Ebubekir UNLU. MD; M.G.O; D. MAS.
Consultant Gynaecologist, Obstetrician and Laparoscopic Surgeon
Dunya Maternity Hospital
Diyarbakir, Turkey
Member OF TURKISH Medical Association
Member of World Association of Laparoscopic Surgeons
Prof. Dr. R. K. Mishra; M.MAS; MRCS.
Senior Consultant Laparoscopic Surgeon
Director, World Laparoscopy Hospital, Gurugram, NCR Delhi
Member World Association of Laparoscopic Surgeon (WALS)
Member Indian Association of Gastrointestinal Endosurgeons (IAGES)
Member Society of American Gastrointestinal and Endoscopic Surgeons (SAGES)
Project submitted towards completion of Diploma in Minimal Access Surgery,World Laparoscopy Hospital, Gurugram, NCR Delhi, India 110018.
ABSTRACT:
If pain in the middle pelvic area persists, a procedure presacral neurectomy is a proven beneficial procedure. With this procedure the surgeon uses either electricity or lasers to destroy tissue containing pain-causing nerves, deep in the pelvic region. Studies indicate that regardless of the severity of the case, pain is reduced in 50% to 90% of patients. The present study was undertaken to evaluate the efficacy of presacral neurectomy for the treatment of Chronic Pelvic Pain in Female.
KEY WORDS
Laparoscopic Presacral Neurectomy [LPSN], Presacral Neurectomy [PSN], Chronic Pelvic Pain [CPP], Conventional Presacral Neurectomy [CPSN], Laparoscopic Uterine Nerve Ablation [LUNA], Uterosacral Nerve Ablation [UNA].
INTRODUCTION
Approximately 20% of all patient visits to gynaecologist are suffering from pelvic pain. Pelvic pain can arise from a number of observable disorders or functional disorders in which obvious pathology is not present. The acute onset of pelvic pain is almost always related to an episodic event, such as ovulation, a rupturing ovarian cyst, or possible an ectopic pregnancy. CPP on the other hand is usually related to an evolving disorder such as endometriosis, pelvic adhesions, a slowly enlarging fibroid tumour or an ovarian cyst. In many cases where no definitive cause of chronic pain in females of reproductive age group is established, the PSN is one of the good options. New standards have been established for various indications. Patient comfort is a great consideration in the 21st century. The acquisition of recent technology and skills now affords a better choice of the mode of surgery. This document reviews the recent advances in treatment technique applicable to LPSN, examines the literature, and suggests guidelines for laparoscopic intervention in patients with CPP.
AIMS:
The aim of this study was to compare the effectiveness and safety of LPSN versus other procedures in the treatment of CPP. The following parameters were evaluated for Laparoscopic Presacral Neurectomy [LPSN] and Other Surgical Procedures like [LUNA, Classic Open Presacral Neurectomy or Hysterectomy].
1. Method of patient selection
2. Operative technique
3. Operating time.
4. Intra-operative and postoperative complications.
5. Postoperative pain and amount of narcotic used.
6. Postoperative morbidity.
7. Hospital stay.
8. Cost effectiveness and
9. Quality of life analyses
Materials and Methods
A literature search was performed using search engine Google & Online Springer Library facility available at World Laparoscopy Hospital.
The following search terms were used:
"Laparoscopic Presacral Neurectomy, Chronic Pelvic Pain, Conventional Presacral Neurectomy".Selected papers were screened for further references, operative procedure were selected only if they are universally accepted procedures and the Institution where the study was done is specialized institution for laparoscopic surgery.
ABDOMINAL PAIN IN FEMALE:
A lack of physical findings does not negate the significance of a patient's pain, and normal examination results do not preclude the possibility of finding pelvic pathology [1]. Many times chronic pelvic pain can be produced by a non noxious stimulus [allodynia], which radiates into areas not directly involved in the original site of tissue injury.
Gynecologic Extra uterine CAUSES OF CHRONIC PELVIC PAIN
Most common extra uterine causes of chronic pelvic pain in Females are:
- Adhesion
- Adnexial cysts
- Chronic ectopic pregnancy
- Chlamydia endometritis
- Salpengitis
- Endometritis
- Endosalpengitis
- Ovarian retention syndrome
- Pelvic congestion syndrome
- Tuberculous salpengitis
- Irritable bowel syndrome
- Hernias and
- Recurrent Appendicitis
GynAecologic UterinE CAUSES OF CHRONIC PELVIC PAIN:
- Adenomyosis
- Atypical dysmenorrhoea
- Ovulatory pain
- Cervical stenosis
- Chronic endometritis
- Polyps
- Intrauterine devices
- Symptomatic genital prolapse.
The diagnostic laparoscopy is one of the commonly performed procedures for finding etiology of pelvic pain [Acute or Chronic]. In one of the study performed by Howard FM 2627 diagnostic laparoscopy was performed for pelvic pain with following results [2].
| Number of Patients | With Chronic Pelvic Pain | Without Chronic Pelvic Pain |
|---|---|---|
| Total Number of Patient | 1524 | 1103 |
| Number of visible pathology | 35% | 72% |
| Endometriosis * | 33% | 5% |
| Chronic PID | 5% | 1% |
| Leiyomyomas | <1% | 2% |
*Endometriosis should be established histologically there is no correlation between histologic and visual findings [3].
SURGICAL ANATOMY:

Presacral Sandwich; Peritoneum {Loose connective tissue, fat and hypogastric plexus, middle sacral vessels Periosteum}
Pathophysiology of Complex Pelvic Pain Syndromes in Female
The pathophysiology of visceral pain syndromes is:
- Silent C- fibers becoming activated
- Biochemical up-regulation due to neuroplasticity.
- Visceral Pain [Parasympathetic and sympathetic]
- Chronic Visceral pains are characteristically
- Unpleasant
- Anxiety provoking
- Intense
- Diffuse
- Variable
PAIN PERCEPTION: THE GENDER BIAS ?
Females report pain perception more intensely than males [4]. Females prefer emotion focused coping while males prefer sensory focused coping strategies to deal with pain, and there are other factors in female pelvic pain, gonadal hormones, genetic factors, family history, mood disturbance, coping profiles and sex role.
Management of Chronic Abdominal Pain in Female:
General principles:
v Attempt to prevent CPP Syndrome.
v Early treatment
v Adequate pain relief with poly pharmacy if necessary
Medical management of Pelvic pain:
While these treatments are very successful there is still a 20-25% failure rate and surgery has been an option for cases of dysmenorrhoea that fail to respond to medical therapy.
- NSAID,
- weak opiod
- non opiod
- short acting [PARACETAMOL with codein]
- Long acting [oxycontin]
Surgical management of Pelvic pain:
Neuro Ablative Procedures
Most commonly performed Neuro abalative procedures are:
- Laparoscopic Presacral Neurectomy [LPSN]
- Laparoscopic Uterosacral Nerve Ablation [LUNA]
Adjunctive SURGICAL Procedures:
Surgical interventions for CPP include:
- Uterine suspension
- Ovariopexy
- Cystoscopy with Hydrotension
- Hernia repair
Multidisciplinary treatment:
- Behavior modification
- Physical therapym
- Surgical intervention if indicated
- Pharmacological therapy
Laparoscopic Presacral Neurectomy [LPSN]
General Management of CPP:
- Patient education "It's not Cancer"
- Establish realistic goals
- Multi component sources of pain
Preoperative Measures
- Catheterization
- Bowel preparation
- Routine Anesthetic and Medical checkups
- Peglac powder-1 sachet with water a night prior to surgery
Patient position
Steep trendelenburg with 15- 20 degree head down position in supine position.
SURGICAL TASK:
Laparoscopy usually done under general anaesthesia and involves the following: Carbon dioxide gas is injected into the abdomen, distending it and pushing the the bowel away so that physician has a wider view. The procedure requires making small incision at the navel and above the pubic bone. The laparoscope is inserted through the incision at the navel [the umbilical incision]. Two other working port is introduced 5 cm lateral on either side of the umbilicus. A probe is then inserted through the second incision allowing the physician to directly view the outside surface of uterus, fallopian tubes, and ovaries. One or two additional port can be made on either side of the lower abdomen through these incisions. Parietal peritoneum is gently opened; the sympathetic and parasympathetic fibers and ganglions are very close under the peritoneum.
Presacral neurectomy is performed on the anterior aspects of vertebral bodies L5 and S1. Adjacent vital structures which could be injured include the common iliac veins, the ureter, and the sigmoid mesentery. The patient is placed in steep Trendelenburg position and rolled to the left, displacing the sigmoid colon laterally. A blunt probe also used to effectively remove the sigmoid from the operative site.
Damage to the left common iliac vein may occur during laparoscopic PSN. The iliac arteries have thicker walls and are more resistant to damage. The risk of damage to the vein can be reduced by identifying its retroperitoneal location by the "waterbed sign." To elicit this sign, the peritoneum between the common iliac arteries is tapped with a blunt probe, and the location of large venous structures will be apparent by a bouncing retroperitoneal fluctance, indicating the presence of blood under low pressure. Sometimes the retroperitoneal venous structures can be seen through the peritoneum, but it is still wise to elicit this sign. The peritoneum caudal to the vein is grasped, elevated and incised transversely from the edge of the sigmoid mesentery on the left to the common iliac vessels on the right.Elevation of the peritoneum moves it away from any retroperitoneal vessels.
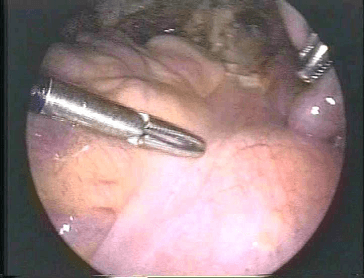
Picture: Incision point for Presacral Neurectomy
One concept which can increase the risk of damage to either ureter during a PSN is that a PSN is properly performed from "ureter to ureter". This errant notion has no basis in the published literature14-22 or anatomy books, since the presacral neural plexus is located in midline or just slightly to the left of midline. It is not necessary to identify the left ureter during a PSN. The left ureter is hidden beneath the mesentery of the sigmoid colon and actually lies lateral to the mesentery. The left ureter can be seen only with difficulty if the mesentery is retracted laterally. Thus, if the left ureter is visible from the operative field, the dissection has been carried too far to the left. Dissection to try to find the left ureter, risks damage to the vessels of the mesentery. Since the neural fibers of the presacral plexus are located between the common iliac vessels, the dissection during a PSN should not usually come to lie in the vicinity of the left ureter.
Blunt dissection is used at each angle of the peritoneal incision to create windows towards the periosteum of L5 L6. This also defines the position of the common iliac veins. The next step is to grasp and elevate the presacral tissue and transect it in successively deeper layers. As this dissection proceeds, sizable presacral vessels may come into view. Since the presacral plexus passes anterior to these vessels, it is not necessary to transect any vessels and expose bare periosteum if the tissue anterior to the vessels is removed. Blunt dissection is then used to peel the presacral plexus off the underlying periosteum and any presacral vessels. The overlying peritoneum is stripped away and the plexus is transected caudally and the specimen removed. The sigmoid colon lies just beyond the caudal peritoneal edge and could potentially be injured during final transection of the plexus if care is not taken. PSN is most safely performed with some type of contained surgical energy, such as electrosurgery or sharp dissection, rather than surgical energy with overstrike potential, such as CO2 laser vaporization or argon beam coagulator. The cavitational ultrasonic surgical aspirator's results are also good for PSN [6].
Laparoscopic Uterosacral Nerve Ablation [LUNA]:
![Line of incision for Laparoscopic Uterosacral Nerve Abalation [LUNA]](presac/image005.png)
Picture: Line of incision for Laparoscopic Uterosacral Nerve Abalation [LUNA]
Laparoscopic uterosacral nerve ablation [LUNA] may be used to incise the nerves and relax the ligaments that attach to the bottom of the uterus. In one systematic review, there were no differences in pain relief between women who had the procedure and those who didn't. Some small studies have reported benefits. In all, evidence is lacking on the value of this procedure and there are some risks to it [13].
Chronic pelvic pain in women due to hernias may be misdiagnosed by practicing clinicians. These fascial defects, their symptoms, physical findings, and proper treatment must be known in order to help women experiencing this form of chronic pelvic pain.
The study included 264 patients referred to a chronic pelvic pain clinic, who underwent 386 laparoscopic surgical repairs of hernial defects. Laparoscopic treatment of hernia pain in women is effective in relieving chronic pain and has a low recurrence and complication rate in the hands of experienced. Not all hernias are symptomatic. In one study, 4of 54 [7%] inguinal hernias in women diagnosed laparoscopically were producing no symptoms [8, 31].
Adjunctive SURGICAL Procedures:
- Appendicectomy: Appendiceal pathologyy does exist and can be the cause of chronic lower abdominal pain. In five recent reports appendectomy resulted in relief of symptoms of right lower quadrant pain in selected patients. In addition there does not appear to be a correlation. In five recent reports appendectomy resulted in relief of symptoms of right lower quadrant pain in selected patients [9, 10]
- Resection or Vaporization of vulvar / vestibular tissue for human papillioma virus [HPV] induced or chronic vulvodynia / vestibulitis.
- Cervical dilation for stenosis for cervix of uterus.
- Hysteroscopic resection for intracavitary or submucous myomas or intracavitary polyps.
- Myomectomy or myolysis for symptomatic Intramural, subserosal or pedunculated myomas.
- Adhesiolysis for peritubular and periovarian adhesions, and enterolysis for bowel adhesions, Adhesiolysis for all thick adhesions in areas of pain as well as thin adhesions affecting critical structures such as ovaries and tubes.
- Salpingectomy or neosalpingostomy for symptomatic hydrosalpinx.
- Ovarian treatment for symptomatic ovarian pain.
- Resection of endometriosis from all surfaces including removal from bladder and bowel as well as from the rectovaginal septal space. Complete resection of all disease in a debulking operation is essential.
- Appendectomy for symptoms of chronic appendicitis, and chronic right lower quadrant pain.
- Uterine suspension for symptoms of collision dyspareunia, pelvic congestion, severe dysmenorrhea, cul-de sac endometriosis.
- Repair of all hernia defects whether sciatic, inguinal, femoral, Spigelian, ventral or incisional.
- Hysterectomy if relief has not been achieved by organ-preserving surgery such as resection of all endometriosis and presacral neurectomy, or the central pain continues to be disabling. Before such a radical step is taken, MRI of the uterus to confirm presence of adenomyosis may be helpful, trigger point injection therapy for myofascial pain and dysfunction in pelvic and abdominal muscles [5].
With application of all currently available laparoscopic modalities, 80% of women with chronic pelvic pain will report a decrease of pain to tolerable levels, a significant average reduction which is maintained in3-year follow up [5].
DISCUSSION:
Laparoscopic uterosacral nerve ablation [LUNA] may be used to sever nerves and relax the ligaments that attach to the bottom of the uterus. In one systematic review, there were no differences in pain relief between women who had the procedure and those who didn't. Some small studies have reported benefits. In all, evidence is lacking on the value of this procedure and there are some risks to it. If pain in the middle pelvic area persists, a procedure called presacral neurectomy may be beneficial [13].
With application of all currently available laparoscopic modalities, 80% of women with chronic pelvic pain will report a decrease of pain to tolerable levels [9, 14]. The comparison between UNA with presacral neurectomy [PSN] for primary dysmenorrhoea showed no significant difference in pain relief in the short term, however long term PSN was shown to be significantly more effective [14]. For the treatment of secondary dysmenorrhoea the identified RCTs addressed only endometriosis. The treatment of UNA combined with surgical treatment of endometrial implants versus surgical treatment of endometriosis alone showed that the addition of UNA did not aid pain relief. For PSN combined with endometriosis treatment versus endometriosis treatment alone there was also no overall difference in pain relief, although the data suggests a significant difference in relief of midline abdominal pain. Adverse events were significantly more common for presacral neurectomy, however the majority were complications such as constipation, which may spontaneously improve.
Long-term outcome of laparoscopic presacral neurectomy is satisfactory in the majority of patients. The stage of endometriosis is not related directly to the degree of pain improvement achieved. Presacral neurectomy can be performed safely and efficiently by laparoscopy and is a valuable alternative treatment for pelvic pain [14,15,16].
The comparison of laparoscopic uterosacral nerve ablation with presacral neurectomy for primary dysmenorrhea showed that at 12 months follow-up, presacral neurectomy was more effective. In secondary dysmenorrhea, along with laparoscopic surgical treatment of endometriosis, the addition of laparoscopic uterosacral nerve ablation did not improve the pain relief, while presacral neurectomy did. Adverse events were more common for presacral neurectomy than procedures without presacral neurectomy [14]. For the treatment of primary dysmenorrhoea there was some evidence of the effectiveness of laparoscopic uterine nerve ablation [LUNA] when compared to a control or no treatment. The comparison between LUNA and laparoscopic presacral neurectomy [LPSN] for primary dysmenorrhoea showed no significant difference in pain relief in the short term. However; long-term LPSN was shown to be significantly more effective than LUNA. For the treatment of secondary dysmenorrhoea six identified RCTs addressed endometriosis and one included women with uterine myomas. The treatment of LUNA combined with surgical treatment of endometrial implants versus surgical treatment of endometriosis alone showed that the addition of LUNA did not aid pain relief. For PSN combined with endometriosis treatment versus endometriosis treatment alone there was an overall difference in pain relief although the data suggests this may be specific to laparoscopy and for midline abdominal pain only [15].
In one literature author has reviewed records of 655 patients receiving laparoscopic conservative surgery and laparoscopic presacral neurectomy for diagnoses including adenomyosis with dysmenorrhea [n = 55], moderate and severe endometriosis with dysmenorrhea [n = 127], minimal and mild endometriosis with dysmenorrhea [n = 208], primary dysmenorrhea [n = 99], and chronic pelvic pain with or without pathologic disease [n = 166]. Pain relief was evaluated at least 12 months postoperatively. RESULTS: Pain relief was evaluated in 527 patients. Significant pain relief, no pain or mild pain requiring no medication was found in 22 [52%] of 42 women with adenomyosis. Pain relief was in 75 [73%] of 103 patients with moderate to severe endometriosis with dysmenorrhea. in 123 [75%] of 164 with minimal to mild endometriosis with dysmenorrhea, in 64 [77%] of 83 with primary dysmenorrhea, and in 84 [62%] of 135 with chronic pelvic pain. In addition 485 [74%] of the 655 patients complained of constipation after laparoscopic presacral neurectomy, which was relieved easily by medication. Presacral neurectomy can be performed safely and efficiently by laparoscopy and is a valuable alternative treatment for pelvic pain [17].
| Procedure | Relief in Pain in Percentage |
|---|---|
| LPSN | Pain relief after 6 month 87.3 %, Pain relief after 12 month 85.7 %. |
| LUNA | Pain relief 25% |
| Luna and endometriosis extirpation | Pain relief 75% |
| Only endometriosis extirpation | Pain relief 74% |
| Endometriosis ablation | Pain relief after 6 month 56%, Pain relief after 12 month 54%. |
| Hysterectomy | Pain relief 50% with 50% Recurrence |
Table1: Comparison in CPP reduction with various procedures.
Advantage of Laparoscopic Presacral Neurectomy:
Laparoscopy VS Laparotomy:
PSN with both laparoscopy and laparotomy are effective, but there are differences. Some experts believe that laparoscopy surgery should be the treatment of choice for women with endometriosis. Laparoscopy is now the gold standard treatment for endometriosis .The goal of conservative surgery is to aggressively remove as many endometrial implants and cysts as possible without causing surgical scarring and subsequent adhesions that could cause fertility problems. Studies report pain reduction after surgery in more than 60% of women. Conservative surgery, however, can miss microscopic implants that may continue to cause pain and other symptoms after the procedure in one study, laparoscopy achieved pain relief in over 62% of women [7].
Pregnancy rate
It is found that pregnancy rates in patients who undergone LPSN with endometriosis ablation was higher (50%) than patients who were gone for open PSN and endometriosis ablation (20%) [32].
Laparoscopy and Adhesions
Laparoscopic surgical techniques lead to fewer intra-abdominal adhesions by reducing tissue trauma, which in turn reduces circulating inflammatory mediators [20].
Dysmenorrhea:
UNA with presacral neurectomy [PSN] for primary dysmenorrhoea showed no significant difference in pain relief in the short term, however long term PSN was shown to be significantly more effective. For the treatment of secondary dysmenorrhoea the identified RCTs addressed only endometriosis. The treatment of UNA combined with surgical treatment of endometrial implants versus surgical treatment of endometriosis alone showed that the addition of UNA did not aid pain relief. For PSN combined with endometriosis treatment versus endometriosis treatment alone there was also no overall difference in pain relief, although the data suggests a significant difference in relief of midline abdominal pain. Adverse events were significantly more common for presacral neurectomy, however the majority were mild complications such as constipation, which may spontaneously improve [21].
Laparoscopy and Immunity
All surgery and anaesthesia can cause depression of cell-mediated immunity in the postoperative period, including reduction in the number of circulating lymphocytes, impairment of natural killer cell cytotoxicity, depression of T cell proliferation, and diminished neutrophil function. Animal and clinical studies have shown that laparoscopic surgery impairs a patient's immune state less than open surgery. Cell-mediated immunity is less impaired after laparoscopic operation than after open. Interleukin 6 levels were less in a study on newborn infants undergoing laparoscopic procedures when compared to open [20]
Cost effectiveness of LPSN
Debate still exists about the cost comparison between laparoscopic and open surgery. Most surgeons have the opinion that laparoscopic procedure is cost effective. It may be more expensive for the hospital but it offers cost savings to society as a result of faster return to work [22].
ENDOMETRIOSIS AND LPSN
If LPSN and Endometriosis is combined together it has many advantages. Most common causes of pelvic pain is endometriosis [8]. Laparoscopy is considered as gold standard for the treatment of endometriosis. Deependometriosis in cul-de sac in which the approach by laparatomy is difficult laparoscopy is benificial.
The general advantages of laparoscopy which include same day diagnosis and treatment, short hospitalisation, rapid recuperation, superior cosmetics, excellent patient acceptance, cost effectiveness, and results at least equal to laparotomy.
The operative advantages of a laparoscopic approach to the cul-de-sac include:
- Easy intraoperative access to the rectum and vagina
- A magnification source which is easier to manipulate then an operating microscope so that the surgeon can get a very close view of lesions involving the deep pelvis and rectum
- The ability to perform an underwater examination at the end of the procedure during which all blood clot is evacuated and complete hemostasis obtained.
To describe optimal procedures and preliminary results for videolaparoscopic presacral neurectomy as part of the surgical treatment of endometriosis associated with intractable dysmenorrhoea. Observational study was performed with follow up for at least one year. Eighty five women (18-45 years) with endometriosis and intractable pain, referred because medical and surgical management had failed. Subjects without a central (midline) component to their discomfort were excluded. Excision and vaporization of endometriotic pathology was followed by presacral neurectomy. During surgery, severity of endometriosis was assessed using revised American Fertility Society scoring. Overall pelvic pain and dysmenorrhoea relief were determined by office visit, telephone interview and questionnaire at a minimum of one year postoperatively. There were no operative complications and all women left hospital within 24 h of surgery. Overall pain relief was reported by 49 [94%] of 52 patients followed. The other three subjects noted no pain abatement. Dysmenorrhoea was reduced in 48 [92%] whereas four [8%] women claimed no relief. Laparoscopic presacral neurectomy is an option for treating dysmenorrhoea and pelvic pain in selected women, but is indicated only if medical management has failed. Videolaparoscopic presacral neurectomy using the CO2 laser is safe in trained hands. Pain relief achieved is within the range reported for laparotomy [23].
Cancer and Pain
A 70% mean reduction in chronic cancer related pelvic pain was achieved with neurolytic blockade of the superior hypogastric nerve plexus, confirming a role for presacral neurectomy in the treatment of pelvic pain. Surgical interruption of the hypogastric plexus [pre-sacral neurectomy] is a well-accepted procedure that has been demonstrated to relieve a variety of painful pelvic conditions, predominantly of pain associated with gynaecological malignancies [24].
Role of Hysterectomy
Hysterectomy with bilateral oophorectomy was effective in women who failed to obtain long-term relief of pain with oral contraceptives and nonsteroidal anti-inflammatory medications. These women were diagnosed with pelvic congestion syndrome, although pathology revealed that 25% had adenomyosis. Of 99 women who underwent hysterectomy for chronic pelvic pain of at least 6 months duration, and whose disease by symptoms and examination was confined to the uterus, 77.8% had significant improvement and 22.2% had persistent pain.
Disadvantages of Presacral Neurectomy
Operation Period:
Generally all laparoscopic procedures are more time consuming for the following reasons.
- Inherent nature of slow manoeuvre of laparoscopic techniques.
- Time taken by careful slow insufflations.
- Routine diagnostic laparoscopy before starting any laparoscopic procedure.
Laparoscopy and risk of anaesthesia:
The general anaesthesia and the pneumoperitoneum required as part of the laparoscopic procedure does increase risk in certain patient groups [33].
Most surgeons would not recommend LPSN in:
- Patients with cardiac diseases and COPD Should not be considered a good candidate for L PSN.
- In patients who have had previous lower abdominal surgery LPSN may also be more difficult
- The elderly May also be at increased risk for complications with general anaesthesia combined with pneumoperitoneum.
- Those with lowered cardio-pulmonary reserve
- With regard to the consequences of the pneumoperitoneum and a longer operative time.
Specific complications of LPSN:
Long-term complications with LPSN are uncommon. An occasional patient will report alteration of the sensation of bladder fullness due to interruption of sympathetic fibers carrying bladder sensation. These patients seem to urinate normally, do not have increased urinary infections, and are not incontinent. Some patients may report a decrease of vaginal lubrication with sexual arousal. Constipation is not a predictable consequence of presacral neurectomy since the parasympathetic fibers which stimulate evacuation of the rectosigmoid pass through the inferior hypogastric plexus [also termed the pelvic plexus] and are not interrupted by PSN.
shown evidence efficacy similar to that seen after laparotomy PSN Studies indicate that of long-term In patients undergoing laparoscopic PSN, follow-up observation has regardless of the severity of the case, pain is reduced in 50% to 90% of patients and the benefit can last for more than a year. In one study, major complications occurred in 0.6% of cases. Constipation is a very common side effect and is easily relieved with medication.[7]
Pelvic surgery may cause parasympathetic constipation in 10%-15% of patients [15]which may spontaneously improve or is easily relieved with medications [25,26] diarrhea and urinary problems. There were four major complications [0.6%] that required further surgery, including injury of the right internal iliac artery [n = 1] and chylous ascites [n = 3]. Three cases [0.5%] had laceration of the middle
General complications:
In one study, major complications occurred in 0.6% of cases [39]. A series of 2140 operative laparoscopies were reviewed in a retrospective study of patient records. Operative laparoscopy included minor procedures, minimal adhesiolysis, destruction of minimal endometriosis foci, ovarian biopsy, ovarian puncture, tubal sterilization, major laparoscopic surgery extended adhesiolysis, tuboplasties, uterine suspension, treatment for ectopic pregnancy, salpingitis, ovarian cyst, moderate and severe endometriosis, and advanced laparoscopic surgery hysterectomy, myomectomy, bladder neck suspension.At another studies, two major vascular complications, 3 intestinal injuries, 1 anesthesiological complication, and 4 urinary tract injuries occurred. Two minor and 5 postoperative complications were noted. The overall complication rate was 17/2140 i.e. 0.79%. The major complication rate was 10/2140 i.e. 0.46% [27].
Future prospects of laparoscopic PSN:
In the future, remote handling technology will overcome some ofthe manipulative restriction of current instruments. There is no doubt that 20 years from now some surgeons will be operating exclusively via a computer interface controlling a master-slave manipulator. But the future of any new technology depends upon applications and training[28].
Insufficiency:
There was also a suggestion that PSN benefits the midline component of endometriosis pain but not the adnexal or lateral component. In one study when all laparoscopic procedures like uterine colposuspension, Ovariopexy, Cystoscopy with hydrotension, and LPSN were employed fully, 20% of patients experience unsatisfactory results. The main reason perceived for this dissatisfaction was insufficient psychological preparedness of the patient. Thus, it is important to provide sufficient psychological support to patients of CPP. Multidisciplinary approach and individualisation of every case is necessary for this reason [11, 29 ,30]
conclusion:
PSN is beneficial for some women with predominantly midline pelvic pain. Indicated surgical interventions for chronic pelvic pain are best performed with minimal invasive surgery earlier rather than later. Adequate post operative pain relief and behavioral modification improve long term results. Chronic Pelvic Pain in female should always be dealt with multi-disciplinary approach. LPSN is safe, and can provide less postoperative morbidity in experienced hands, as open PSN. LPSN is a useful method for reducing hospital stay, complications and return to normal activity. With better training in minimal access surgery now available, the time has arrived for it to take its place in the surgeon's repertoire.
References:
[1] ACOG Practice Bulletin,Clinical Manegement Guidelines for Obstetricients, Number 51,March2004 F. Howard
[2] C. Paul Perry, MD, FACOG; Pelvic Pain Center, Brookwood Women's Medical Center, Birmingham, AL
[3] Endometriosis: Correlation between histologic and visual findings at laparoscopy. Obst Gynec. 184:14-13 ; 2001 Walter AJ, Hentz JG,et al.
[4] Keog E,Herdenfeldt M, Gender ,Coping and the Perception of Pain Pain 97 ;195-201;2002
[5] JLSL, Vol.9 Number 3,July-September 2005 pp 249-251
[6] A Simplified Method of Laparoscopic Presacral Neurectomy for the Treatment of associated with open surgery, may encourage more women to obtain relief www.nezhat.com/oplap_abst.htm, Camran Nezhat, MD, Farr Nezhat, MD; British Journal of Obstetrics & Gynaecology, 8/92, Vol 99, pp 659-63 was 46
[7] Miranda, Christian; Carvail Antonio R JLSL vol 7 number 1 January-march 2003 pp 53-58
[8] Hernias as a Cause of Chronic Pelvic Pain in WomenJSLS 2006,10:212-215, C. Paul Perry MD, Juan Diego Villegas Echeverri, MD
[9] Source: JSLS, Journal of the Society of Laparoendoscopic Surgeons, Volume 2,Number 2,April-June1998, pp. 129-139.Pelvic Surgical Treatment for Chronic Pelvic Pain : Carter, James E.
[10] Strigo IA, Bushnell MC, Bovin M, Duncan Gh. Psychophysical analysis of visceral and coetaneous pain in human subjects. Pain 97; 235-246:2006
[11] Carter JE. Surgical treatment for chronic pelvic pain JLSL 1998-Apr-Jun 2[2]:129-139
[12] Vercelling P. Aimi G, Busacca M, et .al Laparoscopic uterosacral ligament resection for dysmenorrhea associated of a randomized controlled trial. Fertile Steril 2003: 80-310
[13] Laparoscopic uterosacral ligament resection for dysmenorrhea associated with endometriosis: results of a randomized, controlled trial. www. textmed. com Vercellini P, Aimi G, Busacca M, Apolone G, Uglietti A, Crosignani PG.
[14] Acta Obstet Gynecol Scand. 2007 ;86 [1]:4-15 17230282 Surgical interruption of pelvic nerve pathways in dysmenorrhea: a systematic review of effectiveness P M Latthe , M L Proctor , C M Farquhar , N Johnson , K S Khan.
[15] Perry CP, Relationship of gyn. surgery to Constipation 1999;6 [1] ;75-80
[16] Presacral neurectomy can be effective for central pelvic pain, but pain in the Uterine nerve ablation is less effective than presacral neurectomy. japan.medscape.com. ACOG Issues New Guidelines for Chronic Pelvic PainNews Author: Laurie Barclay, MD CME Author: Charles Vega, MD, FAAFP Obstet Gynecol.1997 Dec;90 [ 6 ] :974-7.
[17] The efficacy and complications of laparoscopic presacral neurectomy in pelvic pain FP Chen and YK Soong
[18] Reviewed By: Harvey Simon, MD, Editor-in-Chief, Well-Connected reports; Associate Professor of Medicine, Harvard Medical School; Physician, Massachusetts General Hospital
[19] Kavic MS. Chronic pelvic pain ,hernias and the general surgeon J.Laproendesc Surg 1999;3:89-30
[20] Laparoscopic versus open appendectomy for the treatment of acute appendicitis. RK Mishra, GB Hanna, A Cuschieri [www.World Laparoscopy Hospital.com]
[21] Anders Throrell, Stofelan Grondal et al. Eur J Surg 1999;165:751-754
[22] Cuschieri A Cost efficacy of laparoscopic vs. open surgery . Surg Endosc 1998;12:1197-1198
[23] Advanced Laparoscopic Surgeons, specialists in minimally invasive of endometriomas followed by ovarian repair, and presacral neurectomy Prospective Comparison of Laparoscopic and Conventional Anterior Resection. www.adlap.com/endoExtensive.htm 26k
[24] Fujimoto T, Segawa o, Lane G.J., Esaki S, Miyana T. Surg Endosc 1999; 13:773-777. Interleukin 6 levels were less in a study on newborn infants undergoing laparoscopic procedures when compared to open.
[25] ZulloF,Palomba S,Zupi E, et al. ; Effectiveness of PSN in women with severe dysmenorrhea caused by endometriosis who were treated with LPSN [RCT]Am J Obstet Gynecol 2003 www.textmed.com
[26] Carter JE. Surgical treatment for chronic pelvic pain JLSL 1998-Apr-Jun 2[2]:129-139
[27] Complications of Operative Gynecological Laparoscopy Miranda, Cristi�n S;Carvajal, Antonio R.JSLS, Journal of the Society of Laparoendoscopic Surgeons, Volume 7,Number 1, January - March 2003, pp. 53-58
[28] Cuschieri. A. The dawn of a new century. Surg Endosc [2000] 14: 1-4.
[29] Gambone Jc, Reither RC,Non-surgical Manegement of Chronic Pelvic Pain: a Multi-disciplineary approach Clin Obstet Gynecol 1990;33:205-211
[30] American journal of obstetrics and gynecology [Am. j. obstet. gynecol.] ISSN0002-9378 CODENAJOGAHSource / Source 2003,vol.189,no1,pp.5-10
[31] Spangen L, Andersson R, Non-palpable inguinal hernia in Female Am.Surgeon 1998;9:574-577
[32] Pregnancy rates following ablative laparoscopic surgery for endometriomas K.D. Jones, 1 and C.J.G. Sutton Minimal Access Therapy Training Unit, The Royal Surrey County Hospital, Guildford GU2 7XX, UK.
[33] Textbook of Laparoscopic Surgery by Prof. Dr. R. K. Mishra. M.MAS; MRCS. World Laparoscopy Hospital, Gurugram, NCR Delhi, India.





