Obesity is a growing health concern worldwide, and bariatric surgery has become a popular treatment option for individuals with severe obesity. Laparoscopic adjustable gastric banding (LAGB) is one of the most common bariatric surgeries performed worldwide. LAGB involves placing an adjustable band around the upper part of the stomach, which creates a small pouch and restricts food intake. While LAGB has been shown to be effective in promoting weight loss in the short term, the long-term outcomes of this surgery remain a topic of debate. In this essay, we will discuss the long-term outcomes of LAGB, including its effects on weight loss, comorbidities, and quality of life.
Background
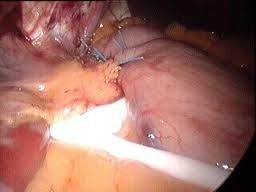
LAGB was first introduced in the 1980s as a modification of traditional open gastric banding surgery. In LAGB, the surgeon makes small incisions in the abdomen and places an adjustable band around the upper part of the stomach. The band is connected to a port that is placed under the skin, which allows for adjustment of the band's tightness.
LAGB is a reversible procedure and can be removed if necessary. Additionally, LAGB has a lower complication rate than other bariatric surgeries, such as gastric bypass and sleeve gastrectomy.
Weight Loss Outcomes of LAGB
One of the primary goals of LAGB is to promote weight loss in individuals with severe obesity. Several studies have shown that LAGB is effective in promoting weight loss in the short term, with patients experiencing an average weight loss of 45-60% of excess weight in the first two years after surgery.
However, the long-term weight loss outcomes of LAGB are less clear. Some studies have shown that patients maintain significant weight loss up to ten years after surgery, while others have shown that weight regain occurs over time. Additionally, weight loss outcomes may vary depending on factors such as patient age, sex, and initial weight.
Comorbidity Outcomes of LAGB
Obesity is associated with a variety of comorbidities, including diabetes, hypertension, and sleep apnea. LAGB has been shown to be effective in improving these comorbidities in the short term. Several studies have shown that LAGB can lead to significant improvements in diabetes control, blood pressure, and sleep apnea in the first two years after surgery.
However, the long-term effects of LAGB on comorbidities are less clear. Some studies have shown that LAGB can lead to sustained improvements in comorbidities up to ten years after surgery, while others have shown that improvements may decrease over time.
Quality of Life Outcomes of LAGB
Obesity can have a negative impact on an individual's quality of life, including their physical, emotional, and social well-being. LAGB has been shown to improve quality of life in the short term, with patients reporting improvements in physical functioning, emotional well-being, and social functioning in the first two years after surgery.
However, the long-term effects of LAGB on quality of life are less clear. Some studies have shown that quality of life improvements may be sustained up to ten years after surgery, while others have shown that quality of life may decrease over time.
Challenges and Complications of LAGB
While LAGB has many potential benefits, it also has several challenges and complications that must be carefully considered. One of the main challenges of LAGB is the need for frequent band adjustments. The tightness of the band must be adjusted periodically to ensure optimal weight loss outcomes. Additionally, the band may need to be removed or replaced if complications such as band slippage or erosion occur.
Other complications of LAGB include infection, bleeding, and port site problems. Additionally, LAGB can lead to long-term complications such as band intolerance, gastroesophageal reflux disease (GERD), and esophageal dilation.
Furthermore, LAGB is not a suitable option for all individuals with severe obesity. Patients who have previously undergone abdominal surgery, have a history of esophageal or gastric disease, or have a BMI over 50 may not be candidates for LAGB.
Conclusion
LAGB is a popular bariatric surgery that has been shown to be effective in promoting weight loss and improving comorbidities and quality of life in the short term. However, the long-term outcomes of LAGB are less clear. While some studies have shown sustained weight loss and improvements in comorbidities and quality of life up to ten years after surgery, others have shown weight regain and decreasing improvements over time.
Additionally, LAGB has several challenges and complications that must be carefully considered, including the need for frequent band adjustments and the risk of long-term complications such as band intolerance, GERD, and esophageal dilation.
Ultimately, the decision to undergo LAGB should be made on a case-by-case basis, taking into account the patient's medical history, the risks and benefits of the surgery, and the potential long-term outcomes. Patients considering LAGB should discuss their options with their healthcare provider and carefully weigh the potential risks and benefits of this surgery.
It is important for patients to have realistic expectations about the outcomes of LAGB and to understand that this surgery is not a magic cure for obesity. While LAGB can be an effective tool for promoting weight loss and improving comorbidities and quality of life, it requires significant lifestyle changes and ongoing commitment to maintaining a healthy weight.
Additionally, it is important for patients to understand that LAGB is not a suitable option for all individuals with severe obesity. Patients must be carefully screened to ensure that they are appropriate candidates for the surgery and that the potential benefits outweigh the risks.
As with any surgical procedure, it is essential for patients to carefully follow postoperative instructions and attend regular follow-up appointments with their healthcare provider. This can help to ensure optimal outcomes and prevent complications or long-term problems.
As the field of bariatric surgery continues to advance, new techniques and procedures may emerge that offer improved outcomes for patients with severe obesity. It is important for patients and healthcare providers to stay informed about the latest developments in this field and to carefully weigh the potential risks and benefits of each surgical approach.
In conclusion, LAGB is a popular bariatric surgery that has been shown to be effective in promoting weight loss and improving comorbidities and quality of life in the short term. While the long-term outcomes of LAGB are less clear, patients who are appropriate candidates for this surgery may benefit from sustained weight loss and improvements in comorbidities and quality of life. However, LAGB requires significant lifestyle changes and ongoing commitment to maintaining a healthy weight, and it is not a suitable option for all individuals with severe obesity. Patients considering LAGB should carefully weigh the potential risks and benefits of this surgery and discuss their options with their healthcare provider.