Page 37 - WJOLS - Laparoscopic Journal
P. 37
WJOLS
Cholecystoduodenal Fistula is not the Contraindication for Laparoscopic Surgery
surgeons all over the world. High incidence of cholelithiasis allows easier definition of the gallbladder/cystic duct junction
combined with the lack of health care facilities and the lack and circumferential dissection around the cystic duct and
of awareness on the part of the patient contributes to very cholecystoduodenal fistula (Fig. 6).
common presentation of the patient in the advanced stage
of the disease.
INVESTIGATIONS
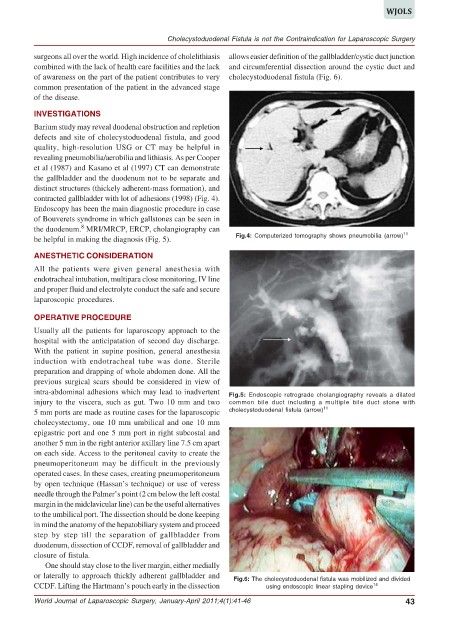
Barium study may reveal duodenal obstruction and repletion
defects and site of cholecystoduodenal fistula, and good
quality, high-resolution USG or CT may be helpful in
revealing pneumobilia/aerobilia and lithiasis. As per Cooper
et al (1987) and Kasano et al (1997) CT can demonstrate
the gallbladder and the duodenum not to be separate and
distinct structures (thickely adherent-mass formation), and
contracted gallbladder with lot of adhesions (1998) (Fig. 4).
Endoscopy has been the main diagnostic procedure in case
of Bouverets syndrome in which gallstones can be seen in
8
the duodenum. MRI/MRCP, ERCP, cholangiography can 11
be helpful in making the diagnosis (Fig. 5). Fig.4: Computerized tomography shows pneumobilia (arrow)
ANESTHETIC CONSIDERATION
All the patients were given general anesthesia with
endotracheal intubation, multipara close monitoring, IV line
and proper fluid and electrolyte conduct the safe and secure
laparoscopic procedures.
OPERATIVE PROCEDURE
Usually all the patients for laparoscopy approach to the
hospital with the anticipatation of second day discharge.
With the patient in supine position, general anesthesia
induction with endotracheal tube was done. Sterile
preparation and drapping of whole abdomen done. All the
previous surgical scars should be considered in view of
intra-abdominal adhesions which may lead to inadvertent Fig.5: Endoscopic retrograde cholangiography reveals a dilated
injury to the viscera, such as gut. Two 10 mm and two common bile duct including a multiple bile duct stone with
5 mm ports are made as routine cases for the laparoscopic cholecystoduodenal fistula (arrow) 11
cholecystectomy, one 10 mm umbilical and one 10 mm
epigastric port and one 5 mm port in right subcostal and
another 5 mm in the right anterior axillary line 7.5 cm apart
on each side. Access to the peritoneal cavity to create the
pneumoperitoneum may be difficult in the previously
operated cases. In these cases, creating pneumoperitoneum
by open technique (Hassan’s technique) or use of veress
needle through the Palmer’s point (2 cm below the left costal
margin in the midclavicular line) can be the useful alternatives
to the umbilical port. The dissection should be done keeping
in mind the anatomy of the hepatobiliary system and proceed
step by step till the separation of gallbladder from
duodenum, dissection of CCDF, removal of gallbladder and
closure of fistula.
One should stay close to the liver margin, either medially
or laterally to approach thickly adherent gallbladder and Fig.6: The cholecystoduodenal fistula was mobilized and divided
CCDF. Lifting the Hartmann’s pouch early in the dissection using endoscopic linear stapling device 14
World Journal of Laparoscopic Surgery, January-April 2011;4(1):41-46 43