Postoperative Care in Laparoscopic Surgery: Best Practices
Introduction:
Laparoscopic surgery has revolutionized the field of surgery, offering patients a minimally invasive alternative to traditional open procedures. While the benefits of reduced scarring and quicker recovery are evident, the importance of postoperative care in laparoscopic surgery cannot be overstated. This article explores the best practices in postoperative care for patients undergoing laparoscopic procedures, aiming to provide a comprehensive guide for healthcare professionals and patients alike.
Understanding Laparoscopic Surgery:
Laparoscopic surgery, also known as minimally invasive surgery, involves making small incisions through which a camera and specialized instruments are inserted to perform surgical procedures. Common laparoscopic surgeries include cholecystectomy, appendectomy, and various gynecological procedures. The reduced trauma to the body during these surgeries contributes to quicker recovery times, but proper postoperative care is essential for optimal outcomes.
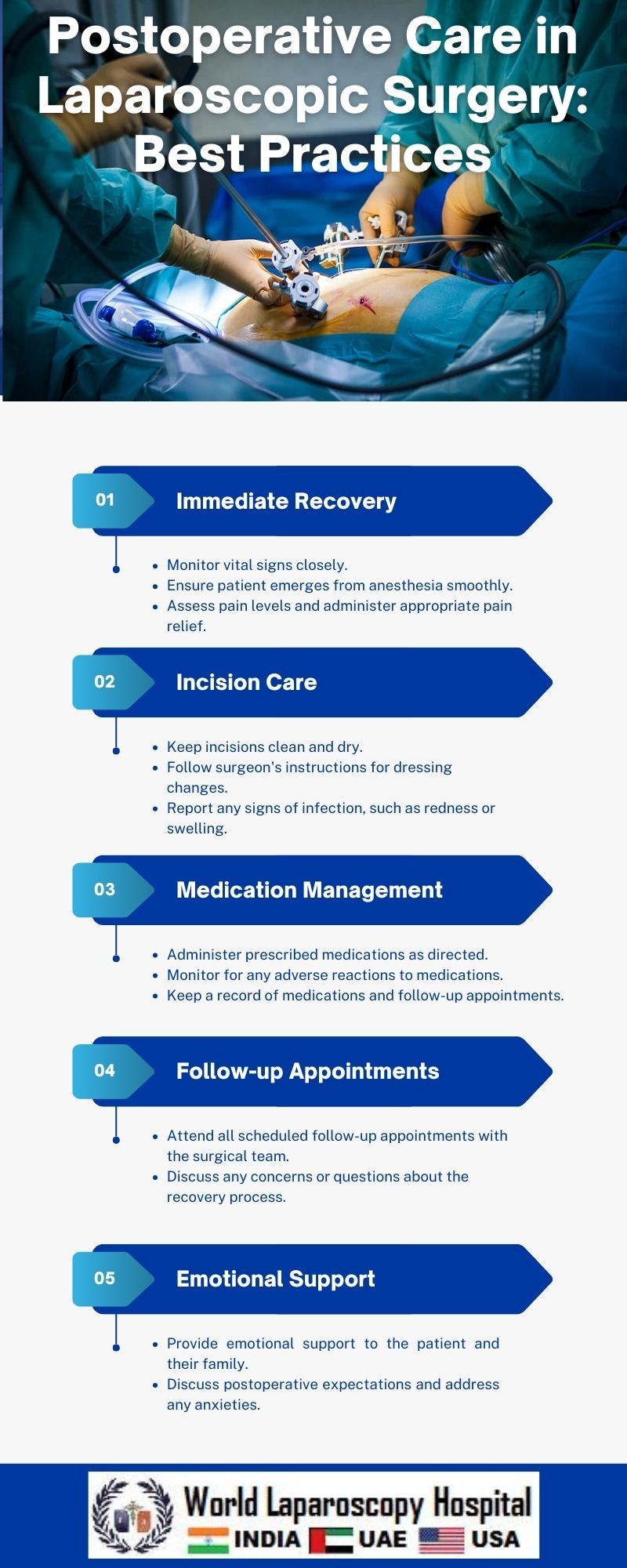
Immediate Postoperative Period:
Monitoring Vital Signs:
The first hours after laparoscopic surgery are critical, and continuous monitoring of vital signs is paramount. Blood pressure, heart rate, respiratory rate, and oxygen saturation levels should be closely observed to detect any signs of instability early on.
Pain Management:
Effective pain management is crucial for patient comfort and recovery. A multimodal approach, combining non-opioid analgesics, local anesthetics, and patient-controlled analgesia (PCA), can minimize pain while reducing the risk of opioid-related side effects.
Fluid Management:
Intravenous fluids are administered to maintain hydration and support organ function. Monitoring urine output helps assess renal function and ensures adequate fluid balance.
Ambulation and Early Mobilization:
Encouraging early ambulation and mobilization aids in preventing complications such as deep vein thrombosis (DVT) and atelectasis. Gradual movement helps restore normal physiological functions and promotes faster recovery.
Intermediate Postoperative Care:
Dietary Management:
Transitioning from a clear liquid diet to solid foods is gradual, allowing the gastrointestinal system to adapt. Monitoring for nausea, vomiting, and bowel movements is crucial to ensure the digestive tract's proper functioning.
Respiratory Care:
Deep breathing exercises and incentive spirometry are employed to prevent respiratory complications. Patients are educated on the importance of these exercises in maintaining lung function and preventing atelectasis.
Wound Care:
While laparoscopic incisions are smaller than those in open surgery, proper wound care is essential. Sterile dressings and regular inspections for signs of infection or hematoma are standard practices.
Pain Control Strategies:
Tailoring pain management strategies to the patient's individual needs helps strike a balance between pain relief and minimizing side effects. Non-pharmacological approaches, such as relaxation techniques, can complement pharmacological interventions.
Long-Term Postoperative Care:
Follow-up Appointments:
Scheduled follow-up appointments with the surgical team are vital for monitoring the patient's progress. Postoperative visits allow for the evaluation of wound healing, assessment of any residual symptoms, and addressing patient concerns.
Activity and Exercise:
Gradual resumption of normal activities and exercise is encouraged, taking into account the specific surgery performed. Physical therapy may be recommended to optimize recovery and restore full functionality.
Psychosocial Support:
Surgery, even minimally invasive, can be emotionally challenging. Providing psychosocial support through counseling or support groups can help patients cope with the psychological aspects of their recovery.
Complication Monitoring:
Vigilant monitoring for potential complications such as infection, bleeding, or herniation is crucial in the long-term postoperative period. Patients should be educated on warning signs and encouraged to seek medical attention if they experience any concerning symptoms.
Patient Education:
Empowering patients with knowledge about their postoperative care is integral to a successful recovery. Clear communication regarding expectations, potential complications, and self-care measures enhances patient compliance and overall satisfaction.
Conclusion:
Postoperative care in laparoscopic surgery is a dynamic and multifaceted process that extends beyond the operating room. Implementing best practices, including vigilant monitoring, effective pain management, and comprehensive patient education, is essential for ensuring optimal outcomes. Healthcare professionals play a pivotal role in guiding patients through the various stages of recovery, ultimately contributing to a smoother and more successful healing process after laparoscopic surgery.






