Page 32 - World Journal of Laparoscopic Surgery
P. 32
Laparoscopic Choledochal Cyst Resection with Biliary Reconstruction
Figs 2A to F: Surgical port sites (A) To applied pneumoperitoneum using Fig. 3: Bilioenteric anatomy with CC type I
an open Hasson umbilical approach; (B and C) 12 mm port; (D, E, and F)
Are optional ports and could be used at 5 mm port CC resection with simplified common bile duct reconstruction is
demonstrated in Figure 3.
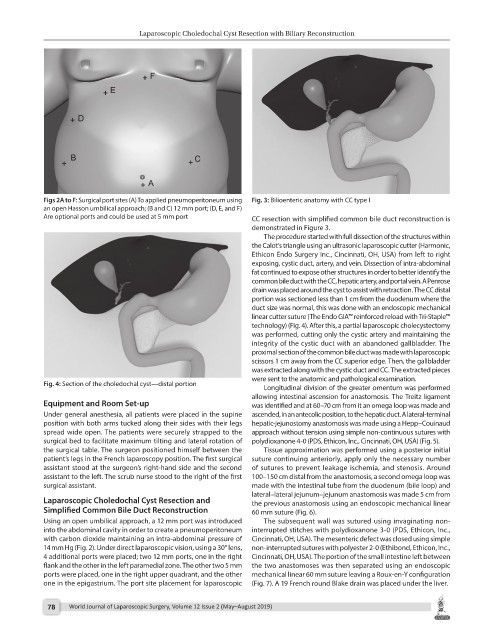
The procedure started with full dissection of the structures within
the Calot’s triangle using an ultrasonic laparoscopic cutter (Harmonic,
Ethicon Endo Surgery Inc., Cincinnati, OH, USA) from left to right
exposing, cystic duct, artery, and vein. Dissection of intra-abdominal
fat continued to expose other structures in order to better identify the
common bile duct with the CC, hepatic artery, and portal vein. A Penrose
drain was placed around the cyst to assist with retraction. The CC distal
portion was sectioned less than 1 cm from the duodenum where the
duct size was normal, this was done with an endoscopic mechanical
linear cutter suture (The Endo GIA™ reinforced reload with Tri-Staple™
technology) (Fig. 4). After this, a partial laparoscopic cholecystectomy
was performed, cutting only the cystic artery and maintaining the
integrity of the cystic duct with an abandoned gallbladder. The
proximal section of the common bile duct was made with laparoscopic
scissors 1 cm away from the CC superior edge. Then, the gallbladder
was extracted along with the cystic duct and CC. The extracted pieces
were sent to the anatomic and pathological examination.
Fig. 4: Section of the choledochal cyst—distal portion
Longitudinal division of the greater omentum was performed
allowing intestinal ascension for anastomosis. The Treitz ligament
Equipment and Room Set-up was identified and at 60–70 cm from it an omega loop was made and
Under general anesthesia, all patients were placed in the supine ascended, in an antecolic position, to the hepatic duct. A lateral-terminal
position with both arms tucked along their sides with their legs hepatic-jejunostomy anastomosis was made using a Hepp–Couinaud
spread wide open. The patients were securely strapped to the approach without tension using simple non-continuous sutures with
surgical bed to facilitate maximum tilting and lateral rotation of polydioxanone 4-0 (PDS, Ethicon, Inc., Cincinnati, OH, USA) (Fig. 5).
the surgical table. The surgeon positioned himself between the Tissue approximation was performed using a posterior initial
patient’s legs in the French laparoscopy position. The first surgical suture continuing anteriorly, apply only the necessary number
assistant stood at the surgeon’s right-hand side and the second of sutures to prevent leakage ischemia, and stenosis. Around
assistant to the left. The scrub nurse stood to the right of the first 100–150 cm distal from the anastomosis, a second omega loop was
surgical assistant. made with the intestinal tube from the duodenum (bile loop) and
lateral–lateral jejunum–jejunum anastomosis was made 5 cm from
Laparoscopic Choledochal Cyst Resection and the previous anastomosis using an endoscopic mechanical linear
Simplified Common Bile Duct Reconstruction 60 mm suture (Fig. 6).
Using an open umbilical approach, a 12 mm port was introduced The subsequent wall was sutured using invaginating non-
into the abdominal cavity in order to create a pneumoperitoneum interrupted stitches with polydioxanone 3-0 (PDS, Ethicon, Inc.,
with carbon dioxide maintaining an intra-abdominal pressure of Cincinnati, OH, USA). The mesenteric defect was closed using simple
14 mm Hg (Fig. 2). Under direct laparoscopic vision, using a 30° lens, non-interrupted sutures with polyester 2-0 (Ethibond, Ethicon, Inc.,
4 additional ports were placed; two 12 mm ports, one in the right Cincinnati, OH, USA). The portion of the small intestine left between
flank and the other in the left paramedial zone. The other two 5 mm the two anastomoses was then separated using an endoscopic
ports were placed, one in the right upper quadrant, and the other mechanical linear 60 mm suture leaving a Roux-en-Y configuration
one in the epigastrium. The port site placement for laparoscopic (Fig. 7). A 19 French round Blake drain was placed under the liver.
78 World Journal of Laparoscopic Surgery, Volume 12 Issue 2 (May–August 2019)