Page 47 - WJOLS
P. 47
WJOLS
Laparoscopic Rectopexy: Is It Useful for Persistent Rectal Prolapse in Children?
proctoscopy and EMG anal sphincter and pelvic floor in (2 cm between each suture in the rectum) seromuscular
all patients. Computed tomography (CT) scan was done for sutures of PDS size 3/0 using intracorporeal knotting (Fig. 5).
the two children with neurological problem. The authorized Closure of the right peritoneal window with interrupted 3/0
person was informed by the full details about the procedure absorbable suture was done to cover the mesh and close the
and consented. cavity (Fig. 6). Patients were kept nil orally till the return of
All children were given enemas each 6 hours 1 day bowel sounds. Postoperatively, stool softeners were routinely
before the surgery. Prophylactic antibiotics were given at prescribed for at least 12 weeks.
the time of induction of anesthesia. All were operated under
general anesthesia with endotracheal intubation. After full RESULTS
anesthesia and under complete sterilization catheter inserted Of the 14 children, 10 (71.42%) were males and four
to evacuate the urinary bladder. Supraumbilical transverse (28.57%) were females. Male to female ratio was 2:1. The
skin incision was done for 5 mm Ethicon XCEL port with mean age of presentation was 5 years (3-8 years). The
5 mm 00 scope introduction to the peritoneum under presenting complaints were mass descending per rectum
vision on the laparoscope monitor, then co insufflation to along with bleeding per rectum lasting from 1 to 3 years.
2
peritoneum up to 12 mm Hg intra-abdominal pressure was All had rectal prolapse of 5 to 7 cm in length. Two children
operand with hemodynamic and respiratory monitoring by were under neuropsychiatric treatment and one had walking
anesthesia. Introduction of 5 mm, 30º scope at umbilicus port problem. The two neuropsychiatric children were both
and two 5 mm working ports in midclavicular line followed males and weighted 17.4 and 18.2 kg at ages 7 and 9 years,
this over the line joining midinguinal point and both costal respectively. The child with walking problem was a female
margins. The position of the working ports varied with the aged 6 years and weighted 13.8 kg, which was below the
child height and abdominal cavity size, ensuring acceptable 5th centile as per NCHS weight for age charts. The remaining
ergonomics according to the child body built. Trendelenburg 11 out of 14 children were normal in weight and fell between
position removed the bowel away from the pelvis. the 20th and 50th centile by NCHS standards.
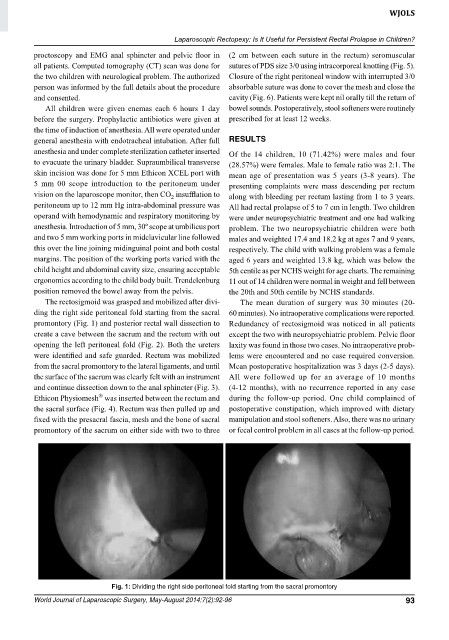
The rectosigmoid was grasped and mobilized after divi- The mean duration of surgery was 30 minutes (20-
ding the right side peritoneal fold starting from the sacral 60 minutes). No intraoperative complications were reported.
promontory (Fig. 1) and posterior rectal wall dissection to Redundancy of rectosigmoid was noticed in all patients
create a cave between the sacrum and the rectum with out except the two with neuropsychiatric problem. Pelvic floor
opening the left peritoneal fold (Fig. 2). Both the ureters laxity was found in those two cases. No intraoperative prob -
were identified and safe guarded. Rectum was mobilized lems were encountered and no case required conversion.
from the sacral promontory to the lateral ligaments, and until Mean postoperative hospitalization was 3 days (2-5 days).
the surface of the sacrum was clearly felt with an instrument All were followed up for an average of 10 months
and continue dissection down to the anal sphincter (Fig. 3). (4-12 months), with no recurrence reported in any case
®
Ethicon Physiomesh was inserted between the rectum and during the follow-up period. One child complained of
the sacral surface (Fig. 4). Rectum was then pulled up and postoperative constipation, which improved with dietary
fixed with the presacral fascia, mesh and the bone of sacral manipulation and stool softeners. Also, there was no urinary
promontory of the sacrum on either side with two to three or fecal control problem in all cases at the follow-up period.
Fig. 1: Dividing the right side peritoneal fold starting from the sacral promontory
World Journal of Laparoscopic Surgery, May-August 2014;7(2):92-96 93