Page 86 - tmp
P. 86
Endoscopic Management of Post‑laparoscopic Re‑sleeve Gastrectomy
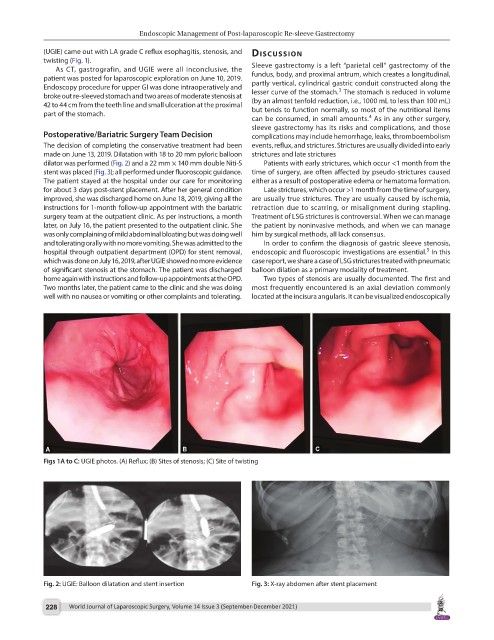
(UGIE) came out with LA grade C reflux esophagitis, stenosis, and dIscussIon
twisting (Fig. 1).
As CT, gastrografin, and UGIE were all inconclusive, the Sleeve gastrectomy is a left “parietal cell” gastrectomy of the
patient was posted for laparoscopic exploration on June 10, 2019. fundus, body, and proximal antrum, which creates a longitudinal,
Endoscopy procedure for upper GI was done intraoperatively and partly vertical, cylindrical gastric conduit constructed along the
3
broke out re-sleeved stomach and two areas of moderate stenosis at lesser curve of the stomach. The stomach is reduced in volume
42 to 44 cm from the teeth line and small ulceration at the proximal (by an almost tenfold reduction, i.e., 1000 mL to less than 100 mL)
part of the stomach. but tends to function normally, so most of the nutritional items
4
can be consumed, in small amounts. As in any other surgery,
sleeve gastrectomy has its risks and complications, and those
Postoperative/Bariatric Surgery Team Decision complications may include hemorrhage, leaks, thromboembolism
The decision of completing the conservative treatment had been events, reflux, and strictures. Strictures are usually divided into early
made on June 13, 2019. Dilatation with 18 to 20 mm pyloric balloon strictures and late strictures
dilator was performed (Fig. 2) and a 22 mm × 140 mm double Niti-S Patients with early strictures, which occur <1 month from the
stent was placed (Fig. 3); all performed under fluoroscopic guidance. time of surgery, are often affected by pseudo-strictures caused
The patient stayed at the hospital under our care for monitoring either as a result of postoperative edema or hematoma formation.
for about 3 days post-stent placement. After her general condition Late strictures, which occur >1 month from the time of surgery,
improved, she was discharged home on June 18, 2019, giving all the are usually true strictures. They are usually caused by ischemia,
instructions for 1-month follow-up appointment with the bariatric retraction due to scarring, or misalignment during stapling.
surgery team at the outpatient clinic. As per instructions, a month Treatment of LSG strictures is controversial. When we can manage
later, on July 16, the patient presented to the outpatient clinic. She the patient by noninvasive methods, and when we can manage
was only complaining of mild abdominal bloating but was doing well him by surgical methods, all lack consensus.
and tolerating orally with no more vomiting. She was admitted to the In order to confirm the diagnosis of gastric sleeve stenosis,
5
hospital through outpatient department (OPD) for stent removal, endoscopic and fluoroscopic investigations are essential. In this
which was done on July 16, 2019, after UGIE showed no more evidence case report, we share a case of LSG strictures treated with pneumatic
of significant stenosis at the stomach. The patient was discharged balloon dilation as a primary modality of treatment.
home again with instructions and follow-up appointments at the OPD. Two types of stenosis are usually documented. The first and
Two months later, the patient came to the clinic and she was doing most frequently encountered is an axial deviation commonly
well with no nausea or vomiting or other complaints and tolerating. located at the incisura angularis. It can be visualized endoscopically
Figs 1A to C: UGIE photos. (A) Reflux; (B) Sites of stenosis; (C) Site of twisting
Fig. 2: UGIE: Balloon dilatation and stent insertion Fig. 3: X-ray abdomen after stent placement
228 World Journal of Laparoscopic Surgery, Volume 14 Issue 3 (September-December 2021)