Page 71 - tmp
P. 71
Intraperitoneal Instillation of Ropivacaine and Postoperative Bowel Movements
Methodology There were no ICU admission or readmission in either of the
A prospective study was conducted on 28 patients undergoing groups. There was no mortality.
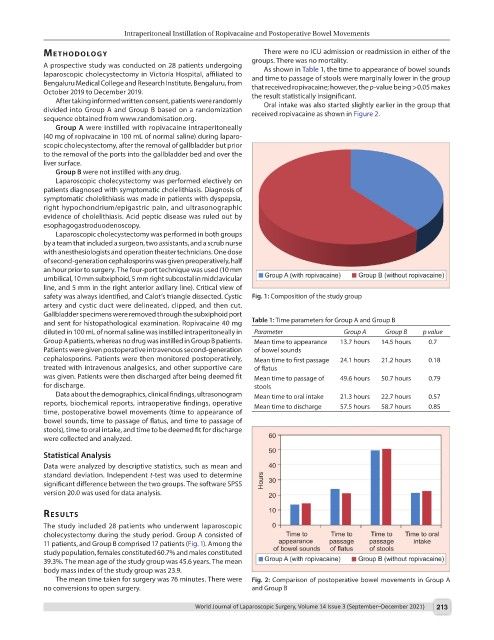
As shown in Table 1, the time to appearance of bowel sounds
laparoscopic cholecystectomy in Victoria Hospital, affiliated to and time to passage of stools were marginally lower in the group
Bengaluru Medical College and Research Institute, Bengaluru, from that received ropivacaine; however, the p-value being >0.05 makes
October 2019 to December 2019. the result statistically insignificant.
After taking informed written consent, patients were randomly Oral intake was also started slightly earlier in the group that
divided into Group A and Group B based on a randomization received ropivacaine as shown in Figure 2.
sequence obtained from www.randomisation.org.
Group A were instilled with ropivacaine intraperitoneally
(40 mg of ropivacaine in 100 mL of normal saline) during laparo-
scopic cholecystectomy, after the removal of gallbladder but prior
to the removal of the ports into the gallbladder bed and over the
liver surface.
Group B were not instilled with any drug.
Laparoscopic cholecystectomy was performed electively on
patients diagnosed with symptomatic cholelithiasis. Diagnosis of
symptomatic cholelithiasis was made in patients with dyspepsia,
right hypochondrium/epigastric pain, and ultrasonographic
evidence of cholelithiasis. Acid peptic disease was ruled out by
esophagogastroduodenoscopy.
Laparoscopic cholecystectomy was performed in both groups
by a team that included a surgeon, two assistants, and a scrub nurse
with anesthesiologists and operation theater technicians. One dose
of second-generation cephalosporins was given preoperatively, half
an hour prior to surgery. The four-port technique was used (10 mm
umbilical, 10 mm subxiphoid, 5 mm right subcostal in midclavicular
line, and 5 mm in the right anterior axillary line). Critical view of
safety was always identified, and Calot’s triangle dissected. Cystic Fig. 1: Composition of the study group
artery and cystic duct were delineated, clipped, and then cut.
Gallbladder specimens were removed through the subxiphoid port
and sent for histopathological examination. Ropivacaine 40 mg Table 1: Time parameters for Group A and Group B
diluted in 100 mL of normal saline was instilled intraperitoneally in Parameter Group A Group B p value
Group A patients, whereas no drug was instilled in Group B patients. Mean time to appearance 13.7 hours 14.5 hours 0.7
Patients were given postoperative intravenous second-generation of bowel sounds
cephalosporins. Patients were then monitored postoperatively, Mean time to first passage 24.1 hours 21.2 hours 0.18
treated with intravenous analgesics, and other supportive care of flatus
was given. Patients were then discharged after being deemed fit Mean time to passage of 49.6 hours 50.7 hours 0.79
for discharge. stools
Data about the demographics, clinical findings, ultrasonogram Mean time to oral intake 21.3 hours 22.7 hours 0.57
reports, biochemical reports, intraoperative findings, operative Mean time to discharge 57.5 hours 58.7 hours 0.85
time, postoperative bowel movements (time to appearance of
bowel sounds, time to passage of flatus, and time to passage of
stools), time to oral intake, and time to be deemed fit for discharge
were collected and analyzed.
Statistical Analysis
Data were analyzed by descriptive statistics, such as mean and
standard deviation. Independent t-test was used to determine
significant difference between the two groups. The software SPSS
version 20.0 was used for data analysis.
results
The study included 28 patients who underwent laparoscopic
cholecystectomy during the study period. Group A consisted of
11 patients, and Group B comprised 17 patients (Fig. 1). Among the
study population, females constituted 60.7% and males constituted
39.3%. The mean age of the study group was 45.6 years. The mean
body mass index of the study group was 23.9.
The mean time taken for surgery was 76 minutes. There were Fig. 2: Comparison of postoperative bowel movements in Group A
no conversions to open surgery. and Group B
World Journal of Laparoscopic Surgery, Volume 14 Issue 3 (September–December 2021) 213