Laparoscopic Wells or Marlex Rectopexy
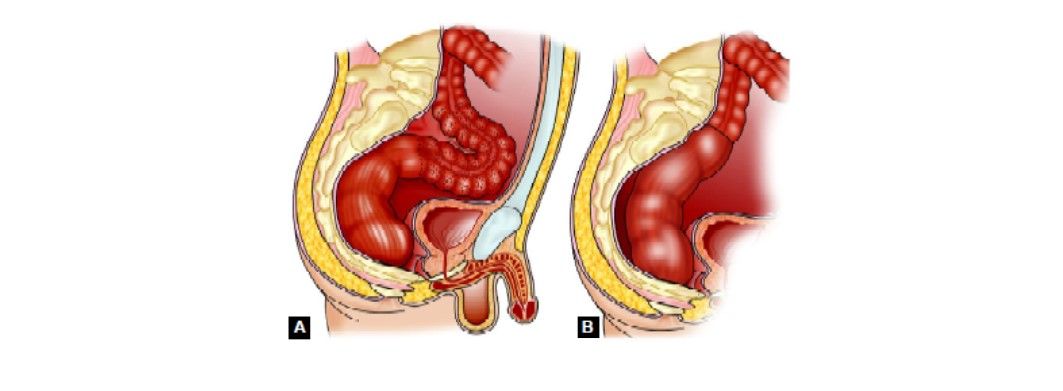
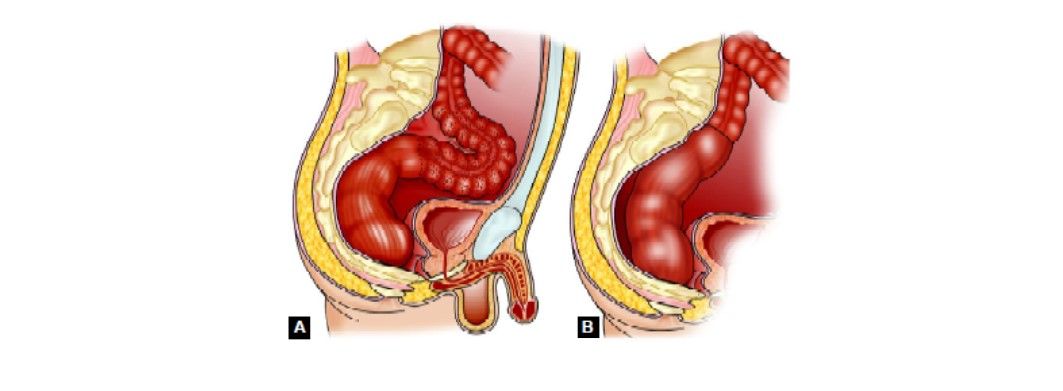
Rectal prolapse is a distressing condition, especially when associated with fecal incontinence and constipation. It usually occurs in children or the elderly. Presently laparoscopic approach is favored as it has better results especially in terms of less postoperative pain, shorter hospital stay, and lower cost. The pelvic sympathetic and parasympathetic nerves run along with the rectum; if dissection is not carried out in the proper plane, injury can occur, leading to bladder dysfunction, impotence, and/or retrograde ejaculation. This is an important consideration when trying to decide which procedure to perform, especially in men, although the risk of injury should be less than 1 to 2 percent. Perineal procedures and anterior resection have a low-risk of outlet obstruction. Abdominal procedures of rectopexy that tack the rectum to the sacrum can cause outlet obstruction if the rectum is wrapped circumferentially, often requiring the release of the fixation to treat the problem.
Laparoscopic Resection rectopexy
In a Marlex rectopexy (Ripstein procedure), the entire rectum is mobilized down to the coccyx posteriorly, the lateral ligaments laterally, and the anterior cul-de-sac anteriorly. A nonabsorbable material, such as Marlex mesh or an Ivalon sponge, is then fixed to the presacral fascia. The rectum is then placed on tension, and the material is partially wrapped around the rectum to keep it in position. The anterior wall of the rectum is not covered with the sponge or mesh in order to prevent a circumferential obstruction. The peritoneal reflections are then closed to cover the foreign body. The Marlex mesh or sponge causes an inflammatory reaction that scars and fixes the rectum into place. The Wells procedure was followed by rectal dysfunction accompanied by increased constipation and evacuation problems. The Ripstein procedure, preserving the lateral ligaments, appears not to affect such symptoms adversely.
Modified mesh rectopexy aligns the rectum, avoids excessive mobilization and division of lateral ligaments thus preventing constipation and preserving potency. We recommend this technique for patients with complete rectal prolapse with up to grade 1, 2, and 3 incontinence based on Browning and Parks classification. During wells rectopexy, the dissection should allow sufficient mobilization of the inferior mesenteric artery so that the origin of the left colic artery is seen. The pedicle is not divided. The plane between the sigmoid colon mesentery and the retroperitoneum is developed laterally, out toward the lateral attachment of the colon. Limited mobilization of the mesentery of the anterior surface of Gerota's fascia and of the left colon should be performed to enhance the fixation of the rectum.
Ripstein's operation often improved anal continence in patients with rectal prolapse and rectal intussusception. This improvement was accompanied by increased Maximum resting pressure in patients with rectal prolapse, indicating recovery of internal anal sphincter function. In one of the studies at the Department of Surgery, Karolinska Institute at Danderyd Hospital, Stockholm, Sweden maximum resting pressure (52+/- 23 mm Hg) was found in Ripstein operation than patients with rectal prolapse. No postoperative increase in MRP was found in patients with rectal intussusception. This suggests an alternate mechanism of improvement in patients with rectal intussusception.
Mobilization of the Lateral Attachments of the Rectosigmoid
For rectal prolapse surgery lateral mobilization the surgeon grasps the rectosigmoid junction with his left-hand instrument and draws it to the patient's right side. This allows the lateral attachments of the sigmoid colon to be seen and divided using cautery. Bruising from the prior retroperitoneal mobilization of the colon can usually be seen in this area. Once this layer of peritoneum has been opened, one immediately enters into the space opened by the retroperitoneal dissection. No dissection should be performed more proximally along the white line of Toldt, toward the splenic flexure.
Rectal Mobilization
An atraumatic bowel clamp inserted through the left lower quadrant port is used to elevate the rectosigmoid colon out of the pelvis and away from the retroperitoneum and sacral promontory, to enable entry into the presacral space. The posterior aspect of the mesorectum can be identified and the mesorectal plane dissected with diathermy, preserving the hypogastric nerves as they pass down into the pelvis anterior to the sacrum. Dissection continues down the presacral space in this avascular plane toward the pelvic floor. Only the posterior 60 percent of the rectum needs be mobilized; however, dissection should be continued all the way to the levator ani muscles. A transanal examining finger should be used to confirm the distal extent of the dissection. The peritoneum on either side of the rectum should be incised to the level of the lateral stalks. The lateral stalks should generally be preserved, the exception being when further dissection must completely reduce a very distal prolapsing segment. The rectum is not divided in the case of wells rectopexy.
Rectopexy
A 2 to 4 cm portion of polypropylene mesh is rolled and inserted through the umbilical trocar. The camera is reinserted and the mesh is positioned at the sacral promontory. A mechanical device used for hernia mesh fixation is used to fix the mesh to the promontory. This may be inserted through the right lower quadrant port, but if adequate access cannot be obtained, a 5 mm suprapubic port may be inserted. Great care must be taken not to tear or strip off the presacral fascia when stapling the mesh in place. The rectum is retracted rostrally to the desired tension to allow complete reduction of the prolapse, which is confirmed by digital rectal examination. The rectopexy is then performed from the right side using the two right-sided trocars. Two or three nonabsorbable sutures are used to attach the distal mesorectum to the mesh at the promontory, sufficient to maintain adequate tension. Alternatively, the mechanical fixation device used for mesh fixation may be employed.
Rectal prolapse is a distressing condition, especially when associated with fecal incontinence and constipation. It usually occurs in children or the elderly. Presently laparoscopic approach is favored as it has better results especially in terms of less postoperative pain, shorter hospital stay, and lower cost. The pelvic sympathetic and parasympathetic nerves run along with the rectum; if dissection is not carried out in the proper plane, injury can occur, leading to bladder dysfunction, impotence, and/or retrograde ejaculation. This is an important consideration when trying to decide which procedure to perform, especially in men, although the risk of injury should be less than 1 to 2 percent. Perineal procedures and anterior resection have a low-risk of outlet obstruction. Abdominal procedures of rectopexy that tack the rectum to the sacrum can cause outlet obstruction if the rectum is wrapped circumferentially, often requiring the release of the fixation to treat the problem.
Laparoscopic Resection rectopexy
In a Marlex rectopexy (Ripstein procedure), the entire rectum is mobilized down to the coccyx posteriorly, the lateral ligaments laterally, and the anterior cul-de-sac anteriorly. A nonabsorbable material, such as Marlex mesh or an Ivalon sponge, is then fixed to the presacral fascia. The rectum is then placed on tension, and the material is partially wrapped around the rectum to keep it in position. The anterior wall of the rectum is not covered with the sponge or mesh in order to prevent a circumferential obstruction. The peritoneal reflections are then closed to cover the foreign body. The Marlex mesh or sponge causes an inflammatory reaction that scars and fixes the rectum into place. The Wells procedure was followed by rectal dysfunction accompanied by increased constipation and evacuation problems. The Ripstein procedure, preserving the lateral ligaments, appears not to affect such symptoms adversely.
Modified mesh rectopexy aligns the rectum, avoids excessive mobilization and division of lateral ligaments thus preventing constipation and preserving potency. We recommend this technique for patients with complete rectal prolapse with up to grade 1, 2, and 3 incontinence based on Browning and Parks classification. During wells rectopexy, the dissection should allow sufficient mobilization of the inferior mesenteric artery so that the origin of the left colic artery is seen. The pedicle is not divided. The plane between the sigmoid colon mesentery and the retroperitoneum is developed laterally, out toward the lateral attachment of the colon. Limited mobilization of the mesentery of the anterior surface of Gerota's fascia and of the left colon should be performed to enhance the fixation of the rectum.
Ripstein's operation often improved anal continence in patients with rectal prolapse and rectal intussusception. This improvement was accompanied by increased Maximum resting pressure in patients with rectal prolapse, indicating recovery of internal anal sphincter function. In one of the studies at the Department of Surgery, Karolinska Institute at Danderyd Hospital, Stockholm, Sweden maximum resting pressure (52+/- 23 mm Hg) was found in Ripstein operation than patients with rectal prolapse. No postoperative increase in MRP was found in patients with rectal intussusception. This suggests an alternate mechanism of improvement in patients with rectal intussusception.
Mobilization of the Lateral Attachments of the Rectosigmoid
For rectal prolapse surgery lateral mobilization the surgeon grasps the rectosigmoid junction with his left-hand instrument and draws it to the patient's right side. This allows the lateral attachments of the sigmoid colon to be seen and divided using cautery. Bruising from the prior retroperitoneal mobilization of the colon can usually be seen in this area. Once this layer of peritoneum has been opened, one immediately enters into the space opened by the retroperitoneal dissection. No dissection should be performed more proximally along the white line of Toldt, toward the splenic flexure.
Rectal Mobilization
An atraumatic bowel clamp inserted through the left lower quadrant port is used to elevate the rectosigmoid colon out of the pelvis and away from the retroperitoneum and sacral promontory, to enable entry into the presacral space. The posterior aspect of the mesorectum can be identified and the mesorectal plane dissected with diathermy, preserving the hypogastric nerves as they pass down into the pelvis anterior to the sacrum. Dissection continues down the presacral space in this avascular plane toward the pelvic floor. Only the posterior 60 percent of the rectum needs be mobilized; however, dissection should be continued all the way to the levator ani muscles. A transanal examining finger should be used to confirm the distal extent of the dissection. The peritoneum on either side of the rectum should be incised to the level of the lateral stalks. The lateral stalks should generally be preserved, the exception being when further dissection must completely reduce a very distal prolapsing segment. The rectum is not divided in the case of wells rectopexy.
Rectopexy
A 2 to 4 cm portion of polypropylene mesh is rolled and inserted through the umbilical trocar. The camera is reinserted and the mesh is positioned at the sacral promontory. A mechanical device used for hernia mesh fixation is used to fix the mesh to the promontory. This may be inserted through the right lower quadrant port, but if adequate access cannot be obtained, a 5 mm suprapubic port may be inserted. Great care must be taken not to tear or strip off the presacral fascia when stapling the mesh in place. The rectum is retracted rostrally to the desired tension to allow complete reduction of the prolapse, which is confirmed by digital rectal examination. The rectopexy is then performed from the right side using the two right-sided trocars. Two or three nonabsorbable sutures are used to attach the distal mesorectum to the mesh at the promontory, sufficient to maintain adequate tension. Alternatively, the mechanical fixation device used for mesh fixation may be employed.


