Page 82 - tmp
P. 82
Single-port vs Traditional Laparoscopic Cholecystectomy
instruments through a single access device via an opening in the
umbilicus. The latest devices that are available let the surgeon to
insert more than two instruments and an optic with or without
trocars through one port. Triangulation can be gained through
articulating prebent instruments. 25–28
We will now discuss the advantages, disadvantages, and
difficulties that we faced during our own experience of SPLC at
the General Surgery department at Mansoura University Hospital.
A recent revolution in MIS for the majority of surgical specialties
has been the rapid recovery times with shorter hospitalization,
fewer wound-related complications post-operatively, and better
esthetic results. However, MPLC is still associated with more tissue
trauma due to the size and number of ports utilized. 18,29–31
In our study, the postoperative pain in both groups was
compared using the number of patients who required additional
analgesia for breakthrough pain (NSAIDS). Analysis of these two
items showed that postoperative pain was more in the MPLC group.
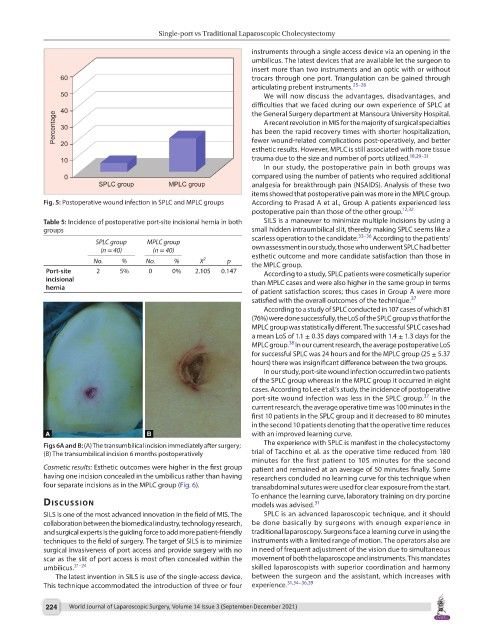
Fig. 5: Postoperative wound infection in SPLC and MPLC groups According to Prasad A et al., Group A patients experienced less
postoperative pain than those of the other group. 12,32
Table 5: Incidence of postoperative port-site incisional hernia in both SILS is a maneuver to minimize multiple incisions by using a
groups small hidden intraumbilical slit, thereby making SPLC seems like a
scarless operation to the candidate. 33–36 According to the patients’
SPLC group MPLC group
(n = 40) (n = 40) own assessment in our study, those who underwent SPLC had better
No. % No. % X 2 p esthetic outcome and more candidate satisfaction than those in
the MPLC group.
Port-site 2 5% 0 0% 2.105 0.147 According to a study, SPLC patients were cosmetically superior
incisional than MPLC cases and were also higher in the same group in terms
hernia
of patient satisfaction scores; thus cases in Group A were more
satisfied with the overall outcomes of the technique. 37
According to a study of SPLC conducted in 107 cases of which 81
(76%) were done successfully, the LoS of the SPLC group vs that for the
MPLC group was statistically different. The successful SPLC cases had
a mean LoS of 1.1 ± 0.35 days compared with 1.4 ± 1.3 days for the
38
MPLC group. In our current research, the average postoperative LoS
for successful SPLC was 24 hours and for the MPLC group (25 ± 5.37
hours) there was insignificant difference between the two groups.
In our study, port-site wound infection occurred in two patients
of the SPLC group whereas in the MPLC group it occurred in eight
cases. According to Lee et al.’s study, the incidence of postoperative
37
port-site wound infection was less in the SPLC group. In the
current research, the average operative time was 100 minutes in the
first 10 patients in the SPLC group and it decreased to 80 minutes
in the second 10 patients denoting that the operative time reduces
with an improved learning curve.
Figs 6A and B: (A) The transumbilical incision immediately after surgery; The experience with SPLC is manifest in the cholecystectomy
(B) The transumbilical incision 6 months postoperatively trial of Tacchino et al. as the operative time reduced from 180
minutes for the first patient to 105 minutes for the second
Cosmetic results: Esthetic outcomes were higher in the first group patient and remained at an average of 50 minutes finally. Some
having one incision concealed in the umbilicus rather than having researchers concluded no learning curve for this technique when
four separate incisions as in the MPLC group (Fig. 6). transabdominal sutures were used for clear exposure from the start.
To enhance the learning curve, laboratory training on dry porcine
dIscussIon models was advised. 31
SILS is one of the most advanced innovation in the field of MIS. The SPLC is an advanced laparoscopic technique, and it should
collaboration between the biomedical industry, technology research, be done basically by surgeons with enough experience in
and surgical experts is the guiding force to add more patient-friendly traditional laparoscopy. Surgeons face a learning curve in using the
techniques to the field of surgery. The target of SILS is to minimize instruments with a limited range of motion. The operators also are
surgical invasiveness of port access and provide surgery with no in need of frequent adjustment of the vision due to simultaneous
scar as the slit of port access is most often concealed within the movement of both the laparoscope and instruments. This mandates
umbilicus. 21–24 skilled laparoscopists with superior coordination and harmony
The latest invention in SILS is use of the single-access device. between the surgeon and the assistant, which increases with
This technique accommodated the introduction of three or four experience. 31,34–36,39
224 World Journal of Laparoscopic Surgery, Volume 14 Issue 3 (September-December 2021)