Laparoscopic Splenectomy
Laparoscopic splenectomy first started in the early nineties, but due to the lack of an acceptable conversion rate, it was not accepted by most of the laparoscopic surgeons. Now due to increased proficiency in the performance of laparoscopic procedures, the conversion rate is now inexistent even with large spleens. To date, this procedure continues to be associated with a steep learning curve but remains a very rewarding elegant procedure. The indications for this procedure have broadened and are now the same as with open procedures. They range from idiopathic thrombocytopenic purpura, unresponsive hemolytic anemia to staging procedures, and to primary splenic cysts.
The only contraindication of laparoscopic splenectomy is excessively large spleens with weight over 1000 gm. We personally believe that the maneuvers used to remove such large spleens do not warrant these procedures. One should always remember that by laparoscopic approach, the spleen cannot be removed in its integral anatomical form and is usually shredded. If there is any need to preserve splenic integrity, then the laparoscopic approach should not be indicated.
Operating Room Set-up and Patient Position
The patient is placed in a supine and semi right lateral position on the table. The surgeon stands to the right of patient. The camera operator stands right side of the patient next to the surgeon towards the right-hand side of the surgeon. The monitor is placed left to the patient and Mayo’s stand is placed near the feet of the patient.

Position of the surgical team

Various steps of splenectomy
Port Position
The port position should be decided according to the baseball diamond concept depending on the size of the spleen.
Operative Procedure
Laparoscopic splenectomy can be described in 5 steps:
Step 1: Dissection of the inferior aspect of the spleen.

Dissection of the inferior aspect of the spleen
Step 2: Dissection of the lateral and retroperitoneal attachments.
Step 3: Transaction of the splenic hilum.
A 10 mm fan retractor is inserted and will lift the inferior aspect spleen superiorly. The tail of the pancreas should be identified. The splenorenal and colosplenic ligaments are divided with sharp dissection. The dissection is continued superior and lateral to mobilize the entire spleen. It is essential to continue our dissection posterior and inferior to the spleen as far as possible. Its purpose is to sufficiently expose the posterior aspect of the splenic hilum. The entire anterior aspect of the hilum should also be well-visualized. Occasionally, the short gastric vessels will have to be first transacted to gain additional exposure. The stapler is inserted and each jaw should be positioned anterior and posterior to the splenic vessels. Although this procedure appears very audacious to the neophyte, complete hemostasis of the splenic hilum is usually achieved. The instrument is fired several times in sequence.
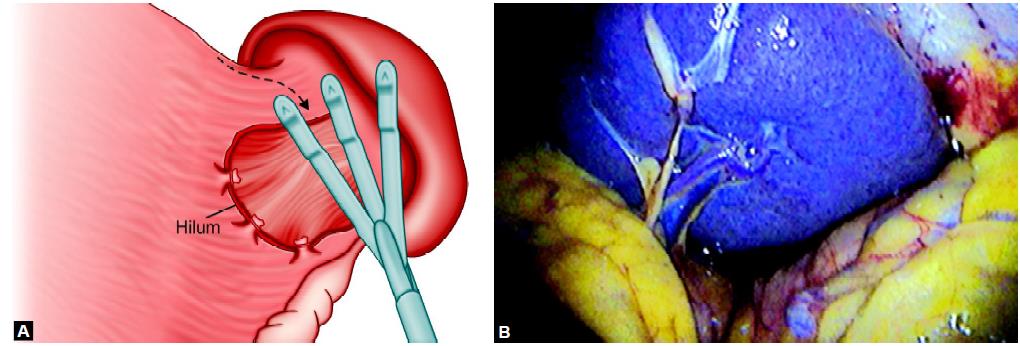
Retractor is necessary to expose the hilum of the spleen

Dissection of the splenic hilum

Use of endo GI linear stapler or vascular stapler can make the laparoscopic splenectomy easy but many surgeons use extracorporeal knots as their main skill to secure splenic umenti
Step 4: Dissection of the short gastric vessels.
The short gastric vessels are best divided using energy like either ligasure harmonic or simple bilateral. The clip or stapler may be used also for short gastric vessels. Each time the spleen is moved superiorly, inferiorly or medially and all the attachments should be carefully dissected. With the slow and careful separation of ligaments, the spleen should be entirely detached.
Step 5: Removing the spleen.
The most lateral 12 mm trocar is removed; its site is enlarged and replaced by a 15 mm trocar. An endobag is introduced and deployed in the intraabdominal cavity. The spleen is placed in the specimen retrieval bag. The specimen retrieval bag is closed and brought against the anterior abdominal wall. It is open via the enlarged trocar site. The spleen is then sectioned in smaller pieces in the specimen retrieval bag and removed with a large clamp. A drain is left in the intra-abdominal cavity. The final evaluation of the abdominal cavity is done and the instruments are removed. The Port is closed according to need.

Manual morcellation of the spleen inside endobag.
Laparoscopic splenectomy first started in the early nineties, but due to the lack of an acceptable conversion rate, it was not accepted by most of the laparoscopic surgeons. Now due to increased proficiency in the performance of laparoscopic procedures, the conversion rate is now inexistent even with large spleens. To date, this procedure continues to be associated with a steep learning curve but remains a very rewarding elegant procedure. The indications for this procedure have broadened and are now the same as with open procedures. They range from idiopathic thrombocytopenic purpura, unresponsive hemolytic anemia to staging procedures, and to primary splenic cysts.
The only contraindication of laparoscopic splenectomy is excessively large spleens with weight over 1000 gm. We personally believe that the maneuvers used to remove such large spleens do not warrant these procedures. One should always remember that by laparoscopic approach, the spleen cannot be removed in its integral anatomical form and is usually shredded. If there is any need to preserve splenic integrity, then the laparoscopic approach should not be indicated.
Operating Room Set-up and Patient Position
The patient is placed in a supine and semi right lateral position on the table. The surgeon stands to the right of patient. The camera operator stands right side of the patient next to the surgeon towards the right-hand side of the surgeon. The monitor is placed left to the patient and Mayo’s stand is placed near the feet of the patient.

Position of the surgical team

Various steps of splenectomy
Port Position
The port position should be decided according to the baseball diamond concept depending on the size of the spleen.
Operative Procedure
Laparoscopic splenectomy can be described in 5 steps:
Step 1: Dissection of the inferior aspect of the spleen.

Dissection of the inferior aspect of the spleen
Step 2: Dissection of the lateral and retroperitoneal attachments.
Step 3: Transaction of the splenic hilum.
A 10 mm fan retractor is inserted and will lift the inferior aspect spleen superiorly. The tail of the pancreas should be identified. The splenorenal and colosplenic ligaments are divided with sharp dissection. The dissection is continued superior and lateral to mobilize the entire spleen. It is essential to continue our dissection posterior and inferior to the spleen as far as possible. Its purpose is to sufficiently expose the posterior aspect of the splenic hilum. The entire anterior aspect of the hilum should also be well-visualized. Occasionally, the short gastric vessels will have to be first transacted to gain additional exposure. The stapler is inserted and each jaw should be positioned anterior and posterior to the splenic vessels. Although this procedure appears very audacious to the neophyte, complete hemostasis of the splenic hilum is usually achieved. The instrument is fired several times in sequence.
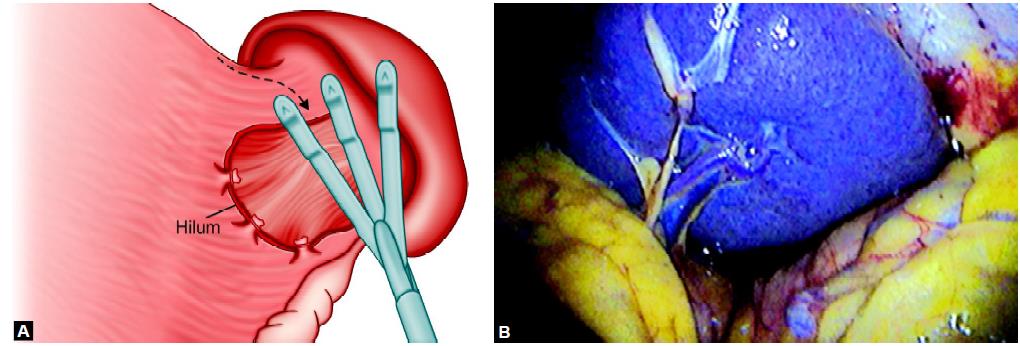
Retractor is necessary to expose the hilum of the spleen

Dissection of the splenic hilum

Use of endo GI linear stapler or vascular stapler can make the laparoscopic splenectomy easy but many surgeons use extracorporeal knots as their main skill to secure splenic umenti
Step 4: Dissection of the short gastric vessels.
The short gastric vessels are best divided using energy like either ligasure harmonic or simple bilateral. The clip or stapler may be used also for short gastric vessels. Each time the spleen is moved superiorly, inferiorly or medially and all the attachments should be carefully dissected. With the slow and careful separation of ligaments, the spleen should be entirely detached.
Step 5: Removing the spleen.
The most lateral 12 mm trocar is removed; its site is enlarged and replaced by a 15 mm trocar. An endobag is introduced and deployed in the intraabdominal cavity. The spleen is placed in the specimen retrieval bag. The specimen retrieval bag is closed and brought against the anterior abdominal wall. It is open via the enlarged trocar site. The spleen is then sectioned in smaller pieces in the specimen retrieval bag and removed with a large clamp. A drain is left in the intra-abdominal cavity. The final evaluation of the abdominal cavity is done and the instruments are removed. The Port is closed according to need.

Manual morcellation of the spleen inside endobag.


