Page 6 - World Journal of Laparoscopic Surgery
P. 6
Mohamed Abdelmohsen, Hazem Badr
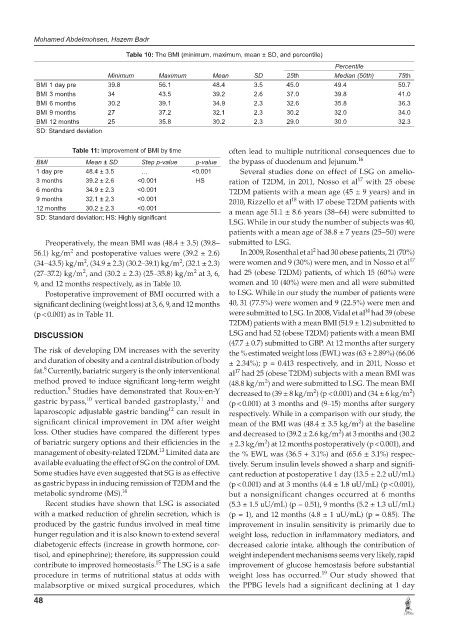
Table 10: The BMI (minimum, maximum, mean ± SD, and percentile)
Percentile
Minimum Maximum Mean SD 25th Median (50th) 75th
BMI 1 day pre 39.8 56.1 48.4 3.5 45.0 49.4 50.7
BMI 3 months 34 43.5 39.2 2.6 37.0 39.8 41.0
BMI 6 months 30.2 39.1 34.9 2.3 32.6 35.8 36.3
BMI 9 months 27 37.2 32.1 2.3 30.2 32.0 34.0
BMI 12 months 25 35.8 30.2 2.3 29.0 30.0 32.3
SD: Standard deviation
Table 11: Improvement of BMI by time often lead to multiple nutritional consequences due to
BMI Mean ± SD Step p-value p-value the bypass of duodenum and Jejunum. 16
1 day pre 48.4 ± 3.5 … <0.001 Several studies done on effect of LSG on amelio-
17
3 months 39.2 ± 2.6 <0.001 HS ration of T2DM, in 2011, Nosso et al with 25 obese
6 months 34.9 ± 2.3 <0.001 T2DM patients with a mean age (45 ± 9 years) and in
9 months 32.1 ± 2.3 <0.001 2010, Rizzello et al with 17 obese T2DM patients with
18
12 months 30.2 ± 2.3 <0.001 a mean age 51.1 ± 8.6 years (38–64) were submitted to
SD: Standard deviation; HS: Highly significant
LSG. While in our study the number of subjects was 40,
patients with a mean age of 38.8 ± 7 years (25–50) were
Preoperatively, the mean BMI was (48.4 ± 3.5) (39.8– submitted to LSG.
2
2
56.1) kg/m and postoperative values were (39.2 ± 2.6) In 2009, Rosenthal et al had 30 obese patients, 21 (70%)
17
(34–43.5) kg/m , (34.9 ± 2.3) (30.2–39.1) kg/m , (32.1 ± 2.3) were women and 9 (30%) were men, and in Nosso et al
2
2
(27–37.2) kg/m , and (30.2 ± 2.3) (25–35.8) kg/m at 3, 6, had 25 (obese T2DM) patients, of which 15 (60%) were
2
2
9, and 12 months respectively, as in Table 10. women and 10 (40%) were men and all were submitted
Postoperative improvement of BMI occurred with a to LSG. While in our study the number of patients were
significant declining (weight loss) at 3, 6, 9, and 12 months 40, 31 (77.5%) were women and 9 (22.5%) were men and
14
(p < 0.001) as in Table 11. were submitted to LSG. In 2008, Vidal et al had 39 (obese
T2DM) patients with a mean BMI (51.9 ± 1.2) submitted to
DISCUSSION LSG and had 52 (obese T2DM) patients with a mean BMI
(47.7 ± 0.7) submitted to GBP. At 12 months after surgery
The risk of developing DM increases with the severity the % estimated weight loss (EWL) was (63 ± 2.89%) (66.06
and duration of obesity and a central distribution of body ± 2.34%); p = 0.413 respectively, and in 2011, Nosso et
8
fat. Currently, bariatric surgery is the only interventional al had 25 (obese T2DM) subjects with a mean BMI was
17
method proved to induce significant long-term weight (48.8 kg/m ) and were submitted to LSG. The mean BMI
2
9
reduction. Studies have demonstrated that Roux-en-Y decreased to (39 ± 8 kg/m ) (p < 0.001) and (34 ± 6 kg/m )
2
2
10
11
gastric bypass, vertical banded gastroplasty, and (p < 0.001) at 3 months and (9–15) months after surgery
12
laparoscopic adjustable gastric banding can result in respectively. While in a comparison with our study, the
significant clinical improvement in DM after weight mean of the BMI was (48.4 ± 3.5 kg/m ) at the baseline
2
loss. Other studies have compared the different types and decreased to (39.2 ± 2.6 kg/m ) at 3 months and (30.2
2
of bariatric surgery options and their efficiencies in the ± 2.3 kg/m ) at 12 months postoperatively (p < 0.001), and
2
13
management of obesity-related T2DM. Limited data are the % EWL was (36.5 + 3.1%) and (65.6 ± 3.1%) respec-
available evaluating the effect of SG on the control of DM. tively. Serum insulin levels showed a sharp and signifi-
Some studies have even suggested that SG is as effective cant reduction at postoperative 1 day (13.5 ± 2.2 uU/mL)
as gastric bypass in inducing remission of T2DM and the (p < 0.001) and at 3 months (4.4 ± 1.8 uU/mL) (p < 0.001),
metabolic syndrome (MS). 14 but a nonsignificant changes occurred at 6 months
Recent studies have shown that LSG is associated (5.3 ± 1.5 uU/mL) (p = 0.51), 9 months (5.2 ± 1.3 uU/mL)
with a marked reduction of ghrelin secretion, which is (p = 1), and 12 months (4.8 ± 1 uU/mL) (p = 0.85). The
produced by the gastric fundus involved in meal time improvement in insulin sensitivity is primarily due to
hunger regulation and it is also known to extend several weight loss, reduction in inflammatory mediators, and
diabetogenic effects (increase in growth hormone, cor- decreased calorie intake, although the contribution of
tisol, and epinephrine); therefore, its suppression could weight independent mechanisms seems very likely, rapid
15
contribute to improved homeostasis. The LSG is a safe improvement of glucose hemostasis before substantial
19
procedure in terms of nutritional status at odds with weight loss has occurred. Our study showed that
malabsorptive or mixed surgical procedures, which the PPBG levels had a significant declining at 1 day
48