Laparoscopic Resection Rectopexy
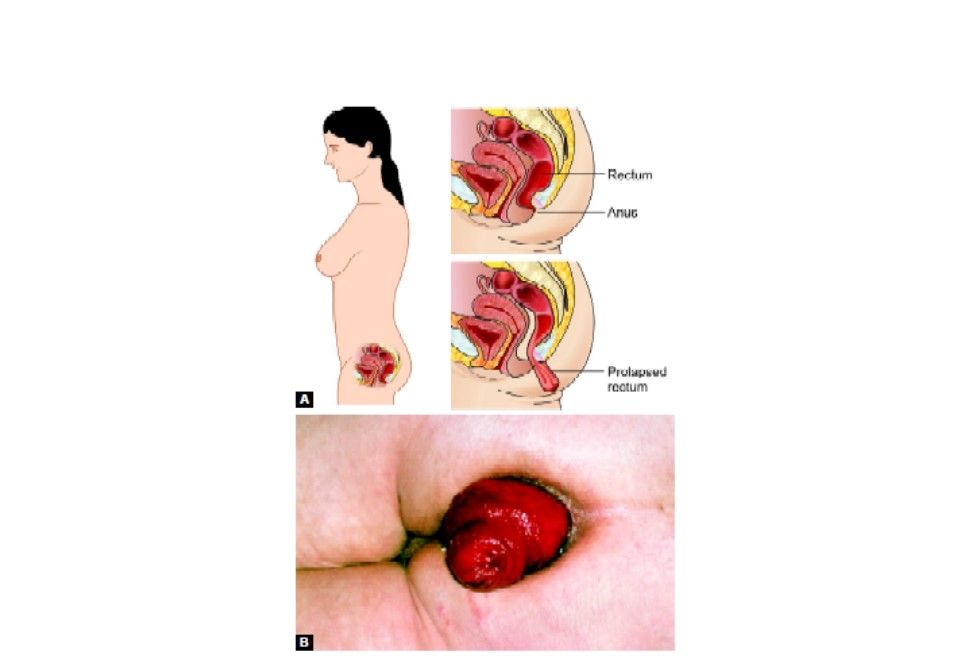
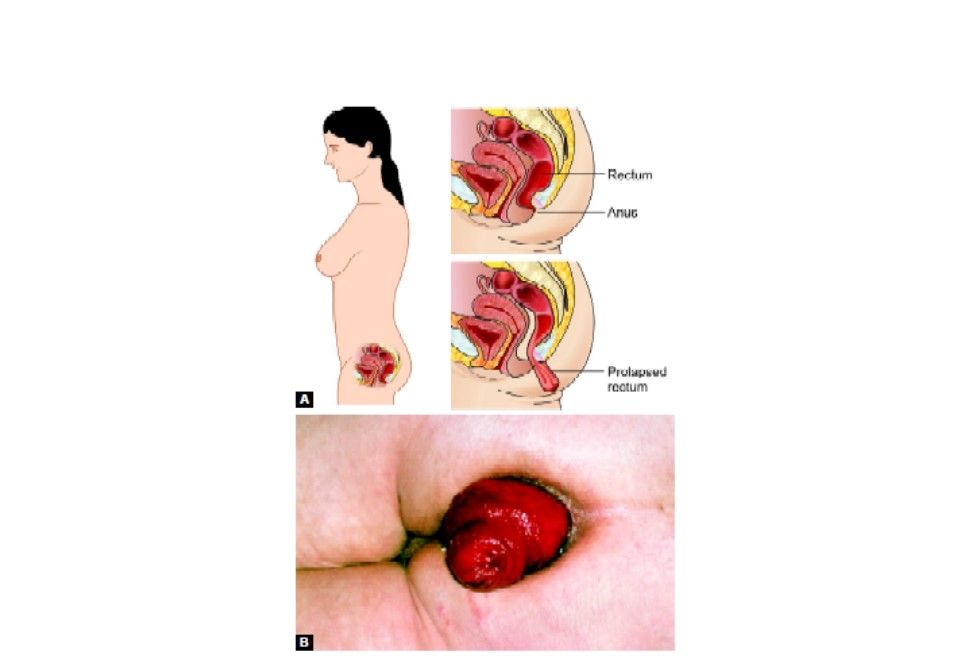
Total rectal prolapse with chronic constipation and anal incontinence is a devastating disorder. It is more common in the elderly, especially women, although why it happens is unclear. Rectal prolapse can cause complications (such as pain, ulcers, and bleeding), and cause fecal incontinence. Surgery is commonly used to repair the prolapse. Rectopexy with or without bowel resection is the most frequent surgical procedure, with 0 to 9 percent recurrence rates in many years. Laparoscopic resection rectopexy is safely feasible as a minimally-invasive treatment option for rectal prolapse.
Rectal Prolapse
Patient Position
The patient is placed supine on the operating table, on a beanbag. After induction of general anesthesia and insertion of an orogastric tube and Foley catheter, the legs are placed in Dan Allen stirrups. The arms are tucked at the patient's side. The abdomen is prepared with an antiseptic solution and draped routinely.
Position of Surgical Team
The primary monitor is placed on the left side of the patient at approximately the level of the hip. The secondary monitor is placed on the right side of the patient at the same level and is primarily for the assistant during the early phase of the surgery and port insertion. The operating nurse's instrument table is placed between the patient's legs. There should be sufficient space to allow the surgeon to move from either side of the patient to between the patient's legs, if necessary. The primary operating surgeon stands on the right side of the patient with the assistant standing on the patient's left and moving to the right side, caudad to the surgeon once ports have been inserted. A 0-degree camera lens is used.
Port Position
This is performed using a Hasson approach. A smiling 10 mm sub umbilical incision is made. This is deepened down to the linea alba, which is then grasped on each side of the midline using Kocher clamps. A scalpel (No. 15 blade) is used to open the fascia between the Kocher clamps and a Kelly forceps is used to open the peritoneum bluntly. The telescope is inserted into the abdomen and an initial laparoscopy is performed, carefully evaluating the liver, small bowel, and peritoneal surfaces. A 12 mm port is inserted in the right lower quadrant approximately 2 to 3 cm medial and superior to the anterior superior iliac spine. This is carefully inserted lateral to the inferior epigastric vessels, paying attention to keep the tract of the port going as perpendicular as possible through the abdominal wall. A 5 mm port is then inserted in the right upper quadrant at least a hand's breadth superior to the lower quadrant port. A left lower quadrant 5 mm port is inserted. All the ports are more or less obeying the baseball diamond concept.
Dissection
The patient is rotated with the left side up and right side down, to approximately 15 to 20 degrees tilt, and often as far as the table can go. This helps to move the small bowel over to the right side of the abdomen. The patient is then placed in the Trendelenburg position. This again helps gravitational migration of the small bowel away from the operative field. The surgeon then inserts two atraumatic bowel clamps through the two right-sided abdominal ports. The greater omentum is reflected over the transverse colon so that it comes to lie on the stomach. If there is no space in the upper part of the abdomen one must confirm that the orogastric tube is adequately decompressing the stomach. The small bowel is moved to the patient's right side allowing visualization of the medial aspect of the rectosigmoid mesentery. This may necessitate the use of the assistant's 5 mm atraumatic bowel clamp through the left lower quadrant to tent the sigmoid mesentery cephalad.
Division of Inferior Mesenteric Vessel
An atraumatic bowel clamp is placed on the rectosigmoid mesentery at the level of the sacral promontory, approximately halfway between the bowel wall and the promontory itself. This area is then stretched up towards the left lower quadrant port, stretching the inferior mesenteric vessels away from the retroperitoneum. In most cases, this demonstrates a groove between the right or medial side of the inferior mesenteric pedicle and the retroperitoneum. Cautery is used to open the peritoneum along this line, opening the plane cranially up to the origin of the inferior mesenteric artery, and caudally past the sacral promontory. Blunt dissection is then used to lift the vessels away from the retroperitoneum and presacral autonomic nerves. The ureter is then looked for under the inferior mesenteric artery. If the ureter cannot be seen, and the dissection is in the correct plane, the ureter should be just deep to the parietal peritoneum, and just medial to the gonadal vessels. Care must be taken not to dissect too deep or caudad leading to injury of the iliac vessels.
If the ureter cannot be found, it has usually been elevated on the back of the inferior mesenteric pedicle, and one needs to stay very close to the vessel not only to find the ureter but also to protect the autonomic nerves. If the ureter still cannot be found, the dissection needs to come in a cranial dissection, which is usually into clean tissue allowing it to be found. If this fails, a lateral approach can be performed. This usually gives a fresh perspective to the tissues, and the ureter can often be found quite easily. In very rare cases the ureter still may not be found.
The dissection should allow sufficient mobilization of the inferior mesenteric artery so that the origin of the left colic artery is seen. The vessel is carefully defined and divided just distal to the left colic artery. A clamp is placed on the origin of the vessel to control it if clips or other energy sources do not adequately control the vessel. In general, a cartridge of the endoscopic linear stapler is used to divide the vessel. Having divided the pedicle, the plane between the sigmoid colon mesentery and the retroperitoneum is developed laterally, out towards the lateral attachment of the colon. Limited mobilization of the mesentery off the anterior surface of Gerota's fascia and of the left colon should be performed to enhance the fixation of the rectum.
Mobilization of the Lateral Attachments of the Rectosigmoid
The surgeon now grasps the rectosigmoid junction with his left-hand instrument and draws it to the patient's right side. This allows the lateral attachments of the sigmoid colon to be seen and divided using cautery. Bruising from the prior retroperitoneal mobilization of the colon can usually be seen in this area. Once this layer of peritoneum has been opened, one immediately enters into the space opened by the retroperitoneal dissection. No dissection should be performed more proximally along the white line of Toldt, toward the splenic flexure.
Mobilization of Rectum
An atraumatic bowel clamp inserted through the left lower quadrant port is used to elevate the rectosigmoid colon out of the pelvis and away from the retroperitoneum and sacral promontory, to enable entry into the presacral space. The posterior aspect of the mesorectum can be identified and the mesorectal plane dissected with diathermy, preserving the hypogastric nerves as they pass down into the pelvis anterior to the sacrum. Dissection continues down the presacral space in this avascular plane toward the pelvic floor. Only the posterior 60 percent of the rectum needs to be mobilized; however, dissection should be continued all the way to the levator ani muscles. A transanal examining finger should be used to confirm the distal extent of the dissection. The lateral stalks should be preserved. The peritoneum on either side of the rectum should be incised to the level of the lateral stalks. The lateral stalks should generally be preserved, the exception being when further dissection must completely reduce a very distal prolapsing segment.
Rectal Division
The fully mobilized rectum should be elevated out of the pelvis and a site selected for optimal rectal tension to maintain a full reduction of the prolapse. A site for rectal division should be chosen in proximal, peritonealized rectum, which assures that the anastomosis will be rostral to the sacral promontory. The rectum is divided laparoscopically with a linear endoscopic stapler through the right lower quadrant trocar. One or two firings of the stapler may be required to divide the rectum. The mesorectum is divided using monopolar and bipolar cautery at this level.
Specimen Extraction and Anastomosis
The specimen is extracted through a left iliac fossa incision. Before making the incision, the proximal colonic transaction point should be grasped with a locking atraumatic bowel grasper. This site should allow a colorectal anastomosis that will provide a safe amount of tension on the rectum to maintain prolapse reduction. After extracorporeal bowel transaction, adequate vascularity of the colon should be assured. A 2/0 Prolene purse-string suture is inserted into the distal end of the left colon, the anvil of a circular stapling gun is inserted and the purse-string suture is tied tightly. The colon is returned to the abdomen and the left iliac fossa incision is closed in layers with 0 polyglycolic acid suture. Pneumoperitoneum is recreated, and the circular stapled anastomosis is formed under laparoscopic guidance. The anastomosis can be leak-tested by filling the pelvis with saline and inflating the neorectum using a proctoscope or bulb syringe.
Rectopexy
The rectum is retracted rostrally to the desired tension to allow complete reduction of the prolapse. The rectopexy is then performed from the right side using the two remaining ports. Two or three nonabsorbable sutures are used to attach the mesorectum distal to the anastomosis to the sacral promontory. Alternatively, nitinol or titanium tackers may be employed using one of the mechanical fixation devices used for mesh hernia repairs.
Total rectal prolapse with chronic constipation and anal incontinence is a devastating disorder. It is more common in the elderly, especially women, although why it happens is unclear. Rectal prolapse can cause complications (such as pain, ulcers, and bleeding), and cause fecal incontinence. Surgery is commonly used to repair the prolapse. Rectopexy with or without bowel resection is the most frequent surgical procedure, with 0 to 9 percent recurrence rates in many years. Laparoscopic resection rectopexy is safely feasible as a minimally-invasive treatment option for rectal prolapse.
Rectal Prolapse
Patient Position
The patient is placed supine on the operating table, on a beanbag. After induction of general anesthesia and insertion of an orogastric tube and Foley catheter, the legs are placed in Dan Allen stirrups. The arms are tucked at the patient's side. The abdomen is prepared with an antiseptic solution and draped routinely.
Position of Surgical Team
The primary monitor is placed on the left side of the patient at approximately the level of the hip. The secondary monitor is placed on the right side of the patient at the same level and is primarily for the assistant during the early phase of the surgery and port insertion. The operating nurse's instrument table is placed between the patient's legs. There should be sufficient space to allow the surgeon to move from either side of the patient to between the patient's legs, if necessary. The primary operating surgeon stands on the right side of the patient with the assistant standing on the patient's left and moving to the right side, caudad to the surgeon once ports have been inserted. A 0-degree camera lens is used.
Port Position
This is performed using a Hasson approach. A smiling 10 mm sub umbilical incision is made. This is deepened down to the linea alba, which is then grasped on each side of the midline using Kocher clamps. A scalpel (No. 15 blade) is used to open the fascia between the Kocher clamps and a Kelly forceps is used to open the peritoneum bluntly. The telescope is inserted into the abdomen and an initial laparoscopy is performed, carefully evaluating the liver, small bowel, and peritoneal surfaces. A 12 mm port is inserted in the right lower quadrant approximately 2 to 3 cm medial and superior to the anterior superior iliac spine. This is carefully inserted lateral to the inferior epigastric vessels, paying attention to keep the tract of the port going as perpendicular as possible through the abdominal wall. A 5 mm port is then inserted in the right upper quadrant at least a hand's breadth superior to the lower quadrant port. A left lower quadrant 5 mm port is inserted. All the ports are more or less obeying the baseball diamond concept.
Dissection
The patient is rotated with the left side up and right side down, to approximately 15 to 20 degrees tilt, and often as far as the table can go. This helps to move the small bowel over to the right side of the abdomen. The patient is then placed in the Trendelenburg position. This again helps gravitational migration of the small bowel away from the operative field. The surgeon then inserts two atraumatic bowel clamps through the two right-sided abdominal ports. The greater omentum is reflected over the transverse colon so that it comes to lie on the stomach. If there is no space in the upper part of the abdomen one must confirm that the orogastric tube is adequately decompressing the stomach. The small bowel is moved to the patient's right side allowing visualization of the medial aspect of the rectosigmoid mesentery. This may necessitate the use of the assistant's 5 mm atraumatic bowel clamp through the left lower quadrant to tent the sigmoid mesentery cephalad.
Division of Inferior Mesenteric Vessel
An atraumatic bowel clamp is placed on the rectosigmoid mesentery at the level of the sacral promontory, approximately halfway between the bowel wall and the promontory itself. This area is then stretched up towards the left lower quadrant port, stretching the inferior mesenteric vessels away from the retroperitoneum. In most cases, this demonstrates a groove between the right or medial side of the inferior mesenteric pedicle and the retroperitoneum. Cautery is used to open the peritoneum along this line, opening the plane cranially up to the origin of the inferior mesenteric artery, and caudally past the sacral promontory. Blunt dissection is then used to lift the vessels away from the retroperitoneum and presacral autonomic nerves. The ureter is then looked for under the inferior mesenteric artery. If the ureter cannot be seen, and the dissection is in the correct plane, the ureter should be just deep to the parietal peritoneum, and just medial to the gonadal vessels. Care must be taken not to dissect too deep or caudad leading to injury of the iliac vessels.
If the ureter cannot be found, it has usually been elevated on the back of the inferior mesenteric pedicle, and one needs to stay very close to the vessel not only to find the ureter but also to protect the autonomic nerves. If the ureter still cannot be found, the dissection needs to come in a cranial dissection, which is usually into clean tissue allowing it to be found. If this fails, a lateral approach can be performed. This usually gives a fresh perspective to the tissues, and the ureter can often be found quite easily. In very rare cases the ureter still may not be found.
The dissection should allow sufficient mobilization of the inferior mesenteric artery so that the origin of the left colic artery is seen. The vessel is carefully defined and divided just distal to the left colic artery. A clamp is placed on the origin of the vessel to control it if clips or other energy sources do not adequately control the vessel. In general, a cartridge of the endoscopic linear stapler is used to divide the vessel. Having divided the pedicle, the plane between the sigmoid colon mesentery and the retroperitoneum is developed laterally, out towards the lateral attachment of the colon. Limited mobilization of the mesentery off the anterior surface of Gerota's fascia and of the left colon should be performed to enhance the fixation of the rectum.
Mobilization of the Lateral Attachments of the Rectosigmoid
The surgeon now grasps the rectosigmoid junction with his left-hand instrument and draws it to the patient's right side. This allows the lateral attachments of the sigmoid colon to be seen and divided using cautery. Bruising from the prior retroperitoneal mobilization of the colon can usually be seen in this area. Once this layer of peritoneum has been opened, one immediately enters into the space opened by the retroperitoneal dissection. No dissection should be performed more proximally along the white line of Toldt, toward the splenic flexure.
Mobilization of Rectum
An atraumatic bowel clamp inserted through the left lower quadrant port is used to elevate the rectosigmoid colon out of the pelvis and away from the retroperitoneum and sacral promontory, to enable entry into the presacral space. The posterior aspect of the mesorectum can be identified and the mesorectal plane dissected with diathermy, preserving the hypogastric nerves as they pass down into the pelvis anterior to the sacrum. Dissection continues down the presacral space in this avascular plane toward the pelvic floor. Only the posterior 60 percent of the rectum needs to be mobilized; however, dissection should be continued all the way to the levator ani muscles. A transanal examining finger should be used to confirm the distal extent of the dissection. The lateral stalks should be preserved. The peritoneum on either side of the rectum should be incised to the level of the lateral stalks. The lateral stalks should generally be preserved, the exception being when further dissection must completely reduce a very distal prolapsing segment.
Rectal Division
The fully mobilized rectum should be elevated out of the pelvis and a site selected for optimal rectal tension to maintain a full reduction of the prolapse. A site for rectal division should be chosen in proximal, peritonealized rectum, which assures that the anastomosis will be rostral to the sacral promontory. The rectum is divided laparoscopically with a linear endoscopic stapler through the right lower quadrant trocar. One or two firings of the stapler may be required to divide the rectum. The mesorectum is divided using monopolar and bipolar cautery at this level.
Specimen Extraction and Anastomosis
The specimen is extracted through a left iliac fossa incision. Before making the incision, the proximal colonic transaction point should be grasped with a locking atraumatic bowel grasper. This site should allow a colorectal anastomosis that will provide a safe amount of tension on the rectum to maintain prolapse reduction. After extracorporeal bowel transaction, adequate vascularity of the colon should be assured. A 2/0 Prolene purse-string suture is inserted into the distal end of the left colon, the anvil of a circular stapling gun is inserted and the purse-string suture is tied tightly. The colon is returned to the abdomen and the left iliac fossa incision is closed in layers with 0 polyglycolic acid suture. Pneumoperitoneum is recreated, and the circular stapled anastomosis is formed under laparoscopic guidance. The anastomosis can be leak-tested by filling the pelvis with saline and inflating the neorectum using a proctoscope or bulb syringe.
Rectopexy
The rectum is retracted rostrally to the desired tension to allow complete reduction of the prolapse. The rectopexy is then performed from the right side using the two remaining ports. Two or three nonabsorbable sutures are used to attach the mesorectum distal to the anastomosis to the sacral promontory. Alternatively, nitinol or titanium tackers may be employed using one of the mechanical fixation devices used for mesh hernia repairs.


