Introduction
Laparoscopic surgery, also known as minimally invasive surgery, has revolutionized the field of surgical interventions by offering patients shorter recovery times, reduced pain, and smaller incisions. However, despite its numerous advantages, laparoscopic procedures pose unique challenges when it comes to infection management. In this comprehensive guide, we will delve into the intricacies of infection control in laparoscopic surgery, exploring the key principles, challenges, and evolving strategies that shape this critical aspect of patient care.
Understanding Laparoscopic Surgery
Before delving into infection management, it's essential to grasp the fundamentals of laparoscopic surgery. Unlike traditional open surgeries, laparoscopic procedures involve making small incisions through which a camera and specialized instruments are inserted. The surgeon navigates and performs the surgery with real-time visualization on a monitor. While this approach offers remarkable benefits, such as decreased blood loss and shorter hospital stays, it presents unique considerations for infection prevention.
The Importance of Infection Management
Infections remain a significant concern in any surgical setting, and laparoscopic procedures are no exception. Inadequate infection management can lead to severe complications, prolonged recovery periods, and increased healthcare costs. As such, implementing rigorous infection control measures is imperative to ensure optimal patient outcomes.
Aseptic Techniques in Laparoscopic Surgery
Maintaining a sterile surgical environment is fundamental to preventing infections. Aseptic techniques, which involve creating and maintaining a bacteria-free field during surgery, play a pivotal role. Sterile drapes, gowns, and gloves are standard components of these measures. Additionally, strict hand hygiene protocols and proper gowning procedures contribute to minimizing the risk of microbial contamination.
Instrument Sterilization and Handling
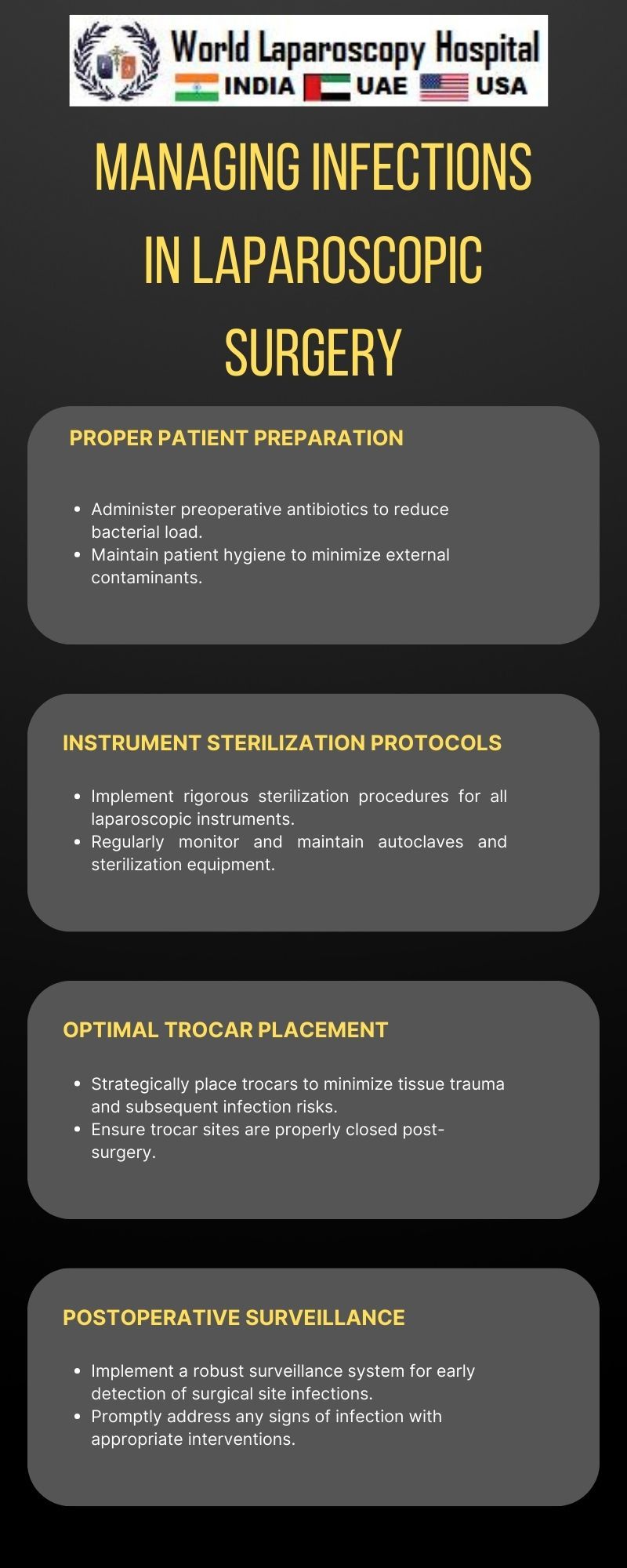
Laparoscopic instruments must undergo meticulous sterilization to prevent the introduction of pathogens into the surgical site. The delicate nature of these instruments requires specialized handling to avoid damage during sterilization processes. Surgeons and operating room staff must be well-trained in the proper care, cleaning, and sterilization of laparoscopic instruments to guarantee their efficacy and patient safety.
Prophylactic Antibiotics: Balancing Efficacy and Prudence
Prophylactic antibiotics are a cornerstone of infection prevention in laparoscopic surgery. Administered before incision, these antibiotics target potential pathogens, reducing the risk of surgical site infections. However, selecting the appropriate antibiotic, timing of administration, and duration of use are critical considerations. Striking the right balance is essential to maximize efficacy while minimizing the development of antibiotic resistance and other adverse effects.
Challenges in Laparoscopic Infection Management
Despite advancements in surgical techniques and infection control measures, laparoscopic procedures present unique challenges. Limited access and visibility in the surgical field, as well as the potential for instrument-related contamination, necessitate heightened vigilance. Surgeons and their teams must navigate these challenges with precision to ensure optimal patient safety.
Postoperative Monitoring and Surveillance
Postoperative monitoring and surveillance are crucial components of infection management in laparoscopic surgery. Close observation of patients for signs of infection, such as fever, increased pain, or abnormal wound appearance, allows for early detection and intervention. Regular follow-up appointments enable healthcare providers to address any emerging issues promptly, reducing the risk of complications.
Emerging Technologies and Innovations
The landscape of laparoscopic surgery is continually evolving, with technological advancements playing a significant role in infection management. Innovations such as robotic-assisted surgery and advanced imaging systems enhance the precision of procedures while minimizing the risk of contamination. Staying abreast of these developments is essential for healthcare professionals seeking to optimize infection control strategies in laparoscopic surgery.
Education and Training
Effective infection management in laparoscopic surgery relies on the expertise of surgical teams. Ongoing education and training programs are essential to ensure that healthcare professionals are well-versed in the latest protocols, technologies, and best practices. Simulated training environments can provide hands-on experience, allowing surgeons and their teams to hone their skills in a risk-free setting.
Conclusion
Managing infections in laparoscopic surgery demands a multifaceted approach that encompasses aseptic techniques, instrument sterilization, judicious antibiotic use, and vigilant postoperative monitoring. As technology continues to advance, so too will our ability to enhance infection control measures and improve patient outcomes. By staying informed, adopting best practices, and embracing innovations, healthcare professionals can navigate the intricate terrain of laparoscopic surgery with confidence and proficiency, ultimately ensuring the well-being of their patients.