Page 6 - wjols
P. 6
Ten-point Strategy for Safe Laparoscopic Cholecystectomy
injuries from trocar or Veress needle insertion and major bile duct
injuries. 18–20
This study also shows that if LC is performed with patience,
complication rates can be reduced to minimal and conversion rates
can be reduced to zero.
Bile duct injury is one of the most dreaded complications during
LC than in OC. 21–23 In the infancy of LC, a CBD injury occurred more
frequently during LC than OC. Although the incidence of CBD injury
during LC is no longer as high as it was initially, it still exceeds that
24
of OC (0.1–0.5 in LC vs 0.2% in OC). Risk factors for a CBD injury
are lack of experience (learning curve), misidentification of biliary
anatomy, intraoperative bleeding, lack of recognition of anatomical
variation of biliary tree, and improperly functioning instruments.
Other factors are acute and chronic cholecystitis, empyema, long-
standing recurrent disease, advanced age, obesity, and previous
surgery. 24,25 Considering the factors, in mind we assigned three
points in the strategy.
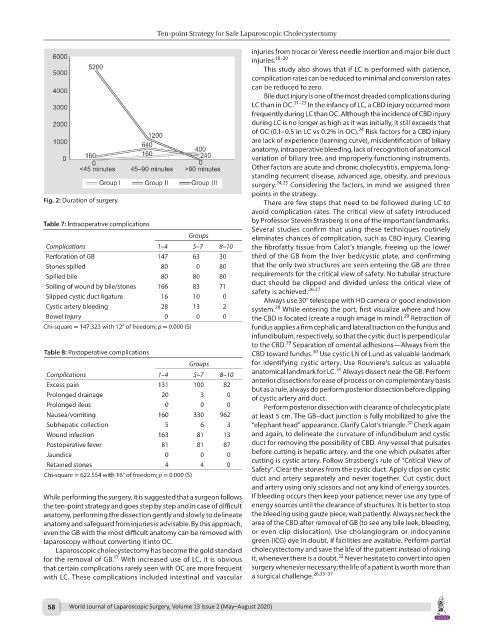
Fig. 2: Duration of surgery There are few steps that need to be followed during LC to
avoid complication rates. The critical view of safety introduced
by Professor Steven Strasberg is one of the important landmarks.
Table 7: Intraoperative complications
Several studies confirm that using these techniques routinely
Groups eliminates chances of complication, such as CBD injury. Clearing
Complications 1–4 5–7 8–10 the fibrofatty tissue from Calot’s triangle, freeing up the lower
Perforation of GB 147 63 30 third of the GB from the liver bed/cystic plate, and confirming
Stones spilled 80 0 80 that the only two structures are seen entering the GB are three
Spilled bile 80 80 80 requirements for the critical view of safety. No tubular structure
Soiling of wound by bile/stones 166 83 71 duct should be clipped and divided unless the critical view of
26,27
safety is achieved.
Slipped cystic duct ligature 16 10 0 Always use 30° telescope with HD camera or good endovision
Cystic artery bleeding 28 13 2 system. While entering the port, first visualize where and how
28
Bowel injury 0 0 0 the CBD is located (create a rough image in mind). Retraction of
29
Chi-square = 147.323 with 12° of freedom; p = 0.000 (S) fundus applies a firm cephalic and lateral traction on the fundus and
infundibulum, respectively, so that the cystic duct is perpendicular
29
to the CBD. Separation of omental adhesions—Always from the
Table 8: Postoperative complications CBD toward fundus. Use cystic LN of Lund as valuable landmark
30
Groups for identifying cystic artery. Use Rouviere’s sulcus as valuable
31
Complications 1–4 5–7 8–10 anatomical landmark for LC. Always dissect near the GB. Perform
Excess pain 131 100 82 anterior dissections for ease of process or on complementary basis
but as a rule, always do perform posterior dissection before clipping
Prolonged drainage 20 3 0 of cystic artery and duct.
Prolonged ileus 0 0 0 Perform posterior dissection with clearance of cholecystic plate
Nausea/vomiting 160 330 962 at least 5 cm. The GB–duct junction is fully mobilized to give the
30
Subhepatic collection 5 6 3 “elephant head” appearance. Clarify Calot’s triangle. Check again
Wound infection 163 81 13 and again, to delineate the curvature of infundibulum and cystic
Postoperative fever 81 81 87 duct for removing the possibility of CBD. Any vessel that pulsates
Jaundice 0 0 0 before cutting is hepatic artery, and the one which pulsates after
Retained stones 4 4 0 cutting is cystic artery. Follow Strasberg’s rule of “Critical View of
Safety”. Clear the stones from the cystic duct. Apply clips on cystic
Chi-square = 622.554 with 16° of freedom; p = 0.000 (S)
duct and artery separately and never together. Cut cystic duct
and artery using only scissors and not any kind of energy sources.
While performing the surgery, it is suggested that a surgeon follows If bleeding occurs then keep your patience; never use any type of
the ten-point strategy and goes step by step and in case of difficult energy sources until the clearance of structures. It is better to stop
anatomy, performing the dissection gently and slowly to delineate the bleeding using gauze piece, wait patiently. Always recheck the
anatomy and safeguard from injuries is advisable. By this approach, area of the CBD after removal of GB (to see any bile leek, bleeding,
even the GB with the most difficult anatomy can be removed with or even clip dislocation). Use cholangiogram or indocyanine
laparoscopy without converting it into OC. green (ICG) dye in doubt, if facilities are available. Perform partial
Laparoscopic cholecystectomy has become the gold standard cholecystectomy and save the life of the patient instead of risking
32
17
for the removal of GB. With increased use of LC, it is obvious it, whenever there is a doubt. Never hesitate to convert into open
that certain complications rarely seen with OC are more frequent surgery whenever necessary; the life of a patient is worth more than
with LC. These complications included intestinal and vascular a surgical challenge. 26,33–37
58 World Journal of Laparoscopic Surgery, Volume 13 Issue 2 (May–August 2020)