Laparoscopic Right Colectomy
A right colectomy or ileocolic resection is the removal of all or part of the right colon and part of the ileum. These operations are performed for the removal of cancers, certain non-cancerous growths as well as severe Crohn's disease. If performed by an expert laparoscopic surgeon, laparoscopic right colectomy and ileocolic resection are as safe as "open" surgery in carefully selected cases.
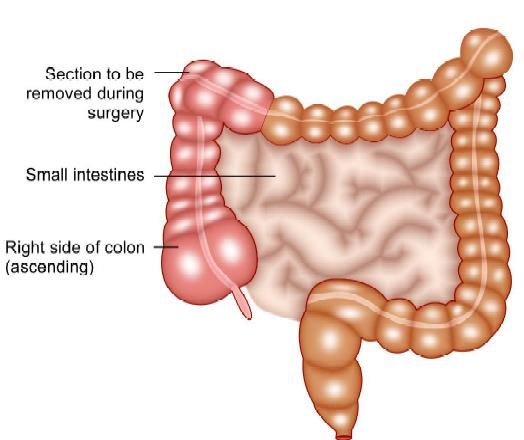
Section to be removed in right colectomy
Indications
The advanced laparoscopic skills required for laparoscopic resection of the colon and rectum have precluded wide dissemination of this procedure. By applying certain key principles, laparoscopic right hemicolectomy can be made simple, reproducible, easy to teach, easy to learn, and cost-effective. Although benign tumors not resectable by a colonoscopic procedure and stricturing inflammatory bowel disease may be good indications for laparoscopy, they are not so common. The most common disease for right colectomy is right-sided colon cancer. Colon cancer seems to be a good indication for laparoscopic surgery if performed using proper oncologic methods, i.e. early proximal ligation of the major mesenteric vessels and wide mesenteric and intestinal resection with complete lymphadenectomy. For right colectomy, laparoscopic mobilization of the bowel, mesenteric resection, or both is performed as for open colectomy, and bowel division and creation of the anastomosis are performed extracorporeally.
Contraindications
• Patients with complete obstruction caused by the cancer
• Cancer extensively invading adjacent organs
• Bulky cancer larger than 10 cm in size should be excluded.
According to these concepts, a proper oncologic approach using laparoscopy for right colon cancer is described in this chapter.
Equipment and Instruments
One can use the same basic equipment, such as light source, insufflator, 30 degrees angled laparoscope, and 5-mm graspers. To this basic equipment can be added reusable instruments such as Babcock and alligator clamps, which should be at least 38 to 40 cm in length to reach from the depths of the pelvis to the upper abdomen using limited port sites. In developing country these reusables can be used to keep disposable equipment to a minimum. Three 10 mm or 12 mm trocars with stability threads, plus reducers for 5 mm instruments should be used. Cannulas should allow instruments to move through smoothly while maintaining a good seal after multiple instrument passages. An energy source device of one's choice can also be added either bipolar, ligasure, or harmonic scalpel can be used. Additional disposable equipment is kept readily available in the operating room and opened only as needed. These include a clip applier, linear vascular stapler, suction irrigator, and fan retractor.
Patient Positioning and Operating Room Setup
The patient is placed supine, and straps are used to secure the patient during steep table position changes. The patient is fixed in a moldable "bean bag" form with both arms tucked in, and placed in a modified lithotomy position using levitator stirrups. A urinary catheter is placed in the bladder, and the stomach is decompressed with a nasogastric tube. Identical operating room personnel is used for the laparoscopic case as for an open right hemicolectomy. The nurse is on the patient's right. This is also where the assistant starts, with the surgeon on the patient's left side facing the right colon. Hasson (open) technique is preferred to safely insert the first port through the umbilicus. After establishing pneumoperitoneum, the surgeon stands on the patient's left side to expose the right mesocolon and to mark the lower border of the ileocolic vessels.
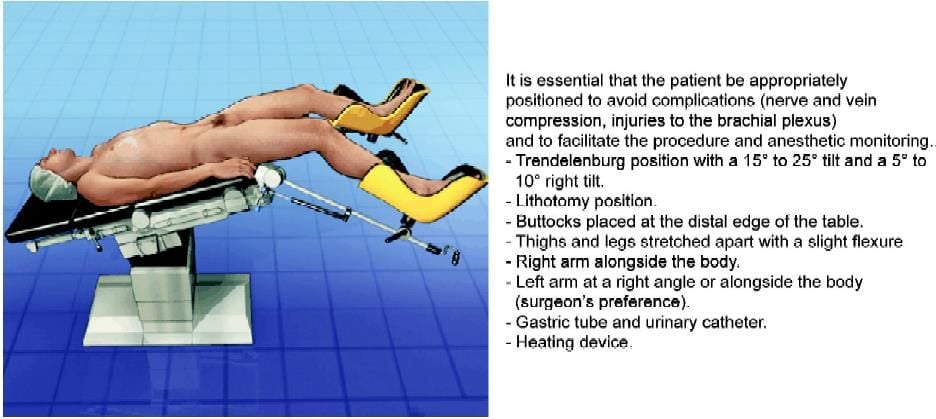
Position of the patient for colorectal surgery
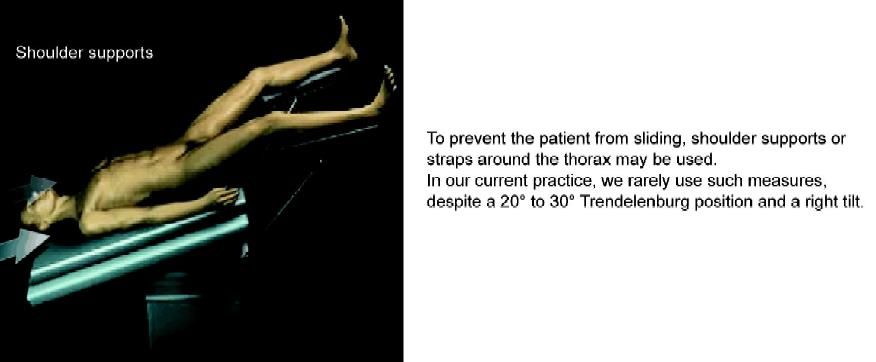
Shoulder support to prevent sliding during colorectal surgery
After initial exploration ensures no prohibitive adhesions, two additional 10 to 12 mm ports are placed under direct visualization, one in the left upper quadrant (in or lateral to the rectus, avoiding the epigastric vessels, approximately a handbreadth from the supraumbilical port) and one in the suprapubic midline. Once all the trocars are in place, the assistant moves to the patient's left side to direct the camera. To start the initial dissection the surgeon moves between the patient's legs, the assistants position themselves on the patient's left side and the nurse stands near the patient's right knee. The main monitor is placed near the patient's right shoulder to give the surgeon and the assistant's optimal viewing. The second monitor is placed on the left side close to the head, a location that gives the best view for the nurse. After completing the proximal vessel ligation with lymphadenectomy and mobilization of the terminal ileum and the cecum, the surgeon moves back to the patient's left side and the first assistant stands between the patient's legs for take-down of right flexure and whole mobilization of the right colon.
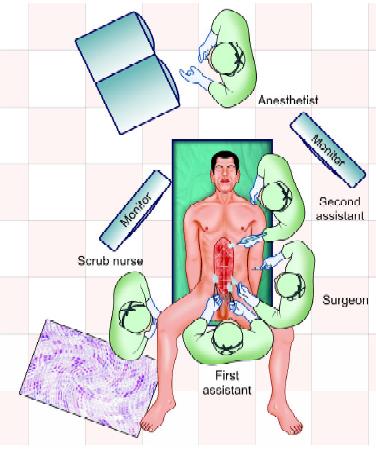
Position of the surgical team during colorectal surgery
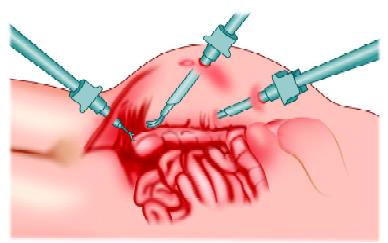
Mobilization of the cecum and right colon
Operative Technique
Right colectomy can be broadly divided into the following steps:
• Ligation of ileocolic vessels
• Identification of right ureter
• Dissection along the superior mesenteric vein
• Division of omentum
• Division of the right branch of middle colic vessels
• Transection of the transverse colon
• Mobilization of the right colon
• Transection of the terminal ileum
• Ileocolic anastomosis
• Delivery of specimen
The patient is positioned in Trendelenburg with the right side inclined upward. This allows the small bowel and omentum to fall toward the left upper quadrant, exposing the cecum and assisting in retraction. The omentum and transverse colon are moved toward the upper abdomen, the ventral side of the right mesocolon is well visualized, and the optimal operative field can be achieved. The small bowel is mobilized out of the pelvis by grasping the peritoneum, not bowel wall, near the base of the cecum, and pulling cephalad and to the left. The appropriate plane along the base of the small bowel mesentery and around the cecum can be seen and the peritoneum overlying it carefully opened, exposing the correct retroperitoneal plane. The ureter is identified either before opening the peritoneum in a thin patient or after, being visualized as it courses over the right iliac vessels. Dissection is then continued around the base of the cecum. Moving cephalad and laterally, the white line of Toldt is incised as the right colon is retracted medially and cephalad by grasping the cut edge of the peritoneum, not the bowel.
Before starting the dissection, the ileocolic pedicle must be definitively identified by retracting the right mesocolon. Various approaches, such as lateral-to-medial (lateral approach), medial-to-lateral (medial approach), and retroperitoneal approach can be tried. The medial approach is quite effective for complete lymphadenectomy with early proximal ligation, minimal manipulation of the tumor-bearing segment, and ideal entry to proper retroperitoneal plane.
Various approaches to the right colon mobilization have been described.
A: Lateral to medial ("classic" open approach);
B: Medial to lateral approach);
C: Retroperitoneal approach.
It is believed that the medial approach is optimal in order to maintain conventional oncologic principles. First, the mesocolon near the ileocecal junction is lifted to confirm the ileocolic pedicle. The root of the ileocolic pedicle is usually located at the lower border of the duodenum. The independent right colic vessels, if present, are located at the upper border at the duodenum. However, the majority of patients do not have the independent right colic vessels (vessels originating directly from the superior mesenteric artery and vein. The surgeon should initially stand on the patient's left side to confidently know the ileocolic pedicle from the superior mesenteric vessels, and to mark the lower border of the ileocolic pedicle.
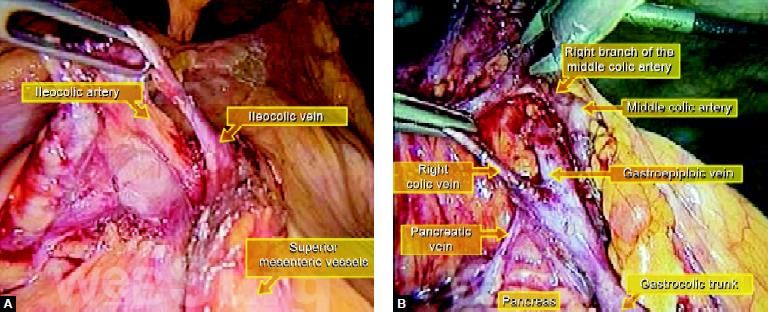
(A) Position of major blood vessels at the time of surgery; (B) Important vessels supplying right side of the colon
Once the ileocolic pedicle is identified, the surgeon moves between the patient's legs, and the scope is inserted through the suprapubic port. The medial side of the right mesocolon is first incised starting from the previously marked region below the ileocolic pedicle, followed by the incision of the peritoneum over to the superior mesenteric vessels. This is done before mobilization of the right colon. With adequate traction of mesocolon toward the right upper quadrant, the ileocolic vessels are easily mobilized from the subperitoneal fascia leading onto the duodenum. Their origins are identified from the superior mesenteric vessels at the lower border of the duodenum and divided.
The surgeon's first step in the dissection is to mark the inferior border of the ileocolic pedicle. From between the legs, the surgeon dissects the peritoneum overlying the ileocolic vascular pedicle over to the superior mesenteric vessels. After mobilization of the ileocolic pedicle from the duodenum, the dissection of the ventral side of the superior mesenteric vein leads to the dissection of the origin of the ileocolic artery. In type B, the ileocolic artery is running behind the superior mesenteric vein. After mobilization and division of the ileocolic pedicle from the duodenum, the dissection of the ventral side of the superior mesenteric vein leads to a complete dissection of the root of the middle colic artery and vein. Careful dissection onto the duodenum and the caudad portion of the pancreas must be exercised in the exposure of the middle colic vessels. Dissection around Henle's trunk (the truck of mesenteric veins consisting of the gastroepiploic vein fusing with the right branch of the middle colic vein or the main middle colic vein) may lead to the exposure of an accessory right colic vein. Accessory right colic vein and right branches of middle colic vessels are clipped and divided. However, if an accessory right colic vein is difficult to confirm in this situation, this vein may be easily detected later at the take-down of the right flexure.
After securing the vessels, the operating table is tilted into the steep Trendelenburg position with the right side down to move the small intestine toward the right upper quadrant. After confirming the right ureter and gonadal vessels through the subperitoneal fascia at the right pelvic brim, the peritoneum is incised along the base of the ileal mesentery upward to the duodenum, and the ileocecal region is mobilized medial to lateral. After this mobilization, the surgeon moves back to the patient's left side and the scope is inserted through the umbilical port. The right mesocolon is mobilized from medial to lateral. Again, this approach allows dissection into the proper retroperitoneal plane. The right gonadal vessels and ureter are safe from injury in this plane, so exposing them is not necessary. This approach also allows the surgeon to work in a straight path from medial to lateral, without tissue to obstruct the vision that can occur working from lateral to medial. This plane connects the previous dissection plane from the caudad side.
The anatomy around the right flexure is very important to avoid inadvertent bleeding especially from around Henle's (gastrocolic) trunk. However, if the previous mesenteric dissection is fully performed from the caudad side and the accessory right colic vein is divided, the right flexure is easily taken down only by dividing the hepatocolic ligament. If the accessory right colic vein is difficult to detect at the previous dissection, it can be easily confirmed from Henle's trunk at this situation and should be divided before extracting the right colon to avoid its injury. Up to this point, the primary tumor has been minimally manipulated using medial to lateral approach. Finally, the right flexure and right colon including the tumor-bearing segment are detached laterally, which completes the mobilization of the entire right colon.

Specimen of the right side of the colon after right colectomy
Once the entire right colon is freed, it is withdrawn through an enlargement of the port site at the umbilicus. The wound must be covered with a wound protector to prevent contamination or metastasis. The resection of ileum and transverse colon, and the anastomosis are accomplished extracorporeally by the functional end to end anastomotic method using conventional staplers or by a hand-sewn method. The anastomotic site is returned to the peritoneal cavity. Wounds and peritoneal cavity are copiously irrigated. All wounds are closed and operation is completed.

Transaction of ileum by the stapler
The identification of a small tumor in the colon may be difficult even in conventional open surgery. In laparoscopic surgery, where there is no tactile sensation, pre- or intraoperative marking of the tumor is frequently needed. Various kinds of marking methods,
e.g. dye injection and mucosal clip placement by preoperative colonoscopy, have been reported for the tumor localization. Several reports demonstrated the usefulness of tattooing the colonic wall adjacent to the tumor with India ink in four quadrants using preoperative colonoscopy.
However, effective injection in all four points of the bowel is sometimes difficult to achieve. In some cases, the surgeon failed to achieve serosal staining visible at laparoscopy, which forced them to use intraoperative colonoscopy. This complicated the laparoscopic colon resection because of the distended bowel related to air insufflation during colonoscopy.
Conclusion
Right-sided colon cancer can be adequately treated by proper laparoscopic procedures adherent to the oncologic principles. Port-site metastasis after laparoscopic colon cancer surgery is unlikely to be a major risk factor when the procedure is performed according to oncologic principles (Refer to Chapter 6). It is believed that laparoscopic right colectomy for cancer performed by expert surgeons is accepted as less invasive surgery without sacrificing the survival benefit compared with conventional open right colectomy.
A right colectomy or ileocolic resection is the removal of all or part of the right colon and part of the ileum. These operations are performed for the removal of cancers, certain non-cancerous growths as well as severe Crohn's disease. If performed by an expert laparoscopic surgeon, laparoscopic right colectomy and ileocolic resection are as safe as "open" surgery in carefully selected cases.
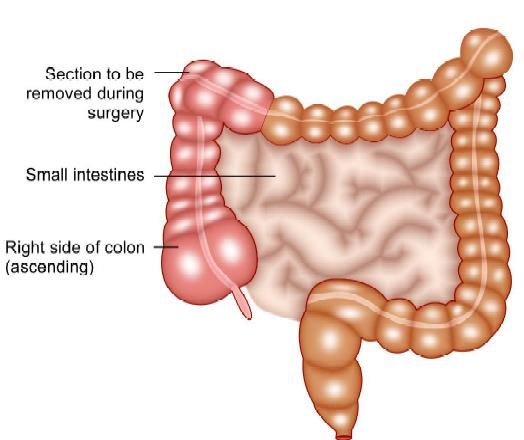
Section to be removed in right colectomy
Indications
The advanced laparoscopic skills required for laparoscopic resection of the colon and rectum have precluded wide dissemination of this procedure. By applying certain key principles, laparoscopic right hemicolectomy can be made simple, reproducible, easy to teach, easy to learn, and cost-effective. Although benign tumors not resectable by a colonoscopic procedure and stricturing inflammatory bowel disease may be good indications for laparoscopy, they are not so common. The most common disease for right colectomy is right-sided colon cancer. Colon cancer seems to be a good indication for laparoscopic surgery if performed using proper oncologic methods, i.e. early proximal ligation of the major mesenteric vessels and wide mesenteric and intestinal resection with complete lymphadenectomy. For right colectomy, laparoscopic mobilization of the bowel, mesenteric resection, or both is performed as for open colectomy, and bowel division and creation of the anastomosis are performed extracorporeally.
Contraindications
• Patients with complete obstruction caused by the cancer
• Cancer extensively invading adjacent organs
• Bulky cancer larger than 10 cm in size should be excluded.
According to these concepts, a proper oncologic approach using laparoscopy for right colon cancer is described in this chapter.
Equipment and Instruments
One can use the same basic equipment, such as light source, insufflator, 30 degrees angled laparoscope, and 5-mm graspers. To this basic equipment can be added reusable instruments such as Babcock and alligator clamps, which should be at least 38 to 40 cm in length to reach from the depths of the pelvis to the upper abdomen using limited port sites. In developing country these reusables can be used to keep disposable equipment to a minimum. Three 10 mm or 12 mm trocars with stability threads, plus reducers for 5 mm instruments should be used. Cannulas should allow instruments to move through smoothly while maintaining a good seal after multiple instrument passages. An energy source device of one's choice can also be added either bipolar, ligasure, or harmonic scalpel can be used. Additional disposable equipment is kept readily available in the operating room and opened only as needed. These include a clip applier, linear vascular stapler, suction irrigator, and fan retractor.
Patient Positioning and Operating Room Setup
The patient is placed supine, and straps are used to secure the patient during steep table position changes. The patient is fixed in a moldable "bean bag" form with both arms tucked in, and placed in a modified lithotomy position using levitator stirrups. A urinary catheter is placed in the bladder, and the stomach is decompressed with a nasogastric tube. Identical operating room personnel is used for the laparoscopic case as for an open right hemicolectomy. The nurse is on the patient's right. This is also where the assistant starts, with the surgeon on the patient's left side facing the right colon. Hasson (open) technique is preferred to safely insert the first port through the umbilicus. After establishing pneumoperitoneum, the surgeon stands on the patient's left side to expose the right mesocolon and to mark the lower border of the ileocolic vessels.
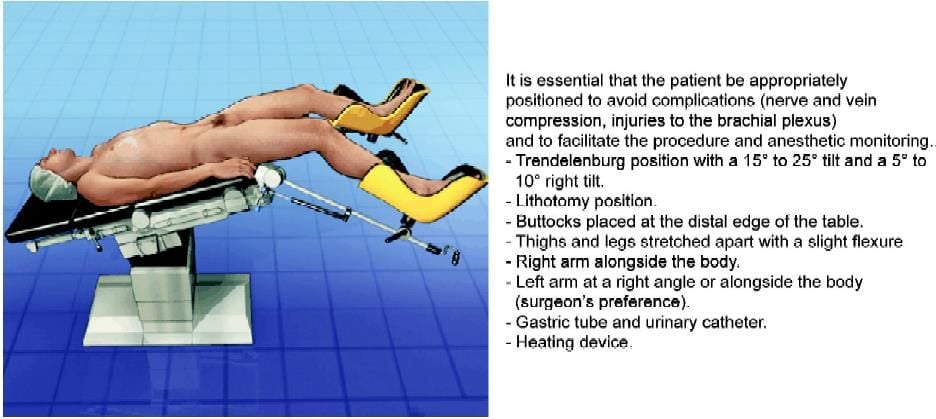
Position of the patient for colorectal surgery
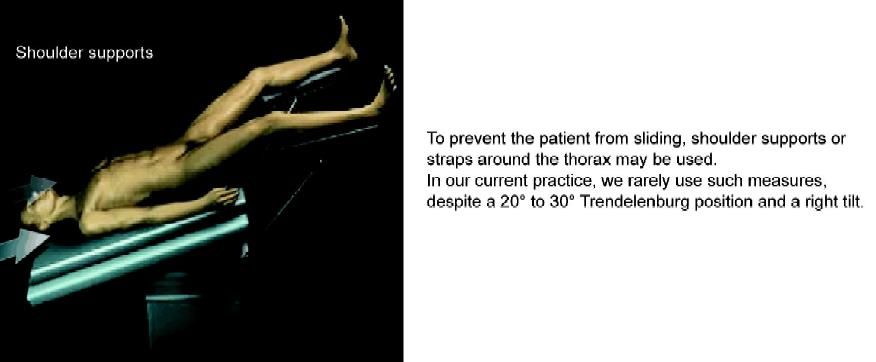
Shoulder support to prevent sliding during colorectal surgery
After initial exploration ensures no prohibitive adhesions, two additional 10 to 12 mm ports are placed under direct visualization, one in the left upper quadrant (in or lateral to the rectus, avoiding the epigastric vessels, approximately a handbreadth from the supraumbilical port) and one in the suprapubic midline. Once all the trocars are in place, the assistant moves to the patient's left side to direct the camera. To start the initial dissection the surgeon moves between the patient's legs, the assistants position themselves on the patient's left side and the nurse stands near the patient's right knee. The main monitor is placed near the patient's right shoulder to give the surgeon and the assistant's optimal viewing. The second monitor is placed on the left side close to the head, a location that gives the best view for the nurse. After completing the proximal vessel ligation with lymphadenectomy and mobilization of the terminal ileum and the cecum, the surgeon moves back to the patient's left side and the first assistant stands between the patient's legs for take-down of right flexure and whole mobilization of the right colon.
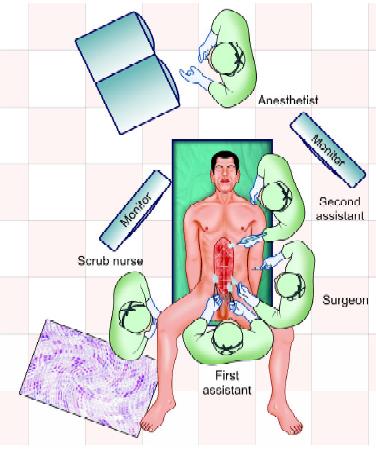
Position of the surgical team during colorectal surgery
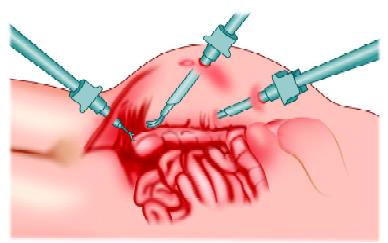
Mobilization of the cecum and right colon
Operative Technique
Right colectomy can be broadly divided into the following steps:
• Ligation of ileocolic vessels
• Identification of right ureter
• Dissection along the superior mesenteric vein
• Division of omentum
• Division of the right branch of middle colic vessels
• Transection of the transverse colon
• Mobilization of the right colon
• Transection of the terminal ileum
• Ileocolic anastomosis
• Delivery of specimen
The patient is positioned in Trendelenburg with the right side inclined upward. This allows the small bowel and omentum to fall toward the left upper quadrant, exposing the cecum and assisting in retraction. The omentum and transverse colon are moved toward the upper abdomen, the ventral side of the right mesocolon is well visualized, and the optimal operative field can be achieved. The small bowel is mobilized out of the pelvis by grasping the peritoneum, not bowel wall, near the base of the cecum, and pulling cephalad and to the left. The appropriate plane along the base of the small bowel mesentery and around the cecum can be seen and the peritoneum overlying it carefully opened, exposing the correct retroperitoneal plane. The ureter is identified either before opening the peritoneum in a thin patient or after, being visualized as it courses over the right iliac vessels. Dissection is then continued around the base of the cecum. Moving cephalad and laterally, the white line of Toldt is incised as the right colon is retracted medially and cephalad by grasping the cut edge of the peritoneum, not the bowel.
Before starting the dissection, the ileocolic pedicle must be definitively identified by retracting the right mesocolon. Various approaches, such as lateral-to-medial (lateral approach), medial-to-lateral (medial approach), and retroperitoneal approach can be tried. The medial approach is quite effective for complete lymphadenectomy with early proximal ligation, minimal manipulation of the tumor-bearing segment, and ideal entry to proper retroperitoneal plane.
Various approaches to the right colon mobilization have been described.
A: Lateral to medial ("classic" open approach);
B: Medial to lateral approach);
C: Retroperitoneal approach.
It is believed that the medial approach is optimal in order to maintain conventional oncologic principles. First, the mesocolon near the ileocecal junction is lifted to confirm the ileocolic pedicle. The root of the ileocolic pedicle is usually located at the lower border of the duodenum. The independent right colic vessels, if present, are located at the upper border at the duodenum. However, the majority of patients do not have the independent right colic vessels (vessels originating directly from the superior mesenteric artery and vein. The surgeon should initially stand on the patient's left side to confidently know the ileocolic pedicle from the superior mesenteric vessels, and to mark the lower border of the ileocolic pedicle.
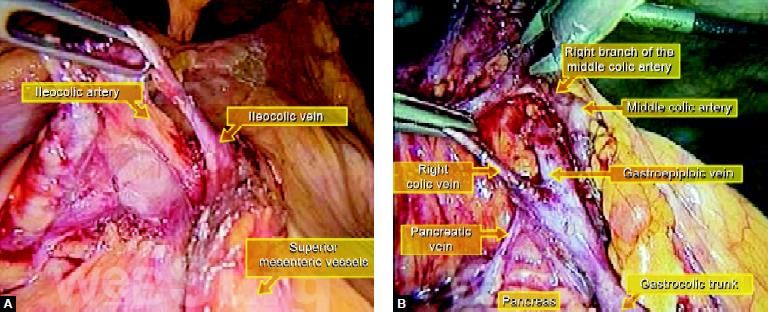
(A) Position of major blood vessels at the time of surgery; (B) Important vessels supplying right side of the colon
Once the ileocolic pedicle is identified, the surgeon moves between the patient's legs, and the scope is inserted through the suprapubic port. The medial side of the right mesocolon is first incised starting from the previously marked region below the ileocolic pedicle, followed by the incision of the peritoneum over to the superior mesenteric vessels. This is done before mobilization of the right colon. With adequate traction of mesocolon toward the right upper quadrant, the ileocolic vessels are easily mobilized from the subperitoneal fascia leading onto the duodenum. Their origins are identified from the superior mesenteric vessels at the lower border of the duodenum and divided.
The surgeon's first step in the dissection is to mark the inferior border of the ileocolic pedicle. From between the legs, the surgeon dissects the peritoneum overlying the ileocolic vascular pedicle over to the superior mesenteric vessels. After mobilization of the ileocolic pedicle from the duodenum, the dissection of the ventral side of the superior mesenteric vein leads to the dissection of the origin of the ileocolic artery. In type B, the ileocolic artery is running behind the superior mesenteric vein. After mobilization and division of the ileocolic pedicle from the duodenum, the dissection of the ventral side of the superior mesenteric vein leads to a complete dissection of the root of the middle colic artery and vein. Careful dissection onto the duodenum and the caudad portion of the pancreas must be exercised in the exposure of the middle colic vessels. Dissection around Henle's trunk (the truck of mesenteric veins consisting of the gastroepiploic vein fusing with the right branch of the middle colic vein or the main middle colic vein) may lead to the exposure of an accessory right colic vein. Accessory right colic vein and right branches of middle colic vessels are clipped and divided. However, if an accessory right colic vein is difficult to confirm in this situation, this vein may be easily detected later at the take-down of the right flexure.
After securing the vessels, the operating table is tilted into the steep Trendelenburg position with the right side down to move the small intestine toward the right upper quadrant. After confirming the right ureter and gonadal vessels through the subperitoneal fascia at the right pelvic brim, the peritoneum is incised along the base of the ileal mesentery upward to the duodenum, and the ileocecal region is mobilized medial to lateral. After this mobilization, the surgeon moves back to the patient's left side and the scope is inserted through the umbilical port. The right mesocolon is mobilized from medial to lateral. Again, this approach allows dissection into the proper retroperitoneal plane. The right gonadal vessels and ureter are safe from injury in this plane, so exposing them is not necessary. This approach also allows the surgeon to work in a straight path from medial to lateral, without tissue to obstruct the vision that can occur working from lateral to medial. This plane connects the previous dissection plane from the caudad side.
The anatomy around the right flexure is very important to avoid inadvertent bleeding especially from around Henle's (gastrocolic) trunk. However, if the previous mesenteric dissection is fully performed from the caudad side and the accessory right colic vein is divided, the right flexure is easily taken down only by dividing the hepatocolic ligament. If the accessory right colic vein is difficult to detect at the previous dissection, it can be easily confirmed from Henle's trunk at this situation and should be divided before extracting the right colon to avoid its injury. Up to this point, the primary tumor has been minimally manipulated using medial to lateral approach. Finally, the right flexure and right colon including the tumor-bearing segment are detached laterally, which completes the mobilization of the entire right colon.

Specimen of the right side of the colon after right colectomy
Once the entire right colon is freed, it is withdrawn through an enlargement of the port site at the umbilicus. The wound must be covered with a wound protector to prevent contamination or metastasis. The resection of ileum and transverse colon, and the anastomosis are accomplished extracorporeally by the functional end to end anastomotic method using conventional staplers or by a hand-sewn method. The anastomotic site is returned to the peritoneal cavity. Wounds and peritoneal cavity are copiously irrigated. All wounds are closed and operation is completed.

Transaction of ileum by the stapler
The identification of a small tumor in the colon may be difficult even in conventional open surgery. In laparoscopic surgery, where there is no tactile sensation, pre- or intraoperative marking of the tumor is frequently needed. Various kinds of marking methods,
e.g. dye injection and mucosal clip placement by preoperative colonoscopy, have been reported for the tumor localization. Several reports demonstrated the usefulness of tattooing the colonic wall adjacent to the tumor with India ink in four quadrants using preoperative colonoscopy.
However, effective injection in all four points of the bowel is sometimes difficult to achieve. In some cases, the surgeon failed to achieve serosal staining visible at laparoscopy, which forced them to use intraoperative colonoscopy. This complicated the laparoscopic colon resection because of the distended bowel related to air insufflation during colonoscopy.
Conclusion
Right-sided colon cancer can be adequately treated by proper laparoscopic procedures adherent to the oncologic principles. Port-site metastasis after laparoscopic colon cancer surgery is unlikely to be a major risk factor when the procedure is performed according to oncologic principles (Refer to Chapter 6). It is believed that laparoscopic right colectomy for cancer performed by expert surgeons is accepted as less invasive surgery without sacrificing the survival benefit compared with conventional open right colectomy.





