Page 5 - Journal of Laparoscopic Surgery - WALS Journal
P. 5
WJOLS
Two-port Laparoscopic Cholecystectomy
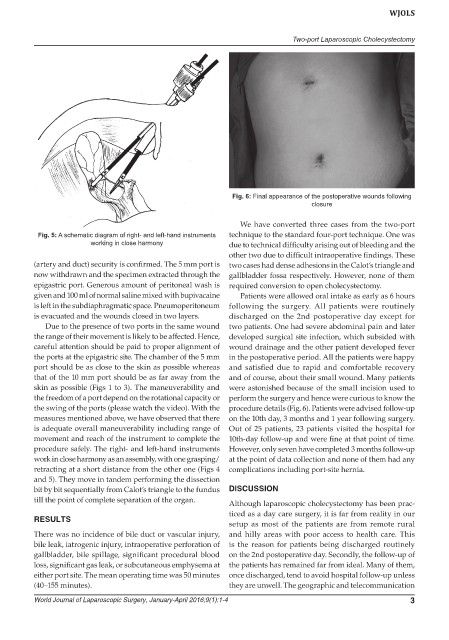
Fig. 6: Final appearance of the postoperative wounds following
closure
We have converted three cases from the two-port
Fig. 5: A schematic diagram of right- and left-hand instruments technique to the standard four-port technique. One was
working in close harmony due to technical difficulty arising out of bleeding and the
other two due to difficult intraoperative findings. These
(artery and duct) security is confirmed. The 5 mm port is two cases had dense adhesions in the Calot’s triangle and
now withdrawn and the specimen extracted through the gallbladder fossa respectively. However, none of them
epigastric port. Generous amount of peritoneal wash is required conversion to open cholecystectomy.
given and 100 ml of normal saline mixed with bupivacaine Patients were allowed oral intake as early as 6 hours
is left in the subdiaphragmatic space. Pneumoperitoneum following the surgery. All patients were routinely
is evacuated and the wounds closed in two layers. discharged on the 2nd postoperative day except for
Due to the presence of two ports in the same wound two patients. One had severe abdominal pain and later
the range of their movement is likely to be affected. Hence, developed surgical site infection, which subsided with
careful attention should be paid to proper alignment of wound drainage and the other patient developed fever
the ports at the epigastric site. The chamber of the 5 mm in the postoperative period. All the patients were happy
port should be as close to the skin as possible whereas and satisfied due to rapid and comfortable recovery
that of the 10 mm port should be as far away from the and of course, about their small wound. Many patients
skin as possible (Figs 1 to 3). The maneuverability and were astonished because of the small incision used to
the freedom of a port depend on the rotational capacity or perform the surgery and hence were curious to know the
the swing of the ports (please watch the video). With the procedure details (Fig. 6). Patients were advised follow-up
measures mentioned above, we have observed that there on the 10th day, 3 months and 1 year following surgery.
is adequate overall maneuverability including range of Out of 25 patients, 23 patients visited the hospital for
movement and reach of the instrument to complete the 10th-day follow-up and were fine at that point of time.
procedure safely. The right- and left-hand instruments However, only seven have completed 3 months follow-up
work in close harmony as an assembly, with one grasping/ at the point of data collection and none of them had any
retracting at a short distance from the other one (Figs 4 complications including port-site hernia.
and 5). They move in tandem performing the dissection
bit by bit sequentially from Calot’s triangle to the fundus DISCUSSION
till the point of complete separation of the organ.
Although laparoscopic cholecystectomy has been prac-
ticed as a day care surgery, it is far from reality in our
RESULTS
setup as most of the patients are from remote rural
There was no incidence of bile duct or vascular injury, and hilly areas with poor access to health care. This
bile leak, iatrogenic injury, intraoperative perforation of is the reason for patients being discharged routinely
gallbladder, bile spillage, significant procedural blood on the 2nd postoperative day. Secondly, the follow-up of
loss, significant gas leak, or subcutaneous emphysema at the patients has remained far from ideal. Many of them,
either port site. The mean operating time was 50 minutes once discharged, tend to avoid hospital follow-up unless
(40–155 minutes). they are unwell. The geographic and telecommunication
World Journal of Laparoscopic Surgery, January-April 2016;9(1):1-4 3