Different treatments have been proposed to corret this defect. Medical therapy with the use of oral contraceptives to reduce menstrual blood, hysteroscopy surgery to facilitate the drainage of blood and to reduce the local production and laparoscopic or vaginal surgery to correct the defect, trying to restore the normal anatomy of the istmical area. When performing Isthmocele repair surgery, regardless of the selected approach, the aim should be at treating the factors responsible for postmenstrual bleeding. Acting in this way will improve the patient's symptoms, solve the problem of infertility associated with impaired sperm transport and reduce chronic inflammation, which will improve the associated painful symptoms.
The hysteroscopic surgical isthmocele correction technique consists of four steps following Gubbini's recommendation. As previously mentioned, the difference with the technique proposed by Fabres lies in the resection of both the lower and upper fibrous arch.
The surgical technique is usually performed with resectoscopes of 26-27 fr after dilation of the cervical canal. Many authors prefer the use of smaller resectors or even mini-resectors that do not require prior cervical dilation. By not performing a previous cervical dilation, the normal anatomy of the isthmocele is not altered, better identifying the defect in its natural state without creating any artifact in the anatomical structures.
The steps to follow to perform an Ithmocele repair are the following:
1- Resection of the lower fibrous arch. The resection of this fibrous tissue that is responsible for the natural exit of the menstrual flow is performed. This anterior arc must be resected until the continuity of the anterior face is restored, making the defect flat, allowing visualization the isthmocele dome. By resecting this fibrous tissue, we prevent the isthmocele from acting as a reservoir of postmenstrual blood.
2- Resection of the posterior arch. Resecting the posterior arch reduces fibrous retraction and improves uterine contractility, a very important factor in cleaning the uterus after menstruation.
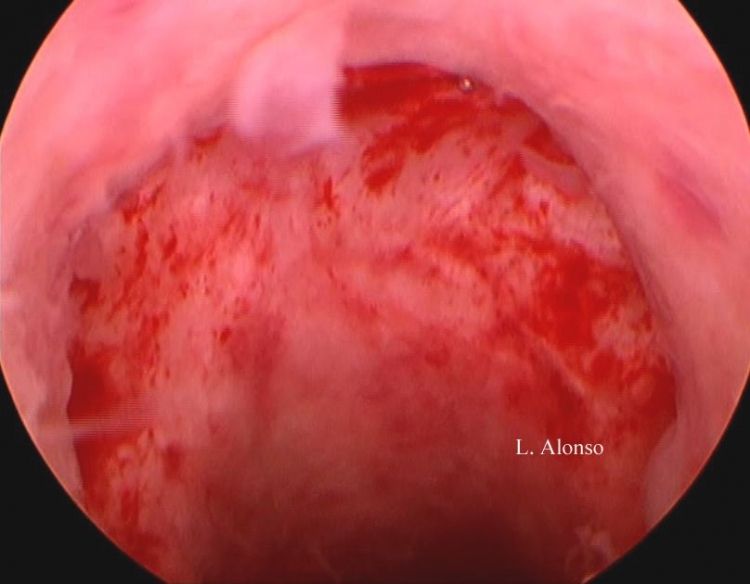
3- Superficial coagulation of the vessels at the bottom of the isthmocele. The objective is to reduce the production of menstrual blood and debris in situ derived from the inflammation and vascular fragility found at the bottom of the isthmocele. We must remember that deep 4- Closing the opening. Most authors use resorbable suture material in double layer for the closure of the myometrium. We have observed that it is easier if it is done first at the corners and then at the level of the center of the defect. These two layers are intended to achieve a greater thickness of residual myometrium thus eliminating the previous defect. Subsequently, the peritoneal closure is performed.
The laparoscopic correction technique requires a high skill level of laparoscopic surgery and a good laparoscopic suture technique, the most difficult step of the procedure is the dissection of the vesicouterine space. There is currently a consensus on choosing the laparoscopic repair technique when the thickness of the residual myometrium is less than 3 mm given that there is little safety margin of the residual myometrium increasing the chance of bladder injury if performed with a hysteroscopic approach.
CHOICE OF ROUTE FOR REPAIR
Surgical techniques for treating isthmocele can be divided into defect reparative with symptoms relief or symptomatic relief only.
Symptomatic surgery aims to improve the symptoms associated with isthmocele such as postmentrual bleeding, infertility and pain. This type of surgery is performed with an hysteroscopic approach which is not intended to repair the healing defect but simply to improve the associated symptoms.
Corrective or reparative surgery pursues the goal to repair the defect and restore the normal anatomy at the isthmic level. This type of surgery can be performed laparoscopically, robotically, combined or vaginally. The opening of the defect, the excision of the fibrous scar tissue from the edges and the closure of the defect by planes are the common points to these techniques.
It should be noted that not all isthmoceles are symptomatic, that not all are associated with postmenstrual bleeding or infertility and that surgery should be reserved only for symptomatic cases.
Recently an agreement of the scientific committee of the Global Congress on Hysteroscopy was published in which is stated that
the hysteroscopic approach represents a comfortable and safe option to treat this pathology when the residual endometrial thickness is at least in 3 mm. On the other hand, when the thickness of the residual myometrium is less than 3 mm, the
preferred route should be laparoscopic, robotic, vaginal or combined, due to the risk of uterine perforation and bladder injury if the hysteroscopic route is chosen .
Isthmocele is a medical condition that occurs when a pouch or pocket develops in the uterine wall after a cesarean section (C-section) delivery. The condition can lead to heavy menstrual bleeding, pelvic pain, and infertility. Hysteroscopic and laparoscopic surgeries are two minimally invasive surgical techniques that can be used to treat isthmocele. In this essay, we will explore isthmocele, hysteroscopic surgery, and laparoscopic surgery, and how they can be used to treat isthmocele.
Isthmocele:
Isthmocele is a condition that occurs when a pouch or pocket develops in the uterine wall after a cesarean section delivery. The condition is caused by incomplete healing of the uterine incision after C-section delivery. The pocket or pouch can fill with menstrual blood and cause heavy menstrual bleeding, pelvic pain, and infertility.
Isthmocele is typically diagnosed using hysteroscopy, a minimally invasive surgical technique that involves inserting a thin, flexible tube with a camera and light source into the uterus. Hysteroscopy allows the surgeon to view the inside of the uterus and identify the presence of an isthmocele.
Hysteroscopic Surgery:
Hysteroscopic surgery is a minimally invasive surgical technique that is used to diagnose and treat conditions of the uterus, such as isthmocele. The procedure involves inserting a thin, flexible tube with a camera and light source into the uterus through the vagina and cervix. The surgeon can view the inside of the uterus on a monitor and use specialized instruments to perform surgery.
Hysteroscopic surgery can be used to treat isthmocele by removing the pouch or pocket that has formed in the uterine wall. The surgeon can use specialized instruments, such as a hysteroscopic resectoscope, to remove the pouch or pocket and create a smooth uterine surface. This can help to alleviate the symptoms of isthmocele, such as heavy menstrual bleeding and pelvic pain.
One of the benefits of hysteroscopic surgery is that it is minimally invasive and does not require any incisions. This can result in a shorter recovery time, less pain, and fewer complications than traditional open surgery. Hysteroscopic surgery can also be performed on an outpatient basis, which means that the patient can go home the same day as the surgery.
Laparoscopic Surgery:
Laparoscopic surgery is a minimally invasive surgical technique that is used to diagnose and treat a wide range of medical conditions, including isthmocele. The procedure involves making small incisions in the abdomen and inserting a thin, flexible tube with a camera and light source into the abdominal cavity. The surgeon can view the inside of the abdomen on a monitor and use specialized instruments to perform surgery.
Laparoscopic surgery can be used to treat isthmocele by removing the pouch or pocket that has formed in the uterine wall. The surgeon can use specialized instruments, such as laparoscopic scissors or a laparoscopic resectoscope, to remove the pouch or pocket and create a smooth uterine surface. Laparoscopic surgery can also be used to repair any damage to the uterine wall that may have occurred during the C-section delivery.
One of the benefits of laparoscopic surgery is that it is minimally invasive and results in less pain, fewer complications, and a shorter recovery time than traditional open surgery. Laparoscopic surgery can also be performed on an outpatient basis, which means that the patient can go home the same day as the surgery.
Hysteroscopic vs. Laparoscopic Surgery:
Both hysteroscopic and laparoscopic surgerycan be used to treat isthmocele, and the choice of surgical technique depends on the individual case. In general, hysteroscopic surgery is preferred for small to moderate isthmoceles, while laparoscopic surgery is preferred for larger isthmoceles or cases where there is damage to the uterine wall that needs to be repaired.
Hysteroscopic surgery is less invasive than laparoscopic surgery and does not require any incisions, which can result in a shorter recovery time and fewer complications. However, hysteroscopic surgery is limited to treating conditions inside the uterus and cannot be used to repair any damage to the uterine wall.
Laparoscopic surgery is more invasive than hysteroscopic surgery and requires small incisions in the abdomen. However, laparoscopic surgery can be used to treat conditions both inside and outside the uterus, including any damage to the uterine wall that may have occurred during the C-section delivery.
Conclusion:
Isthmocele is a medical condition that can occur after a cesarean section delivery and can lead to heavy menstrual bleeding, pelvic pain, and infertility. Hysteroscopic and laparoscopic surgeries are two minimally invasive surgical techniques that can be used to treat isthmocele.
Hysteroscopic surgery involves inserting a thin, flexible tube with a camera and light source into the uterus through the vagina and cervix. The surgeon can view the inside of the uterus on a monitor and use specialized instruments to remove the pouch or pocket that has formed in the uterine wall.
Laparoscopic surgery involves making small incisions in the abdomen and inserting a thin, flexible tube with a camera and light source into the abdominal cavity. The surgeon can view the inside of the abdomen on a monitor and use specialized instruments to remove the pouch or pocket that has formed in the uterine wall and repair any damage to the uterine wall.
The choice of surgical technique depends on the individual case, with hysteroscopic surgery preferred for small to moderate isthmoceles and laparoscopic surgery preferred for larger isthmoceles or cases where there is damage to the uterine wall that needs to be repaired.
Both hysteroscopic and laparoscopic surgeries are minimally invasive and can result in a shorter recovery time, less pain, and fewer complications than traditional open surgery. Patients who are considering hysteroscopic or laparoscopic surgery to treat isthmocele should consult with their doctor to determine which surgical technique is best for their individual case.