.68%) 1.000
UTI 12 (5.48%) 2 (5.00%) 10 (5.59%) 1.000
Cardiovascular 6 (2.74%) 1 (2.50%) 5 (2.79%) 1.000
Bleeding 1 (0.46%) 0 (0.00%) 1 (0.56%) 1.000
Return to OR 20 (9.13%) 3 (7.50%) 17 (9.50%) 1.000
Discharge disposition 0.003
Home 123 (56.2%) 32 (80.0%) 91 (50.8%)
SNF/LTACH 73 (33.3%) 6 (15.0%) 67 (37.4%)
Death 23 (10.5%) 2 (5.00%) 21 (11.7%)
SSI, surgical site infection; DVT/PE, deep vein thrombosis/pulmonary embolism; UTI, urinary tract infection; SNF, skilled nursing facility; LTACH, long-term
acute care hospital
Of these, MIS training (p = 0.001), fellowship training (p = 0.024), and surgery. 6–10,12 Laparoscopic surgery is the preferred approach
BMI (p = 0.027) were found to be statistically significant. (avoid standard of care without a citation) for many surgical
emergencies such as acute appendicitis and cholecystitis. 13,14 Our
Operative Outcome Data study found that laparoscopic repair of PUD is safe and effective
Analysis of postoperative outcomes is shown in Table 5. The 12 as the laparoscopic group was shown to have better outcomes
patients who underwent laparoscopic converted to open repair without any statistical difference in mortality rates. This is not a
were included in the open repair group. Overall, the patients finding that is unique to our study as there have been numerous
who underwent laparoscopic repair fared better with regard to other studies that support our finding with regard to laparoscopic
postoperative outcomes. Patients who underwent open repair had outcomes. 6,7,9,10 In the study by Guadagni et al., there was no
8
longer lengths of stay (6 vs 9 days; p = 0.002) and they were less significant difference in morbidity or mortality of the patients who
likely to be discharged home (80 vs 50.8%; p = 0.003). Surgeries underwent laparoscopic repair of perforated PUD compared to the
performed laparoscopic had lower rates of complications compared group that underwent open repair. Furthermore, Cirocchi et al.,
to open procedures (7.5 vs 18.4%), but the difference did not reach conducted a meta-analysis that concluded there was no clinically
statistical significance (p = 0.147). significant difference in outcomes between laparoscopic and open
12
repair of PPU. Although it was not statistically significant, our study
dIscussIon found that the laparoscopic group had less complications than
Our study revealed that MIS fellowship trained surgeons more the open group. There were no complications related to surgical
frequently performed a laparoscopic repair of PPU regardless site infections and this likely contributed to the decreased LOS
of the patient’s clinical presentation, comorbid conditions, (6 vs 9 days; p = 0.002) found in the laparoscopic group over the open
and demographics. Additionally, patients who underwent group. This finding was supported in Cirocchi et al. study as patients
laparoscopic repair had better outcomes with a statistically who underwent laparoscopic repair of PPU also were found to have
significant shorter LOS and disposition home rather than a skilled less wound infections compared to the open repair group. Our
nursing facility (SNF). study also revealed that the laparoscopic group was more likely to
The literature overwhelmingly supports the idea that laparo- be discharged home, rather than to a SNF (80 vs 56.2%, respectively,
scopic surgery is a safe and effective alternative to open p = 0.003) which is likely related to the decreased complication rate.
44 World Journal of Laparoscopic Surgery, Volume 15 Issue 1 (January–April 2022)