Page 51 - tmp
P. 51
Intraoperative Predictors of Laparoscopic Cholecystectomy
Table 2: Proposed AMU scoring system of predicting difficult LC
GB condition Normal 0 No adhesion 0
Distended 1 Easily separable/mild adhesion 0
Edematous and inflamed 1 Adhesions Moderate adhesion requiring energy 1
Contracted and inflamed 1 Only intra-abdominal adhesion 4
Congested and inflamed 2 Intra-abdominal and GB adhesions 5
Contracted and congested 3 Very severe adhesion/buried GB 5
Empyema 5 Normal/clear 0
Intraoperative pericholecystic fluid Absent 0 Partially obscure 0
Cystic duct abnormality 2
Present 5 Calot’s triangle Partial obscure with cystic duct/
Hartman pouch status Normal/no stone 0 status vessel abnormality 5
Vessel abnormality 5
Impacted stone 5 Fully obscure frozen 5
AMU: Aligarh Muslim University
Score 0–5: Easy
Score 6 and above: Difficult
conclusIon
From this study, we concluded a scoring system based on an
intraoperative procedure that can identify difficult procedures
so as to save time and any untoward complications. Features like
intraperitoneal adhesions, structural anomalies or distortions
distended or contracted GB, and the frozen Calot’s triangle are
signs that are associated with difficulties during the surgery. These
classification systems would be of great help in improving the
outcomes of LC.
references
1. Daradkeh SS, Suwan Z, Abukhalaf M. Preoperative ultrasonography
and prediction of technical difficulties during laparoscopic
cholecystectomy. World J Surg 1994;22(1):75–77. DOI: 10.1007/
s002689900352.
2. Augustine A, Rao R, Vivek MAM. A comprehensive predictive scoring
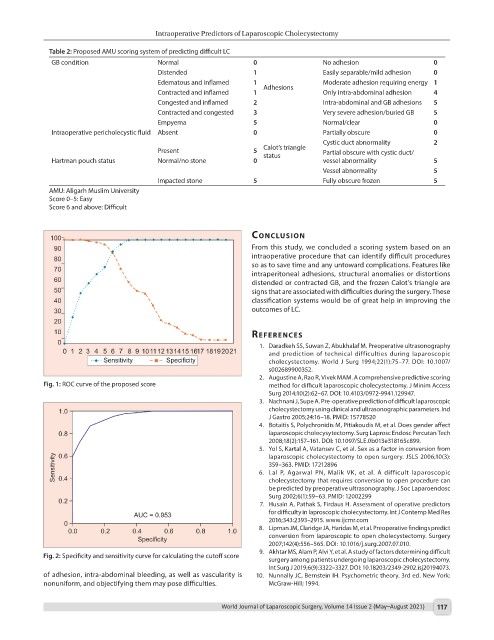
Fig. 1: ROC curve of the proposed score method for difficult laparoscopic cholecystectomy. J Minim Access
Surg 2014;10(2):62–67. DOI: 10.4103/0972-9941.129947.
3. Nachnani J, Supe A. Pre-operative prediction of difficult laparoscopic
cholecystectomy using clinical and ultrasonographic parameters. Ind
J Gastro 2005;24:16–18. PMID: 15778520
4. Botaitis S, Polychronidis M, Pitiakoudis M, et al. Does gender affect
laparoscopic cholecysytectomy. Surg Laprosc Endosc Percutan Tech
2008;18(2):157–161. DOI: 10.1097/SLE.0b013e318165c899.
5. Yol S, Kartal A, Vatansev C, et al. Sex as a factor in conversion from
laparoscopic cholecystectomy to open surgery. JSLS 2006;10(3):
359–363. PMID: 17212896
6. Lal P, Agarwal PN, Malik VK, et al. A difficult laparoscopic
cholecystectomy that requires conversion to open procedure can
be predicted by preoperative ultrasonography. J Soc Laparoendosc
Surg 2002;6(1):59–63. PMID: 12002299
7. Husain A, Pathak S, Firdaus H. Assessment of operative predictors
for difficulty in laproscopic cholecystectomy. Int J Contemp Med Res
2016;343:2393–2915. www.ijcmr.com
8. Lipman JM, Claridge JA, Haridas M, et al. Preoperative findings predict
conversion from laparoscopic to open cholecystectomy. Surgery
2007;142(4):556–565. DOI: 10.1016/j.surg.2007.07.010.
9. Akhtar MS, Alam P, Alvi Y, et al. A study of factors determining difficult
Fig. 2: Specificity and sensitivity curve for calculating the cutoff score
surgery among patients undergoing laparoscopic cholecystectomy.
Int Surg J 2019;6(9):3322–3327. DOI: 10.18203/2349-2902.isj20194073.
of adhesion, intra-abdominal bleeding, as well as vascularity is 10. Nunnally JC, Bernstein IH. Psychometric theory. 3rd ed. New York:
nonuniform, and objectifying them may pose difficulties. McGraw-Hill; 1994.
World Journal of Laparoscopic Surgery, Volume 14 Issue 2 (May–August 2021) 117