Page 4 - Laparoscopic Surgery Online Journal
P. 4
T Anil Kumar et al
OPERATIVE PROCEDURE significantly less blood loss, but a longer operation time.
Since, we were interested in the number of lymph node
Laparoscopy-assisted total gastrectomy with D2 dissection:
This procedure was performed for gastric cancer involving harvested, the mean HLN’s were 24.7 in LAG group as
more than two-third of the stomach. Under five port compared 23.3 in OG group.
approach (Fig. 1) the greater omentum was first dissected,
using the harmonic scalpel along the border of the
transverse colon. The right gastroepiploic vessel was
clipped and cut at its origin with the harmonic; lymph nodes
alongside of it were removed. The duodenal tunnel was
made and duodenum was divided 2 cm distal to prepyloric
vein using linear cutting stapler (Fig. 2). Then the left
gastroepiploic vessel was cut, allowing lymph nodes
alongside it to be removed. Then the gastropancreatic fold
was exposed. Along with the gastroduodenal artery, the
common hepatic artery could be skeletonized easily. The
right gastric artery was divided and cut at its origin, from
the proper hepatic artery to complete dissection of lymph
nodes alongside of it. Then the lymph nodes located along
the celiac trunk and the left gastric artery was removed. Fig. 1: Port positions in laparoscopic gastrectomy
The left gastric artery was cut from the celiac trunk using
clips. Then the splenic artery was skeletonized from its
origin to the end in order to remove lymph nodes. After
returning the stomach and the greater omentum to normal
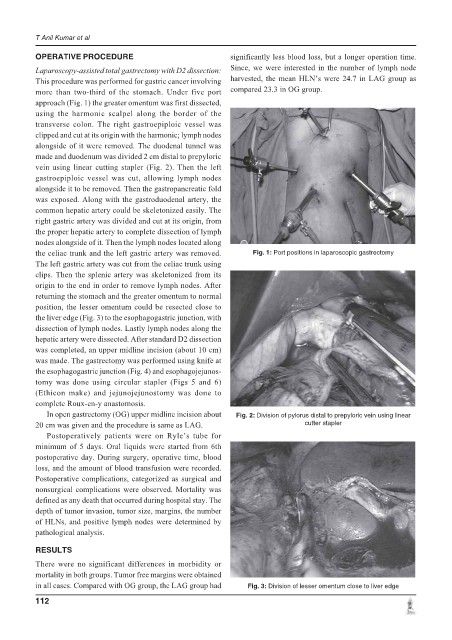
position, the lesser omentum could be resected close to
the liver edge (Fig. 3) to the esophagogastric junction, with
dissection of lymph nodes. Lastly lymph nodes along the
hepatic artery were dissected. After standard D2 dissection
was completed, an upper midline incision (about 10 cm)
was made. The gastrectomy was performed using knife at
the esophagogastric junction (Fig. 4) and esophagojejunos-
tomy was done using circular stapler (Figs 5 and 6)
(Ethicon make) and jejunojejunostomy was done to
complete Roux-en-y anastomosis.
In open gastrectomy (OG) upper midline incision about Fig. 2: Division of pylorus distal to prepyloric vein using linear
20 cm was given and the procedure is same as LAG. cutter stapler
Postoperatively patients were on Ryle’s tube for
minimum of 5 days. Oral liquids were started from 6th
postoperative day. During surgery, operative time, blood
loss, and the amount of blood transfusion were recorded.
Postoperative complications, categorized as surgical and
nonsurgical complications were observed. Mortality was
defined as any death that occurred during hospital stay. The
depth of tumor invasion, tumor size, margins, the number
of HLNs, and positive lymph nodes were determined by
pathological analysis.
RESULTS
There were no significant differences in morbidity or
mortality in both groups. Tumor free margins were obtained
in all cases. Compared with OG group, the LAG group had Fig. 3: Division of lesser omentum close to liver edge
112