Introduction:
Laparoscopic surgery, hailed for its minimally invasive nature, has transformed the landscape of surgical interventions. Despite its advantages, patients often grapple with postoperative pain, prompting a relentless quest for innovations in pain management. This article delves into the latest breakthroughs shaping the landscape of post-laparoscopic pain management, exploring targeted interventions, enhanced recovery protocols, and a paradigm shift towards personalized care.
The advent of laparoscopic surgery marked a significant departure from traditional open procedures. Characterized by smaller incisions, reduced tissue trauma, and quicker recovery times, laparoscopy has become the preferred method for various surgical interventions, spanning from cholecystectomy to colorectal procedures. However, the pursuit of excellence in patient care extends beyond the operating room, emphasizing the importance of effective postoperative pain management.
The Challenge of Post-Laparoscopic Pain:While laparoscopic surgery minimizes external trauma, it doesn't eliminate postoperative pain entirely. Patients commonly experience discomfort, primarily due to insufflation-related effects, residual pneumoperitoneum, and tissue manipulation during the procedure. The challenge lies in optimizing pain relief without compromising the benefits of minimally invasive surgery.
Enhanced Recovery After Surgery (ERAS) Protocols:One noteworthy innovation in post-laparoscopic pain management is the widespread adoption of Enhanced Recovery After Surgery (ERAS) protocols. ERAS emphasizes a multidisciplinary approach, integrating preoperative, intraoperative, and postoperative strategies to enhance recovery. Components such as preoperative counseling, optimized anesthesia techniques, and early ambulation contribute to reduced pain, decreased length of hospital stay, and faster return to normal activities.
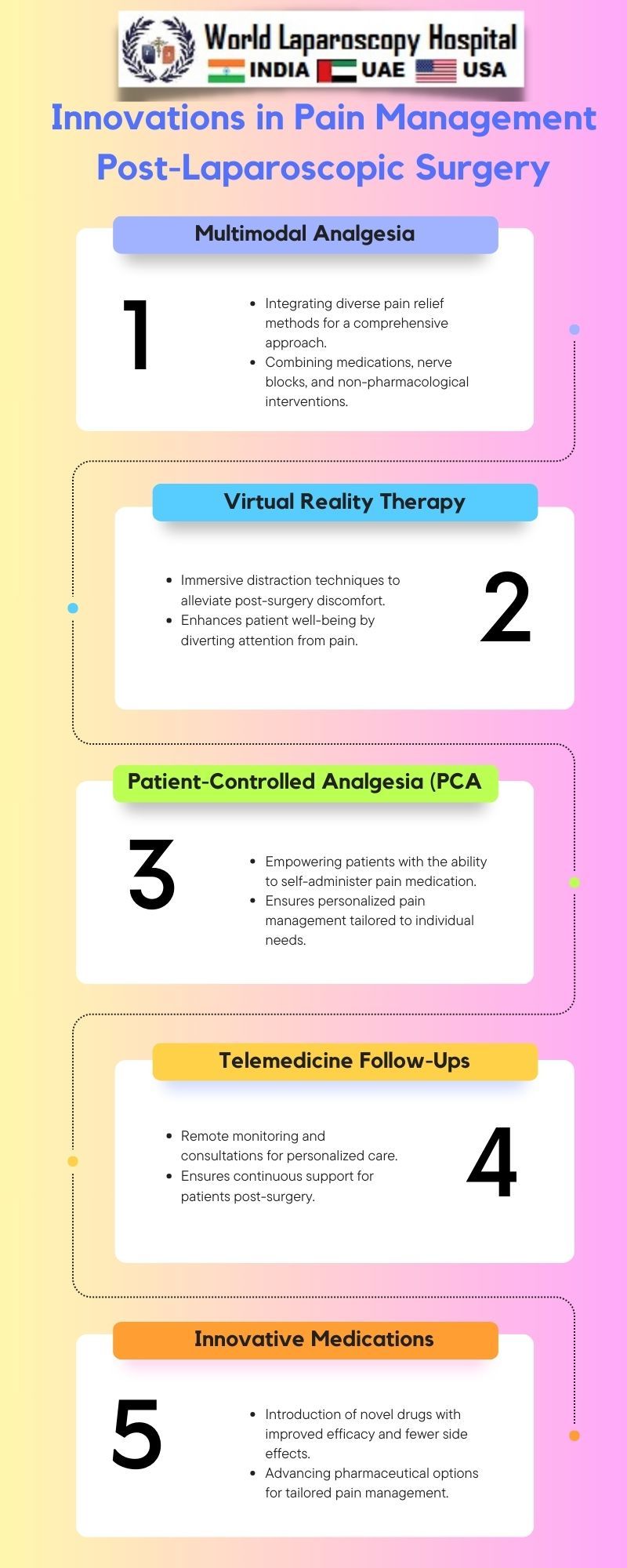
Minimizing Opioid Dependence:The opioid epidemic has prompted a critical reevaluation of postoperative pain management strategies. Innovations focus on minimizing opioid use while maintaining effective pain control. Multimodal analgesia, combining non-opioid medications such as NSAIDs and acetaminophen, has gained prominence. This approach not only reduces reliance on opioids but also mitigates their associated side effects, including sedation and respiratory depression.
Nerve Blocks and Regional Anesthesia:Precision in pain relief post-laparoscopic surgery has been elevated through the application of nerve blocks and regional anesthesia. Targeting specific nerves involved in the surgical site, these interventions provide localized pain control. Transversus abdominis plane (TAP) blocks, epidurals, and paravertebral blocks have emerged as effective options, offering prolonged pain relief and diminishing the need for systemic analgesics.
Intraperitoneal Local Anesthetics:Innovative techniques involve the administration of local anesthetics directly into the peritoneal cavity during laparoscopic procedures. This intraperitoneal approach addresses pain at its source, reducing visceral and somatic discomfort. Studies have shown that instilling local anesthetics, such as ropivacaine or bupivacaine, leads to improved pain scores, decreased opioid requirements, and enhanced patient satisfaction.
Non-Pharmacological Approaches:Beyond traditional pharmacological interventions, a holistic approach to pain management encompasses non-pharmacological strategies. Cognitive-behavioral therapy, acupuncture, and relaxation techniques contribute to a comprehensive pain management plan. Integrating these modalities not only addresses the physical aspect of pain but also considers the psychological and emotional dimensions, promoting a more holistic recovery.
Patient-Centered Care:Personalized pain management plans represent a paradigm shift towards patient-centered care. Tailoring interventions based on individual characteristics, preferences, and pain profiles enhances efficacy. Preoperative assessments that consider factors like pain sensitivity, anxiety levels, and previous pain experiences empower healthcare providers to create bespoke plans, fostering a patient-centric approach to post-laparoscopic pain relief.
Telemedicine in Postoperative Care:The integration of telemedicine has also impacted post-laparoscopic pain management. Remote monitoring allows healthcare providers to assess patients' recovery progress, address concerns, and modify pain management strategies as needed. Telemedicine enhances accessibility to care, particularly for patients in rural or remote locations, ensuring continuous support in the critical postoperative period.
Challenges and Future Directions:Despite these innovations, challenges persist. Standardizing protocols, overcoming barriers to implementing ERAS, and refining personalized pain management approaches require ongoing efforts. The future holds promise with the exploration of novel pharmacological agents, advanced technologies, and a deeper understanding of the neurobiology of pain, paving the way for even more effective post-laparoscopic pain management strategies.
Conclusion:
Innovations in post-laparoscopic pain management reflect a dynamic convergence of medical expertise, technological advancements, and a commitment to patient well-being. From ERAS protocols to nerve blocks and personalized care plans, the landscape is evolving to ensure that the benefits of minimally invasive surgery extend seamlessly into the realm of patient recovery. As research and technology continue to progress, the journey towards optimal post-laparoscopic pain management promises to be one of continued innovation and improved patient outcomes.