The Role of Simulation in Laparoscopic Surgical Training
The Role of Simulation in Laparoscopic Surgical Training
Introduction
Laparoscopic surgery has revolutionized the field of minimally invasive procedures, offering patients faster recovery times, reduced pain, and minimized scarring. However, the mastery of laparoscopic techniques demands rigorous training, and this is where simulation becomes a pivotal ally in shaping the skills of future surgeons.
Evolution of Laparoscopic Surgery
To appreciate the role of simulation in laparoscopic surgical training, it is essential to understand the evolution of laparoscopic surgery itself. The technique, also known as keyhole or minimally invasive surgery, involves making small incisions through which a camera and specialized instruments are inserted, allowing surgeons to visualize and operate inside the body. The transition from traditional open surgery to laparoscopic procedures marked a paradigm shift, bringing forth numerous advantages but also introducing a new set of challenges for surgeons.
Challenges in Laparoscopic Surgical Training
Learning laparoscopic techniques poses unique challenges for surgeons. Unlike open surgery, where the surgical field is directly accessible, laparoscopy demands a different skill set. Surgeons must adapt to a two-dimensional visual representation on a screen, hand-eye coordination with long and narrow instruments, and a restricted field of motion. These factors make the learning curve steep, emphasizing the need for effective training methodologies.
The Birth of Surgical Simulation
The concept of simulation in medical training is not new, but its integration into laparoscopic surgical education has been transformative. Traditional methods of learning involved a gradual transition from observation to hands-on experience in the operating room. However, this approach presented ethical concerns, as patients could be subjected to the learning curve of inexperienced surgeons.
Simulation emerged as a solution to address these concerns. By replicating realistic surgical scenarios in a controlled environment, trainees could practice and refine their skills without putting patients at risk. The development of virtual reality (VR) and augmented reality (AR) technologies further enhanced the fidelity of simulations, providing an immersive and lifelike experience for trainees.
Components of Laparoscopic Surgical Simulation
Hardware-Based Simulators
Hardware-based simulators form the foundation of laparoscopic surgical training programs. These simulators consist of physical components that mimic the look and feel of laparoscopic instruments and equipment. Trainees interact with these simulators to perform tasks such as suturing, cutting, and manipulating objects in a simulated surgical field. Feedback mechanisms, including haptic feedback, provide a sense of touch and resistance, enhancing the realism of the training experience.
Virtual Reality (VR) Simulators
VR simulators take laparoscopic surgical training to the next level by immersing trainees in a computer-generated environment. Using headsets and hand controllers, surgeons can navigate and interact with a three-dimensional virtual space that replicates the intricacies of the human body. VR simulations offer a high degree of realism, allowing trainees to practice complex procedures and develop spatial awareness in a risk-free setting.
Augmented Reality (AR) Applications
AR integrates digital information into the real-world environment, enhancing the surgeon's view during laparoscopic procedures. Through the use of transparent displays or smart glasses, AR overlays critical information, such as anatomical structures and procedural guidance, onto the surgeon's field of vision. This technology promotes enhanced situational awareness and precision, contributing to improved surgical outcomes.
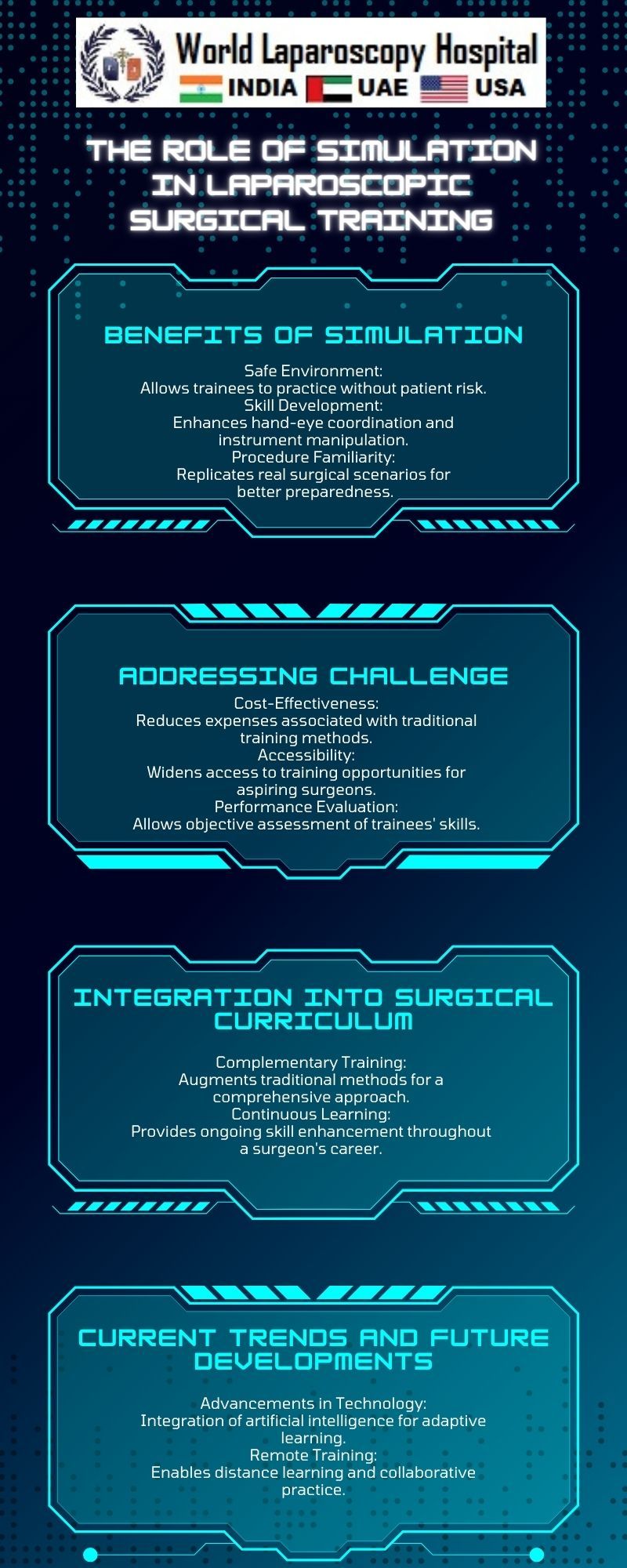
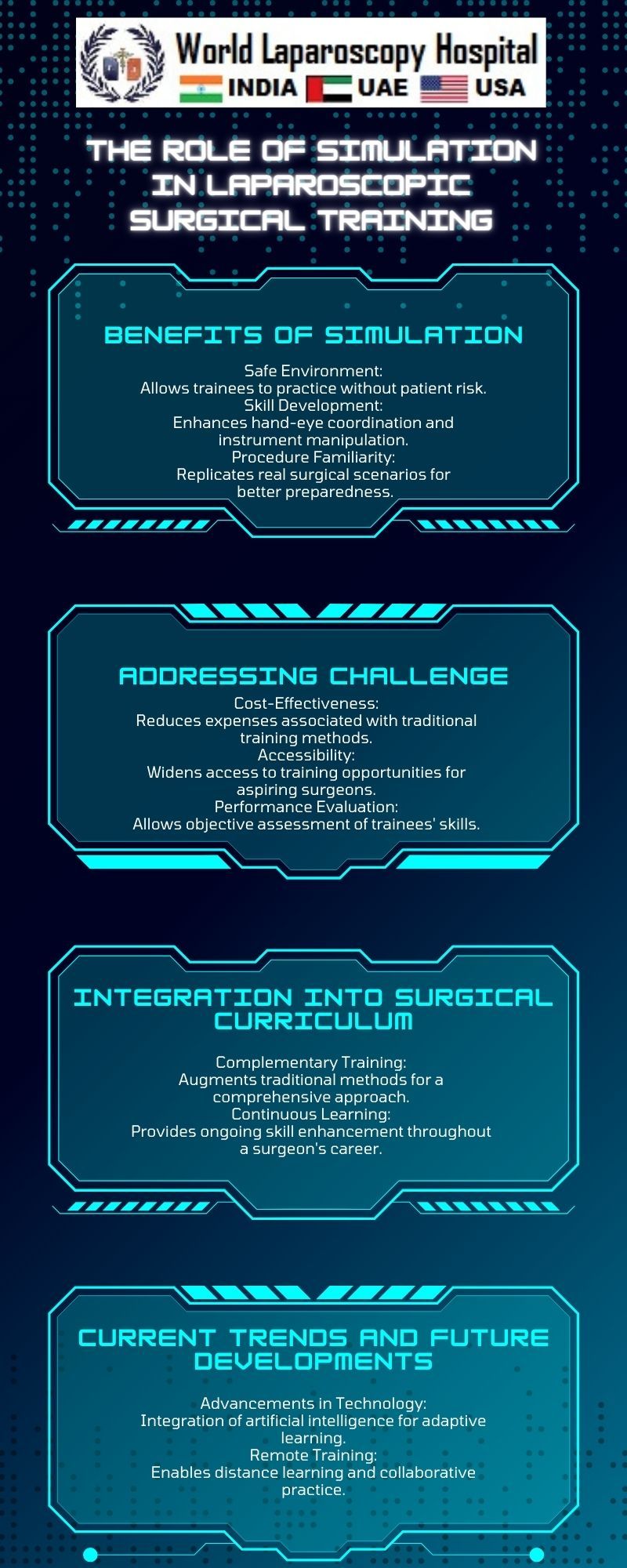
Advantages of Laparoscopic Surgical Simulation
Risk Mitigation
One of the primary advantages of laparoscopic surgical simulation is the mitigation of risks associated with traditional training methods. Trainees can make mistakes and learn from them without compromising patient safety. This approach minimizes the likelihood of errors during actual surgeries, fostering a safer and more competent surgical workforce.
Skill Acquisition and Proficiency
Simulation allows for deliberate practice, a key concept in skill acquisition. Trainees can repeat specific tasks and procedures until they achieve proficiency, building muscle memory and refining their techniques. The controlled environment of simulation enables a focused and structured approach to skill development, accelerating the learning process.
Objective Assessment
Simulation platforms often include performance metrics and assessment tools that objectively evaluate a trainee's skills. Quantifiable data, such as completion time, accuracy, and instrument handling, provide valuable insights for educators and trainees alike. This data-driven approach enhances the objectivity of assessments and facilitates targeted feedback for improvement.
Team Training
Laparoscopic procedures often involve collaboration among surgical teams. Simulation extends its benefits beyond individual skill development to team training scenarios. Surgeons, nurses, and other team members can practice coordination and communication in a simulated environment, fostering a cohesive and efficient surgical team.
Challenges and Limitations
While laparoscopic surgical simulation has revolutionized training methodologies, it is not without challenges and limitations. Cost considerations, access to high-quality simulation platforms, and the ongoing evolution of technology are factors that impact the widespread adoption of simulation in surgical education. Additionally, the ethical implications of balancing simulation training with real patient experiences warrant careful consideration.
Future Directions and Innovations
As technology continues to advance, the future of laparoscopic surgical simulation holds exciting possibilities. Artificial intelligence (AI) integration, personalized learning pathways, and adaptive simulations that respond to individual trainee performance are areas of ongoing research and development. The synergy between simulation and emerging technologies is poised to further refine and individualize surgical training experiences.
Conclusion
Laparoscopic surgical simulation stands as a cornerstone in the evolution of surgical education, providing a safe and effective means for trainees to acquire and refine their skills. The combination of hardware-based simulators, virtual reality, and augmented reality technologies offers a comprehensive approach to training, with benefits ranging from risk mitigation to objective skill assessment. As technology continues to shape the landscape of medical education, the role of simulation in laparoscopic surgical training will undoubtedly play a pivotal role in shaping the next generation of skilled and confident surgeons.
Top
Introduction
Laparoscopic surgery has revolutionized the field of minimally invasive procedures, offering patients faster recovery times, reduced pain, and minimized scarring. However, the mastery of laparoscopic techniques demands rigorous training, and this is where simulation becomes a pivotal ally in shaping the skills of future surgeons.
Evolution of Laparoscopic Surgery
To appreciate the role of simulation in laparoscopic surgical training, it is essential to understand the evolution of laparoscopic surgery itself. The technique, also known as keyhole or minimally invasive surgery, involves making small incisions through which a camera and specialized instruments are inserted, allowing surgeons to visualize and operate inside the body. The transition from traditional open surgery to laparoscopic procedures marked a paradigm shift, bringing forth numerous advantages but also introducing a new set of challenges for surgeons.
Challenges in Laparoscopic Surgical Training
Learning laparoscopic techniques poses unique challenges for surgeons. Unlike open surgery, where the surgical field is directly accessible, laparoscopy demands a different skill set. Surgeons must adapt to a two-dimensional visual representation on a screen, hand-eye coordination with long and narrow instruments, and a restricted field of motion. These factors make the learning curve steep, emphasizing the need for effective training methodologies.
The Birth of Surgical Simulation
The concept of simulation in medical training is not new, but its integration into laparoscopic surgical education has been transformative. Traditional methods of learning involved a gradual transition from observation to hands-on experience in the operating room. However, this approach presented ethical concerns, as patients could be subjected to the learning curve of inexperienced surgeons.
Simulation emerged as a solution to address these concerns. By replicating realistic surgical scenarios in a controlled environment, trainees could practice and refine their skills without putting patients at risk. The development of virtual reality (VR) and augmented reality (AR) technologies further enhanced the fidelity of simulations, providing an immersive and lifelike experience for trainees.
Components of Laparoscopic Surgical Simulation
Hardware-Based Simulators
Hardware-based simulators form the foundation of laparoscopic surgical training programs. These simulators consist of physical components that mimic the look and feel of laparoscopic instruments and equipment. Trainees interact with these simulators to perform tasks such as suturing, cutting, and manipulating objects in a simulated surgical field. Feedback mechanisms, including haptic feedback, provide a sense of touch and resistance, enhancing the realism of the training experience.
Virtual Reality (VR) Simulators
VR simulators take laparoscopic surgical training to the next level by immersing trainees in a computer-generated environment. Using headsets and hand controllers, surgeons can navigate and interact with a three-dimensional virtual space that replicates the intricacies of the human body. VR simulations offer a high degree of realism, allowing trainees to practice complex procedures and develop spatial awareness in a risk-free setting.
Augmented Reality (AR) Applications
AR integrates digital information into the real-world environment, enhancing the surgeon's view during laparoscopic procedures. Through the use of transparent displays or smart glasses, AR overlays critical information, such as anatomical structures and procedural guidance, onto the surgeon's field of vision. This technology promotes enhanced situational awareness and precision, contributing to improved surgical outcomes.
Advantages of Laparoscopic Surgical Simulation
Risk Mitigation
One of the primary advantages of laparoscopic surgical simulation is the mitigation of risks associated with traditional training methods. Trainees can make mistakes and learn from them without compromising patient safety. This approach minimizes the likelihood of errors during actual surgeries, fostering a safer and more competent surgical workforce.
Skill Acquisition and Proficiency
Simulation allows for deliberate practice, a key concept in skill acquisition. Trainees can repeat specific tasks and procedures until they achieve proficiency, building muscle memory and refining their techniques. The controlled environment of simulation enables a focused and structured approach to skill development, accelerating the learning process.
Objective Assessment
Simulation platforms often include performance metrics and assessment tools that objectively evaluate a trainee's skills. Quantifiable data, such as completion time, accuracy, and instrument handling, provide valuable insights for educators and trainees alike. This data-driven approach enhances the objectivity of assessments and facilitates targeted feedback for improvement.
Team Training
Laparoscopic procedures often involve collaboration among surgical teams. Simulation extends its benefits beyond individual skill development to team training scenarios. Surgeons, nurses, and other team members can practice coordination and communication in a simulated environment, fostering a cohesive and efficient surgical team.
Challenges and Limitations
While laparoscopic surgical simulation has revolutionized training methodologies, it is not without challenges and limitations. Cost considerations, access to high-quality simulation platforms, and the ongoing evolution of technology are factors that impact the widespread adoption of simulation in surgical education. Additionally, the ethical implications of balancing simulation training with real patient experiences warrant careful consideration.
Future Directions and Innovations
As technology continues to advance, the future of laparoscopic surgical simulation holds exciting possibilities. Artificial intelligence (AI) integration, personalized learning pathways, and adaptive simulations that respond to individual trainee performance are areas of ongoing research and development. The synergy between simulation and emerging technologies is poised to further refine and individualize surgical training experiences.
Conclusion
Laparoscopic surgical simulation stands as a cornerstone in the evolution of surgical education, providing a safe and effective means for trainees to acquire and refine their skills. The combination of hardware-based simulators, virtual reality, and augmented reality technologies offers a comprehensive approach to training, with benefits ranging from risk mitigation to objective skill assessment. As technology continues to shape the landscape of medical education, the role of simulation in laparoscopic surgical training will undoubtedly play a pivotal role in shaping the next generation of skilled and confident surgeons.