Page 76 - tmp
P. 76
Laparoscopic Hemicolectomy vs Laparoscopic Transverse Colectomy
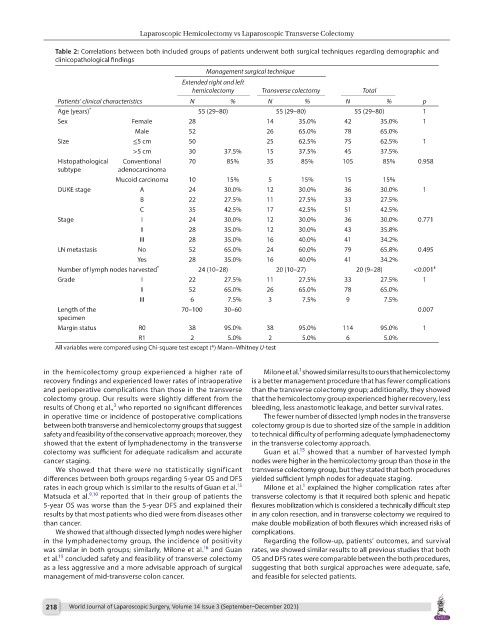
Table 2: Correlations between both included groups of patients underwent both surgical techniques regarding demographic and
clinicopathological findings
Management surgical technique
Extended right and left
hemicolectomy Transverse colectomy Total
Patients’ clinical characteristics N % N % N % p
Age (years) * 55 (29–80) 55 (29–80) 55 (29–80) 1
Sex Female 28 14 35.0% 42 35.0% 1
Male 52 26 65.0% 78 65.0%
Size ≤5 cm 50 25 62.5% 75 62.5% 1
>5 cm 30 37.5% 15 37.5% 45 37.5%
Histopathological Conventional 70 85% 35 85% 105 85% 0.958
subtype adenocarcinoma
Mucoid carcinoma 10 15% 5 15% 15 15%
DUKE stage A 24 30.0% 12 30.0% 36 30.0% 1
B 22 27.5% 11 27.5% 33 27.5%
C 35 42.5% 17 42.5% 51 42.5%
Stage I 24 30.0% 12 30.0% 36 30.0% 0.771
II 28 35.0% 12 30.0% 43 35.8%
III 28 35.0% 16 40.0% 41 34.2%
LN metastasis No 52 65.0% 24 60.0% 79 65.8% 0.495
Yes 28 35.0% 16 40.0% 41 34.2%
Number of lymph nodes harvested * 24 (10–28) 20 (10–27) 20 (9–28) <0.001 £
Grade I 22 27.5% 11 27.5% 33 27.5% 1
II 52 65.0% 26 65.0% 78 65.0%
III 6 7.5% 3 7.5% 9 7.5%
Length of the 70–100 30–60 0.007
specimen
Margin status R0 38 95.0% 38 95.0% 114 95.0% 1
R1 2 5.0% 2 5.0% 6 5.0%
All variables were compared using Chi-square test except (*) Mann–Whitney U-test
1
in the hemicolectomy group experienced a higher rate of Milone et al. showed similar results to ours that hemicolectomy
recovery findings and experienced lower rates of intraoperative is a better management procedure that has fewer complications
and perioperative complications than those in the transverse than the transverse colectomy group; additionally, they showed
colectomy group. Our results were slightly different from the that the hemicolectomy group experienced higher recovery, less
3
results of Chong et al., who reported no significant differences bleeding, less anastomotic leakage, and better survival rates.
in operative time or incidence of postoperative complications The fewer number of dissected lymph nodes in the transverse
between both transverse and hemicolectomy groups that suggest colectomy group is due to shorted size of the sample in addition
safety and feasibility of the conservative approach; moreover, they to technical difficulty of performing adequate lymphadenectomy
showed that the extent of lymphadenectomy in the transverse in the transverse colectomy approach.
15
colectomy was sufficient for adequate radicalism and accurate Guan et al. showed that a number of harvested lymph
cancer staging. nodes were higher in the hemicolectomy group than those in the
We showed that there were no statistically significant transverse colectomy group, but they stated that both procedures
differences between both groups regarding 5-year OS and DFS yielded sufficient lymph nodes for adequate staging.
1
15
rates in each group which is similar to the results of Guan et al. Milone et al. explained the higher complication rates after
Matsuda et al. 9,10 reported that in their group of patients the transverse colectomy is that it required both splenic and hepatic
5-year OS was worse than the 5-year DFS and explained their flexures mobilization which is considered a technically difficult step
results by that most patients who died were from diseases other in any colon resection, and in transverse colectomy we required to
than cancer. make double mobilization of both flexures which increased risks of
We showed that although dissected lymph nodes were higher complications.
in the lymphadenectomy group, the incidence of positivity Regarding the follow-up, patients’ outcomes, and survival
16
was similar in both groups; similarly, Milone et al. and Guan rates, we showed similar results to all previous studies that both
15
et al. concluded safety and feasibility of transverse colectomy OS and DFS rates were comparable between the both procedures,
as a less aggressive and a more advisable approach of surgical suggesting that both surgical approaches were adequate, safe,
management of mid-transverse colon cancer. and feasible for selected patients.
218 World Journal of Laparoscopic Surgery, Volume 14 Issue 3 (September–December 2021)