Laparoscopic Varicocelectomy
Laparoscopic varicocele ligation has been performed by many urologists, and reports from several medical centers have been published. The data suggest that laparoscopic varicocele ligation is therapeutically superior to open surgical and radiographic (embolization) techniques. Laparoscopic varicocelectomy appears to reduce postoperative morbidity. Whether it is necessary to identify and preserve the testicular artery during laparoscopic varicocelectomy remains controversial. Loughlin and Brooks reported on the use of a laparoscopic Doppler probe that they believe, facilitates the identification and preservation of the testicular artery. Matsuda and coworkers claim that the testicular artery does not have to be preserved; they clip the testicular artery and veins en bloc. Further multicenter experience is needed to resolve whether the testicular artery should be preserved during laparoscopic varicocele ligation. Because the testicular artery is preserved during open surgical repair or radiographic embolization procedures we generally preserve the testicular artery during varicocelectomy.
Operative Technique
The technique of laparoscopic varicocele ligation is straightforward. The procedure is usually performed using general anesthesia. A urethral catheter is placed to empty the bladder, and a Veress needle is placed at the umbilicus to inflate the peritoneal cavity with carbon dioxide. Alternatively, Hasson's technique can be performed at the inferior margin of the umbilicus, and the trocar can be placed into the peritoneum under direct vision. Three laparoscopic ports are placed for varicocelectomy according to the baseball diamond concept.
The intra-abdominal vas deferens can be identified as structure joining the spermatic cord above the internal inguinal ring. The gonadal vessels are visualized easily in the retroperitoneum. The posterior peritoneum is excised with cautery, laser, or endoscopic scissors. The gonadal vessels are then mobilized; however, reliably identifying the spermatic artery and its branches are sometimes difficult through the laparoscope. Therefore, many surgeons prefer to use the laparoscopic Doppler probe to facilitate the identification of the spermatic artery during laparoscopic varicocele ligation. The Doppler probe is 28.58 cm long and fits through a 5 mm laparoscopic port. After identifying the gonadal artery, the surgeon isolates the gonadal vein or veins using blunt dissection with atraumatic graspers.
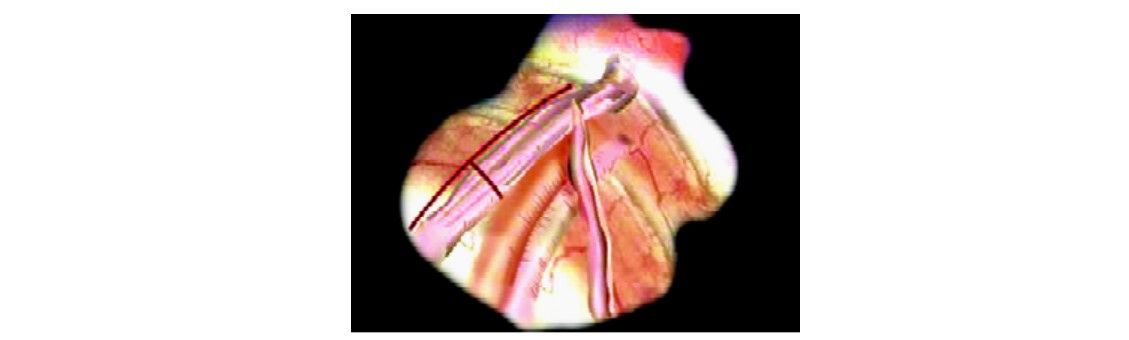
Laparoscopic varicocelectomy

The spermatic vein is identified
Endoscopic clip applier is used to secure it or intracorporeal suturing is used to ligate the gonadal vein or veins while sparing the artery.

Clips applied around a spermatic vein
Laparoscopic Retroperitoneal Node Dissection
The laparoscopic retroperitoneal node dissection in the management of testicular cancer is still not very frequently performed. Increased operating time is a consideration in applying laparoscopic techniques to a procedure. As with pelvic node dissection, the question has also been raised as to the completeness of the laparoscopic retroperitoneal node dissection. Laparoscopic dissection of the nodal tissue behind the aorta and vena cava is difficult laparoscopically.
Laparoscopic retroperitoneal node dissection appears, at least for now, best applied to patients without evidence of bulky disease in the retroperitoneum who would otherwise be candidates for observation rather than surgical exploration. Although the laparoscopic procedure does not currently appear to be as thorough a dissection as the open node dissection, it offers the opportunity to have some pathologic documentation of nodal status in patients considered for observation. The technique for laparoscopic retroperitoneal node dissection has not been standardized and is still evolving; therefore, the reader is referred to the case reports for the author's individual techniques.





