Page 9 - World Journal of Laparoscopic Surgery
P. 9
Laparoscopic Common Bile Duct Exploration
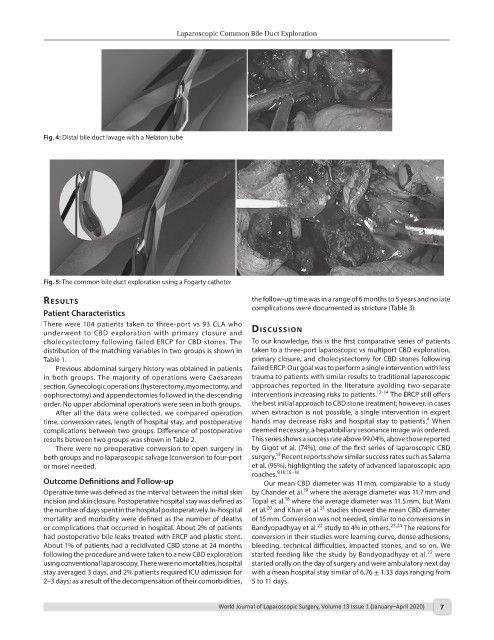
Fig. 4: Distal bile duct lavage with a Nelaton tube
Fig. 5: The common bile duct exploration using a Fogarty catheter
results the follow-up time was in a range of 6 months to 5 years and no late
Patient Characteristics complications were documented as stricture (Table 3).
There were 104 patients taken to three-port vs 93 CLA who dIscussIon
underwent to CBD exploration with primary closure and
cholecystectomy following failed ERCP for CBD stones. The To our knowledge, this is the first comparative series of patients
distribution of the matching variables in two groups is shown in taken to a three-port laparoscopic vs multiport CBD exploration,
Table 1. primary closure, and cholecystectomy for CBD stones following
Previous abdominal surgery history was obtained in patients failed ERCP. Our goal was to perform a single intervention with less
in both groups. The majority of operations were Caesarean trauma to patients with similar results to traditional laparoscopic
section. Gynecologic operations (hysterectomy, myomectomy, and approaches reported in the literature avoiding two separate
oophorectomy) and appendectomies followed in the descending interventions increasing risks to patients. 12–14 The ERCP still offers
order. No upper abdominal operations were seen in both groups. the best initial approach to CBD stone treatment; however, in cases
After all the data were collected, we compared operation when extraction is not possible, a single intervention in expert
4
time, conversion rates, length of hospital stay, and postoperative hands may decrease risks and hospital stay to patients. When
complications between two groups. Difference of postoperative deemed necessary, a hepatobiliary resonance image was ordered.
results between two groups was shown in Table 2. This series shows a success rate above 99.04%, above those reported
There were no preoperative conversion to open surgery in by Gigot et al. (74%), one of the first series of laparoscopic CBD
15
both groups and no laparoscopic salvage (conversion to four-port surgery. Recent reports show similar success rates such as Salama
or more) needed. et al. (95%), highlighting the safety of advanced laparoscopic app
roaches. 9,10,16–18
Outcome Definitions and Follow-up Our mean CBD diameter was 11 mm, comparable to a study
19
Operative time was defined as the interval between the initial skin by Chander et al. where the average diameter was 11.7 mm and
18
incision and skin closure. Postoperative hospital stay was defined as Topal et al. where the average diameter was 11.5 mm, but Wani
21
20
the number of days spent in the hospital postoperatively. In-hospital et al. and Khan et al. studies showed the mean CBD diameter
mortality and morbidity were defined as the number of deaths of 15 mm. Conversion was not needed, similar to no conversions in
22
or complications that occurred in hospital. About 2% of patients Bandyopadhyay et al. study to 4% in others. 23,24 The reasons for
had postoperative bile leaks treated with ERCP and plastic stent. conversion in their studies were learning curve, dense adhesions,
About 1% of patients had a recidivated CBD stone at 24 months bleeding, technical difficulties, impacted stones, and so on. We
22
following the procedure and were taken to a new CBD exploration started feeding like the study by Bandyopadhyay et al. were
using conventional laparoscopy. There were no mortalities, hospital started orally on the day of surgery and were ambulatory next day
stay averaged 3 days, and 2% patients required ICU admission for with a mean hospital stay similar of 6.76 ± 1.33 days ranging from
2–3 days; as a result of the decompensation of their comorbidities, 5 to 11 days.
World Journal of Laparoscopic Surgery, Volume 13 Issue 1 (January–April 2020) 7