Laparoscopic Surgery in Pregnancy: Precautions and Complications
Since the advent of laparoscopic surgery in the 1980s, laparoscopic surgery has been popularized by surgeons throughout the world. However, routine laparoscopic surgery has been slow to catch a pregnant patient. Treatment of surgical disease in the gravid patient requires a unique and careful approach where the safety of the mother and fetus are both considered. During pregnancy due to the physiological changes that take place in the mother and considering the presence of a living fetus in utero, surgical conditions are handled with a lot of care and cautions. In past, pregnancy was considered to be absolutely contraindicated for laparoscopic intervention, but with a better understanding of the physiology of pregnancy and improved anesthetic and laparoscopic techniques, emergency laparoscopic procedures such as diagnostic laparoscopy for pain abdomen, appendicectomy, splenectomy, pheochromocytoma, cholecystectomy, are feasible in pregnancy. Lachman et al. have already reported 300 laparoscopic procedures during pregnancy.
The responsibility of caring for two patients during one operation and the concern over potential harm to the unborn fetus due to the pneumoperitoneum and/or instrumentation are factors that have played a role in the delay of adapting laparoscopic surgery to the pregnant patient. However, recent evidence suggests that not only is laparoscopic surgery safe in the pregnant patient in all three trimesters, but it is also often preferable. During pregnancy usually, all surgical procedures are avoided to minimize various risks of anesthesia and procedure to mother and fetus. At times emergency surgical conditions make it absolutely necessary for an intervention. With increasing progress in minimal access surgery more and more surgeons have found the skill and interest to perform the emergency procedures laparoscopically. Laparoscopy was first done in pregnancy for diagnosis and evaluation. The first laparoscopic appendicectomy in pregnancy was performed by Scheiber in 1990. The first laparoscopic cholecystectomy in laparoscopy was first done in pregnancy for diagnosis and evaluation of acute abdominal pain in 1980.
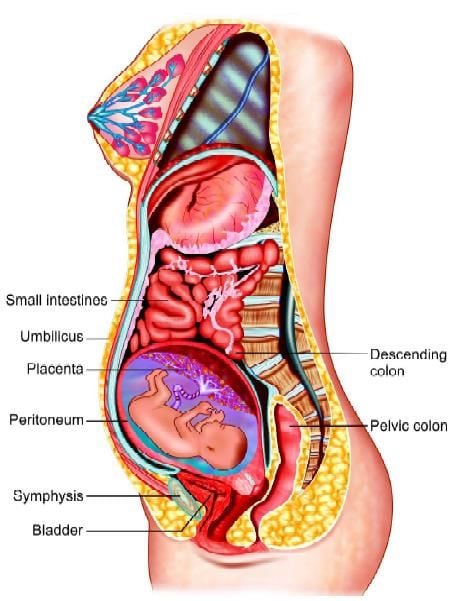
Anatomical changes inside the abdominal cavity during pregnancy
However, surgical intervention in pregnant ladies needs special consideration of the well-being of both mother and fetus, if intrauterine viable fetus is present, and in cases of ectopic pregnancy or heterotrophic pregnancy, the pathophysiological changes brought about during pregnancy should be considered for the safety of the patient. Furthermore, with the advancement of pregnancy laparoscopic diagnosis and procedures become more challengingly difficult as the gravid uterus displaces the organs and becomes completely an abdominal organ. Up to date, the data on laparoscopic procedures during pregnancy are still limited, but with the growing ability of minimal access surgeons the recent accumulating data show that laparoscopic procedures such as diagnostic laparoscopy, adnexal surgery, appendicectomy, splenectomy, cholecystectomy, and management of ectopic and heterotrophic pregnancies are relatively safe and effective during pregnancy, if certain precautions are taken. But of course like all surgical procedures in pregnancy there is an increased risk of certain complications with laparoscopic intervention in pregnancy.
Physiological changes in Pregnancy
Almost all organ systems undergo physiological changes in pregnancy. These changes should be considered during operative procedures in pregnancy.
Gastrointestinal System
Due to enlarged gravid uterus, the stomach is pushed towards diaphragm and assumes a more horizontal position. The viscera like transverse, ascending, and descending colon is displaced, so the location of abdominal pain and tenderness especially in conditions like appendicitis is altered. The hormonally induced decrease lower esophageal sphincter tone causes gastroesophageal regurgitation which places the pregnant lady at a higher risk of aspiration, so nasogastric tube suction and careful airway management is necessary for all pregnant patients undergoing laparoscopy.
Cardiovascular and Hematological Changes
Cardiac output and blood volume increase by 30 to 40 percent, but as RBC volume does not expand by the same ratio this result in physiological anemia especially noticed in the second trimester. After 20 weeks of gestation, the gravid uterus compresses the aorta and inferior vena cava and may cause supine hypotension syndrome, so during surgery, the patient should be positioned in a lateral recumbent position to avoid vena caval compression. A vasomotor block caused by spinal anesthesia produces more severe hypotension than in nonpregnant individuals. During pregnancy WBC count increases to 12,000 to 14,900 per mm. A hypercoagulable state is physiologically developed in pregnancy due to an increase in fibrinogen and other coagulation factors such as factor VII, factor VIII, factor IX, and factor X. Thus, the risk of thromboembolism increases in pregnancy.
Respiratory System
Due to enlarging gravid uterus gradually, the chest movements are restricted. There is an increase in minute ventilation and oxygen consumption and a decrease in residual volume, also mixed venous oxygen content and functional reserve capacity also decrease so the patient is prone to hypoxemia and hypocapnia. PaCO2 of 28 to 32 mm, pH of 7.44, and decrease bicarbonate levels are detected due to chronic respiratory alkalosis which has to be maintained during pregnancy. The patient gains more weight during pregnancy and there is more edema in soft tissues of the neck, so the anesthetist may face more difficulties in airway management.
Urinary System
Hydroureter decreased urethral peristalsis and bladder expansion increases the incidence of urinary tract infection. There is increased retention of water and electrolytes.
Other Changes
In addition to the respiratory changes, there are mild hematologic abnormalities in the pregnant patient. Levels of fibrinogen, factor VII, and factor XII are increased, whereas there are decreased levels of antithrombin III, all of which result in an increased risk of venous thromboembolism. When considering the acute abdomen in a pregnant patient, making the correct diagnosis may often be difficult. Nausea and vomiting, leukocytosis, low-grade fever, mild hypotension, and anorexia are common. The gravid uterus pushes the abdominal contents cephalad, displacing organs and inhibiting the migration of the omentum, causing altered landmarks and often distorting the clinical picture. During the second and third trimesters, the gravid uterus may cause decreased gastric motility and may lead to an increased risk of gastroesophageal reflux disease (GERD) and aspiration as well.
Fetal Consideration
A fetus is a hidden patient in the womb of the pregnant mother and its health should be considered by surgeon and anesthetist both. It is important to:
• Maintain uteroplacental blood flow and oxygenation. Decreased uteroplacental blood flow may be due to maternal hypotension or an increase in uterine artery resistance.
• Maternal hypoxia causes fetal hypoxia and metabolic acidosis and in the long-term, it may be fatal to infants, so it should be prevented.
• Avoid teratogenic drugs during anesthesia. Cocaine is known to have a teratogenic effect so products containing cocaine should be avoided. Diazepam and nitrous oxide are considered safe during anesthesia as no teratogenicity was detected clinically.
• Avoid preterm labor. Try to manipulate the uterus minimum as possible. Although there is an increased incidence of spontaneous abortion, premature delivery, and low birth weight following anesthesia in emergency situations operation are unavoidable.
Effects of Pneumoperitoneum in Pregnancy During Laparoscopic Procedure
In a pregnant patient, the pneumoperitoneum increases the intra-abdominal pressure and this causes decreased inferior vena caval return to the heart, hence decreased cardiac output. With reverse Trendelenburg position decreased cardiac output is even worsened, cardiac index decreases, and when this is combined with mothers hypoxia can cause fetal death. Increased intra-abdominal pressure also leads to decreased uterine blood flow and increase intrauterine pressure, these may, in turn, cause fetal hypoxia and may lead to fetal death. Pneumoperitoneum decreases the diaphragmatic movement, in pregnant lady already the movement of the diaphragm is decreased due to bulky uterus, this further decrease in movement due to pneumoperitoneum causes increased peak airway pressure, decrease functional reserve capacity, increased ventilation-perfusion mismatch, decreased thoracic cavity compliance and increase pleural pressure.
The use of CO2 for causing pneumoperitoneum leads to hypercarbia and further hypoxemia. The CO2 absorbs across the peritoneum and leads to respiratory acidosis in patient and her fetus. If pCO2 increases above 40 mm, decreased removal of CO2 occurs leading to fetal acidosis. Fetal tachycardia and hypotension may develop as a result of fetal hypocarbia. This can be corrected by maintaining mild maternal respiratory alkalosis, by hyperventilating the mother during surgery. Monitoring maternal arterial blood gases is better than monitoring PaCO2 during laparoscopic procedures.
N2O as the gas for pneumoperitonization will not cause fetal respiratory acidosis, but it is highly combustible.
Criteria for Patient Selection
A safe laparoscopic procedure can be performed in all three trimesters of pregnancy from 2 to 31 weeks. During the first trimester, there is an increased risk of abortion up to 12 percent also a risk of teratogenesis increases in the first trimester. In the third trimester, there is a 40 percent risk of preterm labor and a 30 percent risk of premature birth. Also, the visualization in the laparoscopic procedure is decreased due to enlarged uterus.
Therefore, the second trimester is considered the safest time for laparoscopic surgery in pregnancy. The risk of abortion is not increased, with no risk of teratogenesis, and the risk of preterm labor is only five percent in the second trimester.
Advantages of Laparoscopic in Pregnancy
• Short hospital stay
• Early return to normal activities
• Small incision, so rapid postoperative recovery and fewer incision complications such as hernia, postoperative wound infection, and pain.
• Less uterine manipulation and hence decrease uterine irritability and fetal loss.
Risk of Laparoscopy in Pregnancy
• More chance of uterine injury during port entry as the uterus becomes an abdominal organ after the first trimester.
• Problems associated with pneumoperitonization as discussed already.
• CO2 absorption causes increase CO2 pressure and decrease arterial pH.
• Risk of exposure to intra-abdominal smoke including carbon monoxide generated by electrosurgery and laser.
Strategies for Safe Laparoscopic Surgery in Pregnancy
• Surgery should be done in the second trimester.
• If the patient presents in the late third trimester, surgery should be postponed if possible until after delivery.
• Nasogastric incubation is a must in all cases as there is a high risk of aspiration into the lungs.
• Patient can be placed in a dorsal lithotomy position in the first half of pregnancy, but in the second- half to prevent inferior vena cava compression patient is ideally placed in a lateral recumbent position.
• Hypotension should be avoided; proper fluid replacement should be done.
• Ideal method for commencing pneumoperitoneum is open Hasson trocar method. The placement of trocar depends on the size of the gravid uterus.
• Tocolysis is indicated if signs of uterine irritability are present.
• Decrease operation time by using an adequate number of ports, and using the most experienced surgeons.
• Maternal hyperventilation to maintain end-tidal CO2
the pressure at 32 mm Hg.
• Lower CO2 insufflation pressure of < 12 mm Hg should be used to avoid fetal acidosis.
• Electrocautery should be used with care; the smokes containing carbon monoxide should be evacuated promptly to avoid toxic effects to the fetus.
• Entry of all instruments must be under direct vision; care should be taken to avoid injury to the gravid uterus.
• All specimens should be removed with endobag to avoid spillage.
• Manipulators should never be fixed to the vagina or cervix.
Society of American Gastrointestinal Endoscopic Surgery (SAGES) Recommendations
• Obstetrical consultation should be obtained preoperatively.
• When possible, operative intervention should be deferred until the second trimester, when fetal risk is lowest.
• Pneumoperitoneum enhances lower extremity venous stasis already present in the gravid patient and pregnancy induces a hypercoagulable state. Therefore, pneumatic compression devices should be utilized whenever possible.
• Fetal and uterine status, as maternal end-tidal CO2 and/ or arterial blood gases, should be monitored.
• The uterus should be protected with a lead shield if intraoperative cholangiography is a possibility.
• Fluoroscopy should be utilized selectively.
• Given the enlarged gravid uterus, abdominal access should be attained using an open technique.
• Dependent positioning should be utilized to shift the uterus away from the inferior vena cava.
• Pneumoperitoneum pressures should be kept at 10 mm Hg.
• Further studies into methods that increase the safety of laparoscopy in a pregnant patient should be done.
Discussion
Advances in laparoscopic surgery have led to development of methods to perform abdominal surgery and reduce morbidity using minimal access surgery techniques. In 1999, Lachman et al. reported on a series of pregnant women undergoing 518 surgical procedures. Cholecystectomy (45%) is the most common procedure performed during pregnancy followed by adnexal surgery (34%) and appendicectomy (15%). Operative procedures are postponed in the pregnant patient until after delivery, but in acute emergency conditions even if the patient is pregnant, the operation should be performed. According to the recent studies done the second trimester is ideal for laparoscopic intervention. Most cases reported and small series indicate that laparoscopy can be safely performed during pregnancy. The incidence of prematurity and intrauterine growth restriction was reported to be higher in the open surgical group too.
Two recent studies suggest that there is no difference in fetal outcome for patients with singleton pregnancies undergoing laparoscopy or laparotomy. In one study the resultant children born after laparoscopic surgery were performed on their mother during their intrauterine life, were monitored and no evidence of developmental or physical abnormality was detected during the study period. Despite the growing clinical experience suggesting that laparoscopy is as safe as laparotomy in pregnancy, more long-term clinical studies are required.
Conclusion
Laparoscopic access to pathology in pregnancy has many benefits for the patient, but it is important that the surgeon and anesthetist both have immense knowledge of maternal-fetal physiology. An experienced surgeon can continue to perform laparoscopy safely in all trimesters by without significant increases in either maternal or fetal morbidity or mortality. Further controlled clinical studies are needed to clarify many other unknown issues, and revision may be necessary as new data appear.
Since the advent of laparoscopic surgery in the 1980s, laparoscopic surgery has been popularized by surgeons throughout the world. However, routine laparoscopic surgery has been slow to catch a pregnant patient. Treatment of surgical disease in the gravid patient requires a unique and careful approach where the safety of the mother and fetus are both considered. During pregnancy due to the physiological changes that take place in the mother and considering the presence of a living fetus in utero, surgical conditions are handled with a lot of care and cautions. In past, pregnancy was considered to be absolutely contraindicated for laparoscopic intervention, but with a better understanding of the physiology of pregnancy and improved anesthetic and laparoscopic techniques, emergency laparoscopic procedures such as diagnostic laparoscopy for pain abdomen, appendicectomy, splenectomy, pheochromocytoma, cholecystectomy, are feasible in pregnancy. Lachman et al. have already reported 300 laparoscopic procedures during pregnancy.
The responsibility of caring for two patients during one operation and the concern over potential harm to the unborn fetus due to the pneumoperitoneum and/or instrumentation are factors that have played a role in the delay of adapting laparoscopic surgery to the pregnant patient. However, recent evidence suggests that not only is laparoscopic surgery safe in the pregnant patient in all three trimesters, but it is also often preferable. During pregnancy usually, all surgical procedures are avoided to minimize various risks of anesthesia and procedure to mother and fetus. At times emergency surgical conditions make it absolutely necessary for an intervention. With increasing progress in minimal access surgery more and more surgeons have found the skill and interest to perform the emergency procedures laparoscopically. Laparoscopy was first done in pregnancy for diagnosis and evaluation. The first laparoscopic appendicectomy in pregnancy was performed by Scheiber in 1990. The first laparoscopic cholecystectomy in laparoscopy was first done in pregnancy for diagnosis and evaluation of acute abdominal pain in 1980.
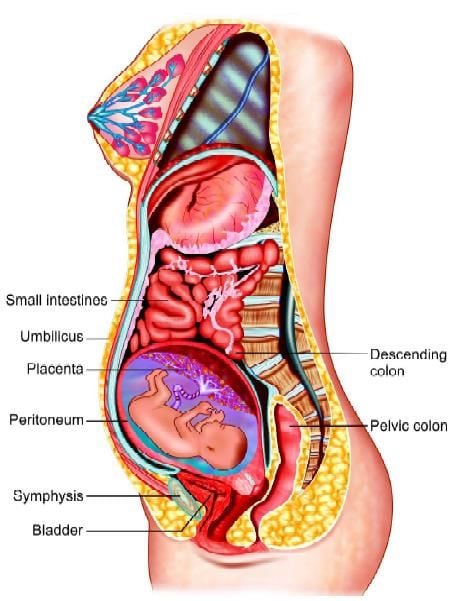
Anatomical changes inside the abdominal cavity during pregnancy
However, surgical intervention in pregnant ladies needs special consideration of the well-being of both mother and fetus, if intrauterine viable fetus is present, and in cases of ectopic pregnancy or heterotrophic pregnancy, the pathophysiological changes brought about during pregnancy should be considered for the safety of the patient. Furthermore, with the advancement of pregnancy laparoscopic diagnosis and procedures become more challengingly difficult as the gravid uterus displaces the organs and becomes completely an abdominal organ. Up to date, the data on laparoscopic procedures during pregnancy are still limited, but with the growing ability of minimal access surgeons the recent accumulating data show that laparoscopic procedures such as diagnostic laparoscopy, adnexal surgery, appendicectomy, splenectomy, cholecystectomy, and management of ectopic and heterotrophic pregnancies are relatively safe and effective during pregnancy, if certain precautions are taken. But of course like all surgical procedures in pregnancy there is an increased risk of certain complications with laparoscopic intervention in pregnancy.
Physiological changes in Pregnancy
Almost all organ systems undergo physiological changes in pregnancy. These changes should be considered during operative procedures in pregnancy.
Gastrointestinal System
Due to enlarged gravid uterus, the stomach is pushed towards diaphragm and assumes a more horizontal position. The viscera like transverse, ascending, and descending colon is displaced, so the location of abdominal pain and tenderness especially in conditions like appendicitis is altered. The hormonally induced decrease lower esophageal sphincter tone causes gastroesophageal regurgitation which places the pregnant lady at a higher risk of aspiration, so nasogastric tube suction and careful airway management is necessary for all pregnant patients undergoing laparoscopy.
Cardiovascular and Hematological Changes
Cardiac output and blood volume increase by 30 to 40 percent, but as RBC volume does not expand by the same ratio this result in physiological anemia especially noticed in the second trimester. After 20 weeks of gestation, the gravid uterus compresses the aorta and inferior vena cava and may cause supine hypotension syndrome, so during surgery, the patient should be positioned in a lateral recumbent position to avoid vena caval compression. A vasomotor block caused by spinal anesthesia produces more severe hypotension than in nonpregnant individuals. During pregnancy WBC count increases to 12,000 to 14,900 per mm. A hypercoagulable state is physiologically developed in pregnancy due to an increase in fibrinogen and other coagulation factors such as factor VII, factor VIII, factor IX, and factor X. Thus, the risk of thromboembolism increases in pregnancy.
Respiratory System
Due to enlarging gravid uterus gradually, the chest movements are restricted. There is an increase in minute ventilation and oxygen consumption and a decrease in residual volume, also mixed venous oxygen content and functional reserve capacity also decrease so the patient is prone to hypoxemia and hypocapnia. PaCO2 of 28 to 32 mm, pH of 7.44, and decrease bicarbonate levels are detected due to chronic respiratory alkalosis which has to be maintained during pregnancy. The patient gains more weight during pregnancy and there is more edema in soft tissues of the neck, so the anesthetist may face more difficulties in airway management.
Urinary System
Hydroureter decreased urethral peristalsis and bladder expansion increases the incidence of urinary tract infection. There is increased retention of water and electrolytes.
Other Changes
In addition to the respiratory changes, there are mild hematologic abnormalities in the pregnant patient. Levels of fibrinogen, factor VII, and factor XII are increased, whereas there are decreased levels of antithrombin III, all of which result in an increased risk of venous thromboembolism. When considering the acute abdomen in a pregnant patient, making the correct diagnosis may often be difficult. Nausea and vomiting, leukocytosis, low-grade fever, mild hypotension, and anorexia are common. The gravid uterus pushes the abdominal contents cephalad, displacing organs and inhibiting the migration of the omentum, causing altered landmarks and often distorting the clinical picture. During the second and third trimesters, the gravid uterus may cause decreased gastric motility and may lead to an increased risk of gastroesophageal reflux disease (GERD) and aspiration as well.
Fetal Consideration
A fetus is a hidden patient in the womb of the pregnant mother and its health should be considered by surgeon and anesthetist both. It is important to:
• Maintain uteroplacental blood flow and oxygenation. Decreased uteroplacental blood flow may be due to maternal hypotension or an increase in uterine artery resistance.
• Maternal hypoxia causes fetal hypoxia and metabolic acidosis and in the long-term, it may be fatal to infants, so it should be prevented.
• Avoid teratogenic drugs during anesthesia. Cocaine is known to have a teratogenic effect so products containing cocaine should be avoided. Diazepam and nitrous oxide are considered safe during anesthesia as no teratogenicity was detected clinically.
• Avoid preterm labor. Try to manipulate the uterus minimum as possible. Although there is an increased incidence of spontaneous abortion, premature delivery, and low birth weight following anesthesia in emergency situations operation are unavoidable.
Effects of Pneumoperitoneum in Pregnancy During Laparoscopic Procedure
In a pregnant patient, the pneumoperitoneum increases the intra-abdominal pressure and this causes decreased inferior vena caval return to the heart, hence decreased cardiac output. With reverse Trendelenburg position decreased cardiac output is even worsened, cardiac index decreases, and when this is combined with mothers hypoxia can cause fetal death. Increased intra-abdominal pressure also leads to decreased uterine blood flow and increase intrauterine pressure, these may, in turn, cause fetal hypoxia and may lead to fetal death. Pneumoperitoneum decreases the diaphragmatic movement, in pregnant lady already the movement of the diaphragm is decreased due to bulky uterus, this further decrease in movement due to pneumoperitoneum causes increased peak airway pressure, decrease functional reserve capacity, increased ventilation-perfusion mismatch, decreased thoracic cavity compliance and increase pleural pressure.
The use of CO2 for causing pneumoperitoneum leads to hypercarbia and further hypoxemia. The CO2 absorbs across the peritoneum and leads to respiratory acidosis in patient and her fetus. If pCO2 increases above 40 mm, decreased removal of CO2 occurs leading to fetal acidosis. Fetal tachycardia and hypotension may develop as a result of fetal hypocarbia. This can be corrected by maintaining mild maternal respiratory alkalosis, by hyperventilating the mother during surgery. Monitoring maternal arterial blood gases is better than monitoring PaCO2 during laparoscopic procedures.
N2O as the gas for pneumoperitonization will not cause fetal respiratory acidosis, but it is highly combustible.
Criteria for Patient Selection
A safe laparoscopic procedure can be performed in all three trimesters of pregnancy from 2 to 31 weeks. During the first trimester, there is an increased risk of abortion up to 12 percent also a risk of teratogenesis increases in the first trimester. In the third trimester, there is a 40 percent risk of preterm labor and a 30 percent risk of premature birth. Also, the visualization in the laparoscopic procedure is decreased due to enlarged uterus.
Therefore, the second trimester is considered the safest time for laparoscopic surgery in pregnancy. The risk of abortion is not increased, with no risk of teratogenesis, and the risk of preterm labor is only five percent in the second trimester.
Advantages of Laparoscopic in Pregnancy
• Short hospital stay
• Early return to normal activities
• Small incision, so rapid postoperative recovery and fewer incision complications such as hernia, postoperative wound infection, and pain.
• Less uterine manipulation and hence decrease uterine irritability and fetal loss.
Risk of Laparoscopy in Pregnancy
• More chance of uterine injury during port entry as the uterus becomes an abdominal organ after the first trimester.
• Problems associated with pneumoperitonization as discussed already.
• CO2 absorption causes increase CO2 pressure and decrease arterial pH.
• Risk of exposure to intra-abdominal smoke including carbon monoxide generated by electrosurgery and laser.
Strategies for Safe Laparoscopic Surgery in Pregnancy
• Surgery should be done in the second trimester.
• If the patient presents in the late third trimester, surgery should be postponed if possible until after delivery.
• Nasogastric incubation is a must in all cases as there is a high risk of aspiration into the lungs.
• Patient can be placed in a dorsal lithotomy position in the first half of pregnancy, but in the second- half to prevent inferior vena cava compression patient is ideally placed in a lateral recumbent position.
• Hypotension should be avoided; proper fluid replacement should be done.
• Ideal method for commencing pneumoperitoneum is open Hasson trocar method. The placement of trocar depends on the size of the gravid uterus.
• Tocolysis is indicated if signs of uterine irritability are present.
• Decrease operation time by using an adequate number of ports, and using the most experienced surgeons.
• Maternal hyperventilation to maintain end-tidal CO2
the pressure at 32 mm Hg.
• Lower CO2 insufflation pressure of < 12 mm Hg should be used to avoid fetal acidosis.
• Electrocautery should be used with care; the smokes containing carbon monoxide should be evacuated promptly to avoid toxic effects to the fetus.
• Entry of all instruments must be under direct vision; care should be taken to avoid injury to the gravid uterus.
• All specimens should be removed with endobag to avoid spillage.
• Manipulators should never be fixed to the vagina or cervix.
Society of American Gastrointestinal Endoscopic Surgery (SAGES) Recommendations
• Obstetrical consultation should be obtained preoperatively.
• When possible, operative intervention should be deferred until the second trimester, when fetal risk is lowest.
• Pneumoperitoneum enhances lower extremity venous stasis already present in the gravid patient and pregnancy induces a hypercoagulable state. Therefore, pneumatic compression devices should be utilized whenever possible.
• Fetal and uterine status, as maternal end-tidal CO2 and/ or arterial blood gases, should be monitored.
• The uterus should be protected with a lead shield if intraoperative cholangiography is a possibility.
• Fluoroscopy should be utilized selectively.
• Given the enlarged gravid uterus, abdominal access should be attained using an open technique.
• Dependent positioning should be utilized to shift the uterus away from the inferior vena cava.
• Pneumoperitoneum pressures should be kept at 10 mm Hg.
• Further studies into methods that increase the safety of laparoscopy in a pregnant patient should be done.
Discussion
Advances in laparoscopic surgery have led to development of methods to perform abdominal surgery and reduce morbidity using minimal access surgery techniques. In 1999, Lachman et al. reported on a series of pregnant women undergoing 518 surgical procedures. Cholecystectomy (45%) is the most common procedure performed during pregnancy followed by adnexal surgery (34%) and appendicectomy (15%). Operative procedures are postponed in the pregnant patient until after delivery, but in acute emergency conditions even if the patient is pregnant, the operation should be performed. According to the recent studies done the second trimester is ideal for laparoscopic intervention. Most cases reported and small series indicate that laparoscopy can be safely performed during pregnancy. The incidence of prematurity and intrauterine growth restriction was reported to be higher in the open surgical group too.
Two recent studies suggest that there is no difference in fetal outcome for patients with singleton pregnancies undergoing laparoscopy or laparotomy. In one study the resultant children born after laparoscopic surgery were performed on their mother during their intrauterine life, were monitored and no evidence of developmental or physical abnormality was detected during the study period. Despite the growing clinical experience suggesting that laparoscopy is as safe as laparotomy in pregnancy, more long-term clinical studies are required.
Conclusion
Laparoscopic access to pathology in pregnancy has many benefits for the patient, but it is important that the surgeon and anesthetist both have immense knowledge of maternal-fetal physiology. An experienced surgeon can continue to perform laparoscopy safely in all trimesters by without significant increases in either maternal or fetal morbidity or mortality. Further controlled clinical studies are needed to clarify many other unknown issues, and revision may be necessary as new data appear.





