Introduction
Laparoscopic splenectomy over the last decade has been accepted as the gold standard for indications like Idiopathic Thrombocytopenic Purpura and has been prolonged to larger and complicated spleens faced by surgeons in a variety of hematological and non-hematological disorders. ITP may be the most common indication for laparoscopic splenectomy. Hereditary spherocytosis, thrombotic thrombocytopenic purpura and others hematological problems adhere to. Hodgkin’s and non-Hodgkin’s lymphomas,and chronic lymphocytic leukemia, usually are reported frequently in literature, performed to manage the complications of hypersplenism, debulk illness, and enhance response to chemotherapy or for symptomatic splenomegaly. Patients with non-Hodgkin’s lymphoma almost never need setting up. Patients along with Hodgkin’s condition who've diffuse illness may all obtain chemotherapy. Likewise, sufferers with limited illness are usually treated with radiotherapy. A few patients with stage II disease will need surgical staging, that ought to be performed laparoscopically and you will be a sign for splenectomy. Literature evaluation reveals that laparoscopic splenectomy can be done in patients when splenectomy is indicated. Contraindications are proportional to surgeon’s experience and expertise. Complete contraindications towards the laparoscopic strategy include severe cardiopulmonary disease and other co-morbid conditions making laparoscopic as well as open splenectomy impossible to do. Relative contraindications may include big spleens, trauma, website hypertension, aneurysms of splenic pedicle, pregnancy, previous abdominal surgical treatment as well as couple of other people. Massive spleens greater than 4000 gm have been tackled laparoscopically, though Terrosu et al8 report higher incidence of conversion, bleeding and morbidity in spleens greater than 2000 gm. Experienced surgeons have reported an effective laparoscopic splenectomy for trauma. Hashizume et al have reported 42 successful splenectomies in the event of cirrhosis with portal hypertension. LS in pregnancy and aneurysms happen to be reported. Upper abdominal surgery that were a relative contraindication continues to be circumvented through the open technique. Significant obesity isn't a contraindication. On the other hand, the actual post-surgical consequences of open up surgery in obese patients often merit the additional laparoscopic effort in these patients. Tha harsh truth that the surgeon needs to understand here's “one ought to know the limitations and transform as soon as possible.”
Though all indications given in standard textbooks of surgery happen to be conquered by laparoscopy, the reported frequent indications are:
- Isolated indications
- Hereditary Spherocytosis
- Hodgkins and Non-Hodgkins lymphoma
- ITP
Use of high end energy sourse is essential for splenectomy and Harmonic Shears is probably the best advance in the practice of laparoscopic and even open surgery. The blades from the working instrument oscillate at 55,000 cycles per second generating local heat in between blades. This induces coagulation of proteins and works well for cutting of tissues and vessels being dissected. Lateral thermal spread is restricted to less than 2 mm, allowing the use of the instrument in difficult areas like the space between the gastric fundus and also the spleen. One should be cautious however in using this device to seal vessels over 4 mm. Another precaution to become kept in mind that the vessels sealed with this instrument shouldn't be handled because they often open and bleed. The harmonic shears offers certainly decreased operative time and has lessened blood loss during surgery.
The use of staplers in open surgery continues to be popular. The same has now been extended to laparoscopy. Intestinal in addition to vascular endoscopic staplers can be found and can supply in number of indications. During laparoscopic splenectomy, the pedicle might be transected en bloc, with a single application of a 3-cm vascular linear laparoscopic stapler. Complications such as bleeding occur, but they are mostly because of inappropriate technique. Massively enlarged spleens are heavy and hard to manipulate by thin and nimble laparoscopic instruments. Handport is an adjustable unit that fits the incision and prevents gas leaks during manipulation, and at rest. Incision is usually necessary for delivery because these are difficult to devote bags. Morcellation can also be contraindicated. Alternatively, whenever a counter-incision for intact elimination of an bigger spleen is predicted, keeping the incision could be planned to facilitate surgery with the “hand-assisted” technique. Having the hands inside of the abdomen provides the all important touch perception, helps retraction and dissection, charge of bleed in necessity and retrieval from the specimen and it is a suggested procedure of choice in splenomegaly. Pfannenstiel incision is less painful than conventional subcostal incision and is the most well-liked incision in hand assisted laparoscopic splenectomy. Ligasure also imparts precise amount of bipolar energy and pressure to tissue achieving permanent seal. These devices can and it has been used not only to seal smaller vessels but also the primary splenic pedicle with success. Tagaya N et al have reported three successful laparoscopic splenectomies utilizing a 2 mm telescope. They used three 2 mm ports for telescope and instruments and something 12 mm port for retrieval. Use of robotics, though in the infancy in surgical applications are also successfully applied in laparoscopic splenectomy by Chapman et al. Preoperative embolization from the splenic artery was advocated in large spleens to diminish blood loss during surgery and operative time.This method has its own complications and has been abandoned by most authors.
Preoperative Preparation
In elective situations, all patients should receive polyvalent pneumococcal and Haemophilus influenza type B vaccinations 2 -3 weeks before surgery. Blood and blood goods are essential in taking care of unexpected complications.
Coperative technique
Position and approach all the placements - supine, lateral and angled have been described. The first literature describes supine position for laparoscopic splenectomy. Lateral and angled positions are preferred today. Surgeons who use endostaplers for pedicle transection appear to prefer lateral position. The angled or the partial right lateral position is amenable to urgent conversion to laparotomy if severe hemorrhage occurs and is our preferred position.
Two approaches are described:
- Anterolateral approach
- Posterior or Posterolateral approach
Within the anterolateral approach, effect of position and gravity after the dissection from the gastrocolic ligament retracts the viscera and exposes the pancreatic tail and also the splenic pedicle. There's immediate access towards the splenic artery and vein. The splenic artery could be ligated at the start of the procedure. Early ligation is supposed to slow up the size and decrease loss of blood during surgery. The splenophrenic ligament may be the last to become tackled. Despite the 6% incidence of benign pancreatic reaction and a slightly higher risk of pancreatic injury (9.5%), we're feeling how the procedure does not handle the spleen around in posterior approach and in event of transformation, it's easier to tackle the spleen within the same position. Accessory spleens will also be easy to consider when searching for this method. Hence, this is the preferred approach in literature.
The posterior technique was described by Gagner et al. In this approach, the spleen is retracted medially after dividing the splenophrenic and splenorenal ligaments. The pancreatic tail is visualized and so may be the splenic pedicle. The approach is reported to possess a lesser incidence of pancreatic complications and bleeding.This method requires experience with retroperitoneal laparoscopic dissection technique unfamiliar to an average laparoscopic surgeon since many are been trained in open splenectomy by transabdominal technique.
The Procedure - Anterolateral approach
Co2 insufflation is done utilizing a Veress needle at umbilicus or open technique at preplanned port site and maintained at 12 mm Hg to 14 mm Hg.
The port placement
The success story to any laparoscopic procedure is based on precise port placement. Though books mention ports related to fixed anatomical landmarks, we're feeling how the port placement be planned after examining the inflated abdomen and the splenic size. The Indian abdomen differs from those of patient from West. The primary objective of port placements should be to tackle the splenic pedthe actualicle easily. The writer normally advocates 4 ports.
- For the telescope - This port is probably the most important. It usually lies along the line joining the umbilicus and the costal margin in the midclavicular line.
- Two working ports would lie on either side of the telescope.
- The fourth port lies in the left anterior or midaxillary line to retract the spleen and use suction at the appropriate interval. Care ought to be come to place this port so the port is away from the spleen along with the working port.
- A fifth port might be required in cases of enlarged spleen or hanging left lobe of liver in the xiphisternum.
Laparoscopic splenectomy is performed in following stages:
- Division of the gastrocolic ligament such as the short gastric vessels,
- Retraction of splenic flexure of the colon by dividing the splenocolic ligament
- Control of the splenic pedicle
- Hilar dissection
- Division of the splenorenal ligament and attachment to the diaphragm
- Division of gastrocolic ligament including the short gastric vessels: The stomach is retracted right and the gastrocolic ligament opened. The ligament is divided using monopolar or bipolar electrocautery, clips or harmonic shears. We discover that careful use of monopolar coagulation is usually sufficient even for short gastric vessels within an average Indian patient. When lateral thermal spread is really a worry specially in the region of the fundus from the stomach and upper pole of the spleen , or short gastric vessels are of larger caliber than expected, bipolar or clips prove useful. Harmonic shears scores total these modalities. On opening the gastrocolic and gastrosplenic ligament, the splenic pedicle behind the pancreatic tail is inspected. The spleen can also be evaluated for notching from the anterior border, which correlates with a distributed hilar vasculature and it is predictive from the level of difficulty. Inspection is also performed for accessory spleens at this time. It's advantageous to keep some amount of gastrosplenic ligament on the side of splenic hilum so that the same might be handled to retract the spleen laterally at the appropriate interval.
- Retraction of splenic flexure from the colon by dividing the splenocolic ligament: The splenocolic ligament is next dissected bringing down the splenic flexure from the colon. The position of the patient and effect of gravity now keeps away the colon in the operative field.
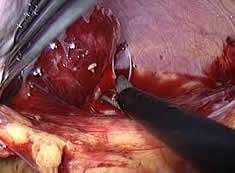
- Securing the Splenic pedicle: Michels described the importance of distributed and magesterial pattern of arterial supply towards the spleen.Within the distributed pattern, multiple branches arise in the main trunks before entering the spleen, whilst in the magesterial pattern the artery enters the hilum as a bundle using the vein. The artery is easily located along the superior border of the pancreas due to its pulsations. Incision on the visceral peritoneum over this artery helps make the dissection easy. The arterial interruption is possible using suture knotting, clips, and endostaplers or even using the newer modalities like Ligasure. The writer uses intracorporeal knotting as primary modality with clips to make sure secure ligation. There's two described methods for tackling the splenic artery. The first is to ligate the splenic artery early in the procedure while others go ahead and take branches of the artery as the dissection proceeds along the hilum from the spleen. Early ligation from the vessel should really decrease how big spleen and cause lesser hemorrhage. Interruption of artery soon changes the colour from the spleen from brown to blue and it is a useful indicator of progress from the procedure. If colour of any part from the spleen remains unchanged, it should indicate another arterial supply to that part and meticulously looked for during further dissection. We now have found this method satisfying in our experience. The splenic vein is tackled as part of hilar dissection. In patients where magistral pattern is encountered, endoscopic vascular staplers are utilized to tackle the completely dissected pedicle en-block in Western countries.
- 4. Hilar dissection: The hilar dissection starts in the lower pole of the spleen and proceeds superiorly staying close to the medial surface. This decreases the chances of injury to the pancreas. In enlarged spleens, the tail from the pancreas can come dangerously near to the hilum making matters worse. Lower polar vessels in many cases are constant and require clips or harmonic shear. The splenic vein is generally a conglomerate of two tributaries. There's a very thin fascia covering the anterior aspect of the vein that needs careful dissection. Entering the correct plane between this fascia and the vein is the key to successful dissection. This is particularly true as the vein is really a thin walled structure that can be easily injured. The splenic vein is interrupted in a similar manner as described for that artery. Since the dissection proceeds superiorly, many find a separate pedicle supplying top of the pole as well as supply in the pancreatic bed. These also require clipping or shearing using harmonic scalpel.
- Division from the splenorenal ligament and attachment towards the diaphragm: Once the hilar dissection is complete, the spleen is detached from the diaphragmatic and renal ligamentous attachments using electrocautery or harmonic shears.
- Retrieval of the spleen: The spleen is delivered by use of commercially accessible puncture resistant bags. The baggage are delivered out through among the ports and the spleen morcellated before removal. Care ought to be taken that we now have no punctures within the bag and spillage into the peritoneal cavity. Enlargedspleens are hard to place in the bags and may require incision for removal. Pathologists sometimes require the entire specimen for reporting. We have been like a routine, employing Pfannenstiel incision of extraction of the spleen due to larger spleens encountered. Drain is positioned after confirming hemostasis within the splenic fossa and ports are closed.
Complications
The complications of laparoscopic splenectomy like a procedure are the same as those of open splenectomy which range from intraoperative bleeding, postsplenectomy sepsis, wound/port site infection and pancreatic injury. The majority of the complications are technique related.27 Higher pancreatic complications23 like pancreatic injury has been a few discussion, with a higher incidence when compared with open procedure.





