Transabdominal Preperitoneal Repair of Inguinal Hernia
An inguinal hernia results from a hole or defect in the muscles, through which the peritoneum protrudes, forming the sac. Inguinal herniorrhaphy is one of the most common operations that general surgeons perform. Laparoscopic herniorrhaphy is being done at a time when laparoscopic cholecystectomy has shown definite benefits over the open technique. But unlike laparoscopic cholecystectomy, laparoscopic hernia repair is an advanced laparoscopic procedure and has a longer learning curve. In addition, TEP requires higher technical expertise for successful results.
Ger in 1982, attempted minimal access groin hernia repair by closing the opening of an indirect inguinal hernial sac using Michel clips. Bogojavlensky in 1989 modified the technique by intracorporeal suture of the deep ring after plugging a PPM into the sac. Toy and Smoot in 1991, described a technique of intraperitoneal Onlay mesh (IPOM) placement, where an intra-abdominal piece of polypropylene or e-PTFE was stapled over the myopectineal orifice without dissection of the peritoneum.
The present-day techniques of laparoscopic hernia repair evolved from Stoppa’s concept of pre-peritoneal reinforcement of fascia transversalis over the myopectineal orifice with its multiple openings by a prosthetic mesh. In the early 1990’ s Arregui and Doin described the transabdominal preperitoneal (TAPP) repair, where the abdominal cavity is first entered, peritoneum over the posterior wall of the inguinal canal is incised to enter into the avascular preperitoneal plane which is adequately dissected to place a large (15 × 10 cm) mesh over the hernial orifices. After fixation of the mesh, the peritoneum is carefully sutured or stapled. TAPP approach has the advantage of identifying missed additional direct or femoral hernia during the first operation itself. Around the same time Phillips and McKernan described the totally extraperitoneal (TEP) technique of endoscopic hernioplasty where the peritoneal cavity is not breached and the entire dissection is performed bluntly in the extraperitoneal space with a balloon device or the tip of the laparoscope itself. An advanced knowledge of the posterior anatomy of the inguinal region is imperative. Once the dissection is complete, a 15 × 10 cm mesh is stapled in place over the myopectineal orifice. It appears to be the most common endoscopic repair today. In both these repairs, the mesh in direct contact with the fascia of the transversalis muscle in the pre-peritoneal space, allows tissue ingrowths leading to the fixation of the mesh (as opposed to being in contact to the peritoneum as in IPOM repair where it is prone to migrate).
Position of Surgical Team
Surgeon stands towards the opposite side of the hernia near the shoulder. Camera assistant should stand either right to the patient or on the opposite side of the patient.
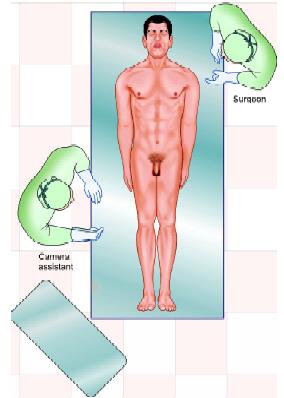
Position of a surgeon in right-sided hernia
Port Position
The position of a port in laparoscopic repair of trans-abdominal hernia repair should be again according to the baseball diamond concept. Please refer to chapter 6.
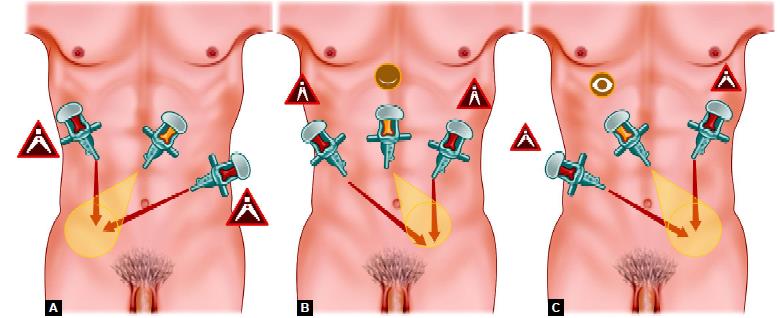
(A) Port position of right-sided hernia; (B) Port position of bilateral hernia; (C) Port position of left-sided hernia
The telescopic port should be in the umbilicus. 30º telescope is a better choice for laparoscopic hernia surgery. A 10 mm umbilical port is used. Two other ports, usually 10 mm for the dominant hand and 5 mm for nondominant hand, are placed lateral to the umbilicus. In a left-sided hernia, the right lateral port should be in the right iliac fossa and left port in the left hypochondrium so that both the instrument should make a manipulation angle of 60°. In right-sided hernia surgery right port should move up towards the hypochondrium and the left port will come down to make the triangle.
Procedure of Tapp
After access, diagnostic laparoscopy is performed to rule out any adhesion or other intra-abdominal lesion. All the important anatomical landmark of hernia surgery is identified with the help of telescope and one atraumatic grasper. The important landmarks of laparoscopic hernia repair are the pubic bone and inferior epigastric vessels. The defect should be seen carefully and if any content is present inside the sac it should be reduced gently. A sliding hernia of the colon should be carefully reduced because chances of perforation of the large bowel are more than other viscera so the assistant should reduce the hernia by pressing it from outside. The assistant should reduce the hernia by pressing the bulge from outside. Any adhesion between the bowel and omentum should be divided carefully using bipolar and scissors.
The next step of transabdominal preperitoneal repair of a hernia is the creation of preperitoneal space. Many surgeons like to do hydrodissection to create this preperitoneal space just by injecting normal saline into preperitoneal space. Some surgeon thinks that it is easy to create preperitoneal space is easy with sharp dissection as well. The peritoneum is cut a minimum of 4 cm lateral to the outer margin of the deep ring at 2 O’clock position if the hernia is the right side and 10 O’clock position for the left side of the hernia. Medial dissection of the peritoneal incision should continue up to medial umbilical ligament. Going medial to a medial umbilical ligament is risky because there is the fear of injury of the urinary bladder. The flap of the peritoneum is separated from above downward as soon as it will reach the site of the internal ring the hernia sac will be encountered.

Incision over peritoneum
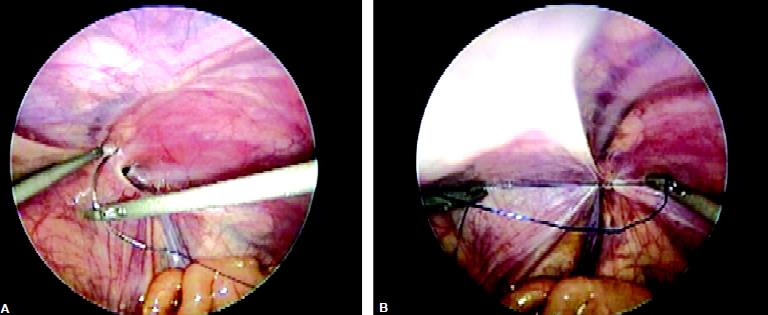
Dissection should be started with opening the peritoneum lateral to the medial umbilical fold in order to identify Cooper’s ligament. Stoppa’s parietalization technique should be used for dissection of the spermatic cord from the peritoneum by separating the elements of the spermatic cord from the peritoneum and peritoneal sac.

Creation of preperitoneal space
In case of an indirect defect, the hernial sac has to be either gently dissected free or inverted, or if it completely adheres with the transversalis fascia and cord structure it can be transacted. Surgeons should use both blunt and sharp dissection and the sac is dissected off the anterior abdominal wall. After being reduced partially it is ligated using an endo- loop and then transected with scissors. In the case of bilateral hernias, the procedure is repeated on the other side. The vas and spermatic vessels have been separated from the sac. The next step is the separation of the sac from cord structures and dissection for the creation of proper lateral space for the placement of mesh. The lateral limit of dissection is the anterosuperior iliac spine while the inferior limit laterally is the psoas muscle. Dissection should be avoided in the “triangle of doom” which is bounded medially by the vas deferens and laterally by the gonadal vessels. A large hernial sac creates multiple planes and it is easy for the beginners to get disoriented with sac vas and vessel. The best way to avoid this confusion is that surgeon should keep himself as close as possible to the outer surface of peritoneum. If the spermatic vessels are injured accidentally it can be clipped. Even if the testicular vessel is injured, the testes will get the blood supply from collateral vessels developed through cremasteric.
Indirect hernias the creation of preperitoneal space is comparatively easy as there is no chance of injury of spermatic vessels and vas. The bulge in the transversalis fascia may be repaired by suturing or stapling. The tacker application and application of electrosurgery should be very careful at the triangle of doom, a triangle of pain, and trapezoid of disaster. In the case of massive complete indirect scrotal hernias, no attempt should be made to reduce the sac completely as it may increase the risk of testicular nerve injury and hematoma formation.
Placement of the Mesh
Criteria for laparoscopic mesh
• Nonabsorbable
• Adequate size
• Adequate memory.
A Proline mesh of appropriate size, usually 15 × 15 cm should be taken and one corner of the mesh should be tailored. Mesh should be rolled and loaded backward in one of the ports. Mesh is placed inside the abdominal cavity through a 12 mm port. If surgery is being performed by a 10 mm port only the port should be removed and rolled mesh should be introduced through the port wound directly. After the introduction of mesh, it is unrolled when it reaches in the peritoneal cavity. The mesh is fixed medially over the Cooper’s ligament and pubic bone using a tacker or anchor. The tailored corner of the mesh should be positioned inferomedially. No lateral slit should be made in the mesh and it should not be fixed laterally to cord structures to prevent injury to the lateral cutaneous nerve of the thigh. The mesh in this position covers the direct, indirect, and femoral defects. It is essential that the mesh should extend below the pubic tubercle so that it covers the femoral orifice. Mesh should also extend medially to cover all the possible orifices of hernia. Laterally mesh should project at least 2 to 3 cm beyond the margin of the deep ring. If the mesh is not of appropriate size, the chance of recurrence is high. Sometime, the surgeon may be disoriented and mesh is placed with its long axis vertical instead of transverse. If the mesh is cut at one of the corner chances of this disorientation is minimum.
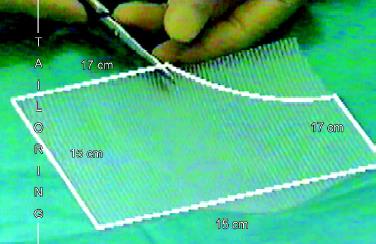
Cutting the corner of the mesh

Introduction of mesh in preperitoneal space
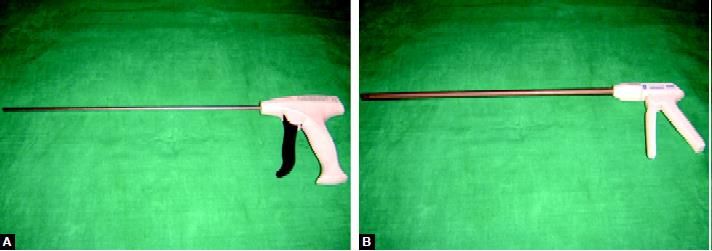
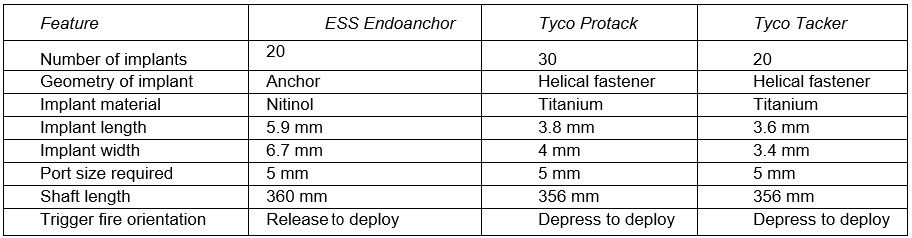
(A) Hernia anchor; (B) Hernia tacker
Implant for Fixing Mesh
Many preloaded devices are available for fixing mesh in hernia surgery. Mesh is fixed medially over the Cooper’s ligament and pubic bone using an implant. Currently, three popular brands of implants to fix the mesh are available. These are Tacker, Protack, or Anchor. The comparative chart of these implants is shown in. After adjusting the mesh properly it should be fixed by stapling first its middle part three-finger above the superior limit of the internal ring. With mesh duly stapled pneumoperitoneum is reduced to 9 mm Hg. It is important to avoid pricking of the inferior epigastric artery or the testicular vessels. Intracorporeal suturing can also be used for fixation of mesh if the surgeon has sufficient suturing skill. After fixing the mesh properly the peritoneum flap is replaced over the mesh and it is closed either by staples or suture. It is important that the mesh should be completely covered by the peritoneum. Ideally, peritoneum should be opposed by overlap fashion and peritoneum defect is closed either by staples or by continuous suturing and Aberdeen termination.

Closure of peritoneum
Repair of Bilateral Inguinal Hernia
In laparoscopic surgery postoperative recovery of bilateral hernia is the same as that of unilateral hernia. The technique of bilateral laparoscopic repair of a hernia is the same as that of unilateral hernia. Patients with bilateral hernia are good candidates for laparoscopy. The two sides may be repaired using two meshes but single long mesh also can be used and is pushed across from one side behind the bladder, and across the inguinal orifice on the opposite side. The size of the mesh for bilateral hernia should be 30 × 15 cm. The surgeon should avoid twisting of mesh. After placing the mesh in bilateral hernia surgery it should look just like a bow tie.

Introduction of mesh for bilateral hernia
Repair of Recurrent Inguinal Hernia
Recurrent laparoscopic hernia after open surgery is better to repair laparoscopically because external anatomy is disrupted and open repair has more chance of recurrence. Laparoscopy is method of choice for recurrent hernia. The defect is usually direct and more than one in a recurrent hernia.
Comparison of ESS Endoanchor, Tyco Protack, Tyco Tacker
The result of laparoscopic repair is excellent even in the case of multiple hernias.
Laparoscopic Hernia in Children
Laparoscopy has been tried in little children. Only closure of ring and herniotomy is possible in the pediatric age group. The sac is simply inverted and tied internally. Care should be taken that the vas or vessels should not be caught in the ligature.
Closure of defect with intracorporeal suturing in pediatric age
Ending of the Operation
At the end of the surgery, the abdomen should be examined for any possible bowel injury or hemorrhage. The entire instrument should be removed and then all the port. Each port should be removed under direct observation through a telescope. Ports larger than 10 mm should be sutured. The telescope should be removed at last after releasing all the gas keeping in mind that the last port should not be pulled without putting telescope or any blunt instrument in, to prevent entrapment of bowel or omentum and formation of adhesion or intestinal adhesion. The wound should be closed with suture, especially a 10 mm wound.





