Infection Control in Laparoscopic Surgery: Best Practices
Title: Infection Control in Laparoscopic Surgery: Best Practices
Introduction
Laparoscopic surgery, also known as minimally invasive surgery, has revolutionized the field of surgery by offering patients shorter recovery times, reduced pain, and smaller incisions compared to traditional open surgeries. However, despite its numerous advantages, laparoscopic surgery is not immune to the risk of infections. Infection control is a critical aspect of ensuring successful outcomes in laparoscopic procedures. This article delves into the best practices for infection control in laparoscopic surgery, emphasizing the importance of maintaining a sterile environment, proper instrument handling, and adherence to established protocols.
Understanding the Risks
While laparoscopic surgery minimizes the risk of infections compared to open surgeries, it is not without its challenges. The insertion of trocars and instruments into the abdominal cavity creates potential entry points for bacteria, and any breach in aseptic technique can lead to infections. Infections in laparoscopic surgery can result in complications such as delayed recovery, extended hospital stays, and increased healthcare costs. Therefore, meticulous infection control measures are imperative to mitigate these risks and optimize patient outcomes.
Preoperative Preparations
Patient Selection and Screening:
Before embarking on laparoscopic surgery, thorough patient selection and screening are essential. Identifying patients with pre-existing conditions that may compromise their immune system or increase infection risk is crucial. Additionally, screening for infections, especially in the abdominal area, helps in determining the appropriate course of action.
Antibiotic Prophylaxis:
Administering prophylactic antibiotics before surgery is a standard practice to reduce the risk of surgical site infections (SSIs). Tailoring antibiotic selection to the specific procedure and adhering to recommended timing guidelines are critical for effectiveness. However, it is equally important to avoid unnecessary prolonged antibiotic use, which can contribute to antibiotic resistance.
Intraoperative Measures
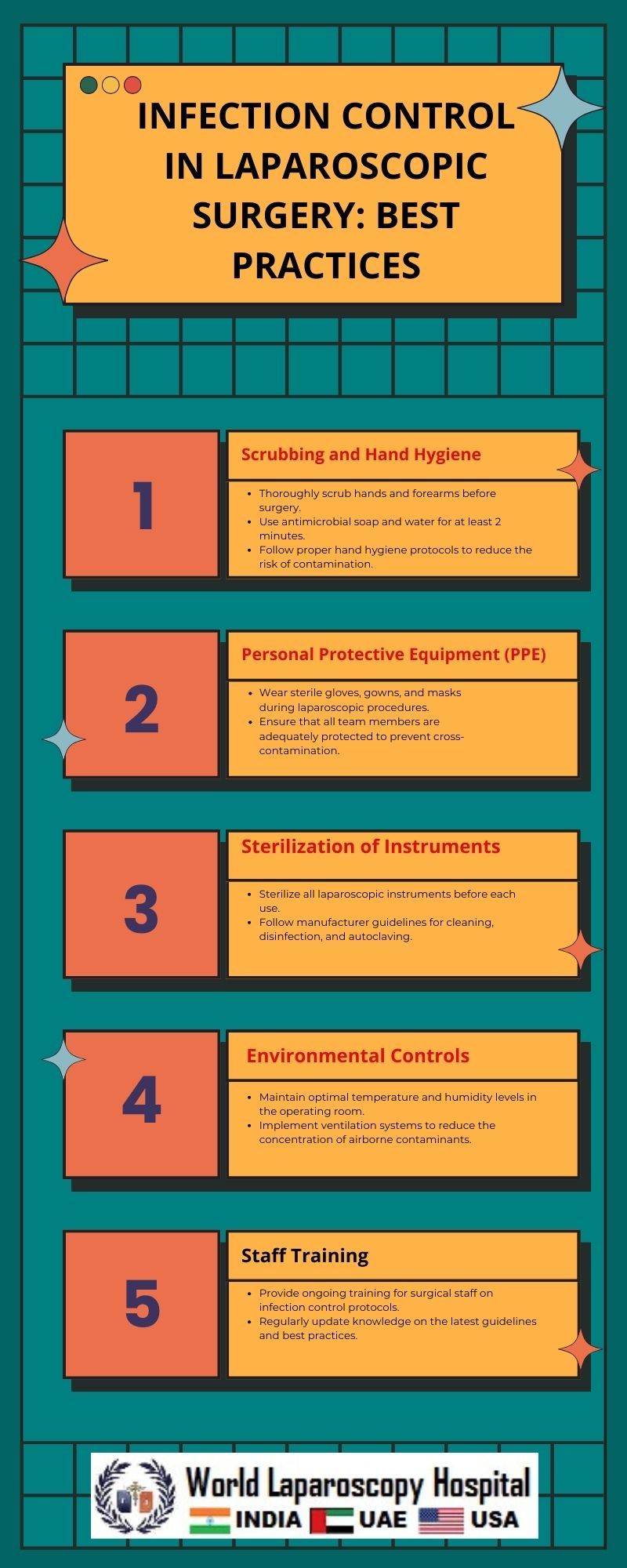
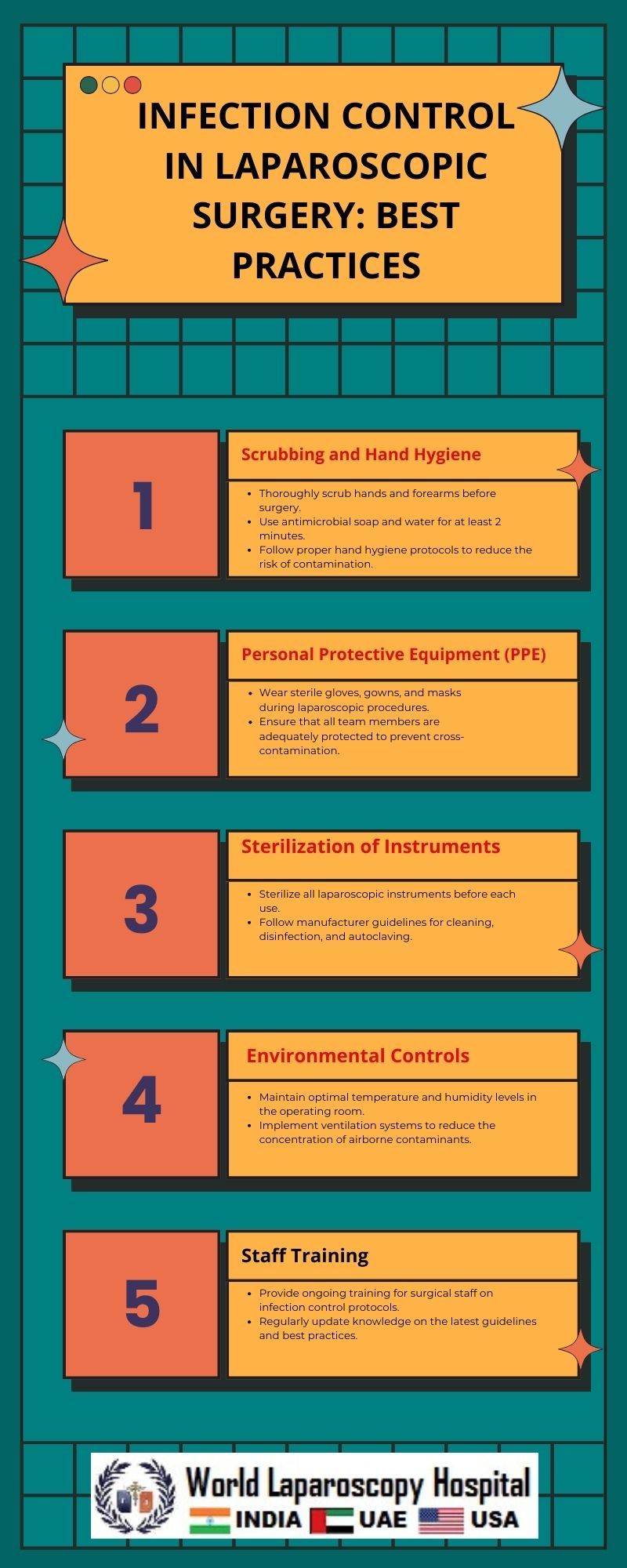
Sterile Technique:
Maintaining a sterile surgical field is paramount in laparoscopic surgery. Strict adherence to aseptic techniques during patient draping, trocar insertion, and throughout the procedure minimizes the risk of introducing pathogens. Sterile gowns, gloves, and drapes should be used, and personnel should follow established protocols for hand hygiene.
Trocar Placement and Entry Techniques:
The correct placement of trocars is crucial for preventing complications and minimizing the risk of infections. Entry techniques, such as the closed or open method, should be chosen based on patient factors and surgeon preference. Verifying the adequacy of insufflation, using proper trocar sizes, and ensuring a clear visual field are essential steps in infection prevention.
Instrument Handling and Sterilization:
Laparoscopic instruments must undergo rigorous sterilization processes to eliminate any potential pathogens. Regular maintenance and inspection of instruments are vital to ensure proper functioning and prevent the risk of contamination during surgery. Surgeons and operating room staff should be well-versed in handling instruments aseptically.
Postoperative Care
Wound Care:
Even with minimally invasive incisions, proper wound care is essential in preventing infections. The use of sterile dressings and regular monitoring of incisions help identify early signs of infection. Patient education on postoperative care, including wound hygiene and recognizing signs of infection, plays a crucial role in infection prevention.
Surveillance and Early Detection:
Implementing a surveillance system for monitoring SSIs allows for early detection and intervention. Regular follow-up appointments enable healthcare providers to assess the patient's recovery progress and promptly address any signs of infection. Timely intervention can significantly reduce the severity and impact of postoperative infections.
Antimicrobial Stewardship:
Prudent use of antimicrobials postoperatively is crucial in preventing the development of antibiotic-resistant strains. Tailoring antibiotic therapy based on culture results, when available, helps in selecting the most effective treatment. Additionally, clear communication between surgical and infectious disease teams enhances overall antimicrobial stewardship efforts.
Institutional Protocols and Training
Standard Operating Procedures (SOPs):
Establishing and adhering to institutional SOPs for laparoscopic surgeries are critical components of infection control. These protocols should encompass preoperative, intraoperative, and postoperative measures, ensuring a standardized approach to minimize variability and enhance patient safety.
Training and Education:
Ongoing training and education for surgical teams are imperative to reinforce infection control practices. Regular updates on the latest guidelines, techniques, and technologies help healthcare professionals stay informed and implement best practices consistently. Simulation training can also provide a hands-on learning experience for maintaining a sterile surgical environment.
Conclusion
Infection control in laparoscopic surgery is a multifaceted endeavor that involves meticulous attention to detail at every stage of the surgical process. From preoperative patient screening to postoperative care, a comprehensive approach is essential for minimizing the risk of infections and optimizing patient outcomes. Surgeons, operating room staff, and healthcare institutions must collaborate to establish and adhere to stringent protocols, fostering a culture of safety and excellence in laparoscopic surgery. By prioritizing infection control measures, the medical community can continue to enhance the safety and efficacy of minimally invasive procedures, ensuring the ongoing success of laparoscopic surgery in modern healthcare.
Top
Introduction
Laparoscopic surgery, also known as minimally invasive surgery, has revolutionized the field of surgery by offering patients shorter recovery times, reduced pain, and smaller incisions compared to traditional open surgeries. However, despite its numerous advantages, laparoscopic surgery is not immune to the risk of infections. Infection control is a critical aspect of ensuring successful outcomes in laparoscopic procedures. This article delves into the best practices for infection control in laparoscopic surgery, emphasizing the importance of maintaining a sterile environment, proper instrument handling, and adherence to established protocols.
Understanding the Risks
While laparoscopic surgery minimizes the risk of infections compared to open surgeries, it is not without its challenges. The insertion of trocars and instruments into the abdominal cavity creates potential entry points for bacteria, and any breach in aseptic technique can lead to infections. Infections in laparoscopic surgery can result in complications such as delayed recovery, extended hospital stays, and increased healthcare costs. Therefore, meticulous infection control measures are imperative to mitigate these risks and optimize patient outcomes.
Preoperative Preparations
Patient Selection and Screening:
Before embarking on laparoscopic surgery, thorough patient selection and screening are essential. Identifying patients with pre-existing conditions that may compromise their immune system or increase infection risk is crucial. Additionally, screening for infections, especially in the abdominal area, helps in determining the appropriate course of action.
Antibiotic Prophylaxis:
Administering prophylactic antibiotics before surgery is a standard practice to reduce the risk of surgical site infections (SSIs). Tailoring antibiotic selection to the specific procedure and adhering to recommended timing guidelines are critical for effectiveness. However, it is equally important to avoid unnecessary prolonged antibiotic use, which can contribute to antibiotic resistance.
Intraoperative Measures
Sterile Technique:
Maintaining a sterile surgical field is paramount in laparoscopic surgery. Strict adherence to aseptic techniques during patient draping, trocar insertion, and throughout the procedure minimizes the risk of introducing pathogens. Sterile gowns, gloves, and drapes should be used, and personnel should follow established protocols for hand hygiene.
Trocar Placement and Entry Techniques:
The correct placement of trocars is crucial for preventing complications and minimizing the risk of infections. Entry techniques, such as the closed or open method, should be chosen based on patient factors and surgeon preference. Verifying the adequacy of insufflation, using proper trocar sizes, and ensuring a clear visual field are essential steps in infection prevention.
Instrument Handling and Sterilization:
Laparoscopic instruments must undergo rigorous sterilization processes to eliminate any potential pathogens. Regular maintenance and inspection of instruments are vital to ensure proper functioning and prevent the risk of contamination during surgery. Surgeons and operating room staff should be well-versed in handling instruments aseptically.
Postoperative Care
Wound Care:
Even with minimally invasive incisions, proper wound care is essential in preventing infections. The use of sterile dressings and regular monitoring of incisions help identify early signs of infection. Patient education on postoperative care, including wound hygiene and recognizing signs of infection, plays a crucial role in infection prevention.
Surveillance and Early Detection:
Implementing a surveillance system for monitoring SSIs allows for early detection and intervention. Regular follow-up appointments enable healthcare providers to assess the patient's recovery progress and promptly address any signs of infection. Timely intervention can significantly reduce the severity and impact of postoperative infections.
Antimicrobial Stewardship:
Prudent use of antimicrobials postoperatively is crucial in preventing the development of antibiotic-resistant strains. Tailoring antibiotic therapy based on culture results, when available, helps in selecting the most effective treatment. Additionally, clear communication between surgical and infectious disease teams enhances overall antimicrobial stewardship efforts.
Institutional Protocols and Training
Standard Operating Procedures (SOPs):
Establishing and adhering to institutional SOPs for laparoscopic surgeries are critical components of infection control. These protocols should encompass preoperative, intraoperative, and postoperative measures, ensuring a standardized approach to minimize variability and enhance patient safety.
Training and Education:
Ongoing training and education for surgical teams are imperative to reinforce infection control practices. Regular updates on the latest guidelines, techniques, and technologies help healthcare professionals stay informed and implement best practices consistently. Simulation training can also provide a hands-on learning experience for maintaining a sterile surgical environment.
Conclusion
Infection control in laparoscopic surgery is a multifaceted endeavor that involves meticulous attention to detail at every stage of the surgical process. From preoperative patient screening to postoperative care, a comprehensive approach is essential for minimizing the risk of infections and optimizing patient outcomes. Surgeons, operating room staff, and healthcare institutions must collaborate to establish and adhere to stringent protocols, fostering a culture of safety and excellence in laparoscopic surgery. By prioritizing infection control measures, the medical community can continue to enhance the safety and efficacy of minimally invasive procedures, ensuring the ongoing success of laparoscopic surgery in modern healthcare.