Laparoscopic Oophorectomy
An oophorectomy is a procedure to remove one or both of a woman's ovaries. A unilateral oophorectomy removes one ovary; a bilateral oophorectomy removes both.
Indications of Oophorectomy
The most common indications for oophorectomy are:
• Persistent localized pain despite previous lysis of adhesions or ablation of endometriosis
• Residual ovary syndrome
• Dysgenetic gonads
• Ovarian cysts greater than 5 cm
• Tubo-ovarian abscess
• Prophylactic therapy for advanced breast cancer
• Early ovarian cancer in young women.
Contradictions
• Hemodynamic instability
• Uncorrected coagulopathy
• Severe cardiopulmonary disease
• Abdominal wall infection
• Multiple previous upper abdominal procedures
• Late pregnancy.

Laparoscopic Oophorectomy
Operative Procedure
The port position is shown in the image below. A properly placed uterine manipulator is important to get a good exposure of ovary and tube. It is sometimes difficult to immobilize the ovary because of its smooth surface and finer texture. In case of difficulty in immobilizing the ovary, the uterine- ovarian ligament can be grasped by one of the atraumatic graspers to lift and isolate the ovary or the ovary can be wedged against the pelvic sidewall using the flattened edges of the opened or closed forceps. It is important to remember that overly aggressive manipulation can cause lacerations in the capsule, follicles, or cysts and result in bleeding. Before starting the procedure, it is important to observe the course of the ureter as it crosses the external iliac artery near the bifurcation of the common iliac artery at the pelvic brim. The left ureter can be more difficult to find because it is often covered by the base of the sigmoid mesocolon.
If the ureter is difficult to identify transperitoneal it must be identified by a retroperitoneal approach. If the previous hysterectomy is done it is better to insert a vaginal probe or sponge stick through the vagina so that the surgeon can maintain orientation, particularly with procedures involving extensive adhesions. Many times anatomic landmarks are distorted by adhesions, endometriosis, or prior surgical extirpation. In those cases, dissection should be started from the most normal area, and then it should proceed toward the more distorted parts of the operative field. Attention should be given that a complete ovary must be removed to prevent ovarian remnant syndrome or tumor development in a dysgenetic gonad. At the end of the procedure, the operative field is inspected and any clots are removed with a suction-irrigator or grasping forceps. Pedicles are inspected underwater and with decreased pneumoperitoneum and any bleeding if present can be controlled with bipolar electrocoagulation.
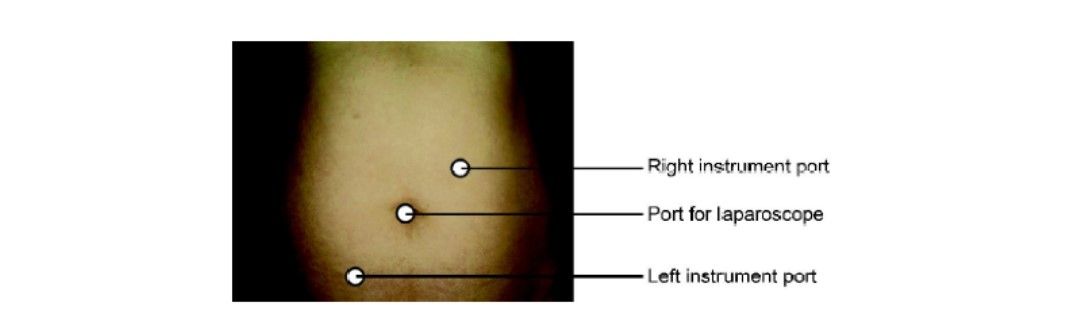
Port position for laparoscopic left oophorectomy
Dissection of the Infundibulopelvic Ligament
Three techniques have been described for managing the infundibulopelvic ligament:
• Bipolar electrodesiccation
• Suture ligation with pretied loop
• Stapling.
Patient cost for the linear stapler is approximately Rs 4500 and Rs 250 for each pretied ligature. Considering these expenses bipolar electrosurgery is the most economical way of dissection and it is preferable for hemostasis of the infundibulopelvic ligament. Endoloop cannot be applied in the presence of adhesions and distorted anatomy. Sometimes it is difficult to place endoloop sutures on a large bunch of pedicles such as the mesovarium and infundibulopelvic ligament. If an extracorporeal slip knot is applied over a wide pedicle, the slipknot can loosen under the tension of the large pedicle. It may increase the risk of intraoperative hemorrhage. If the stump is large a piece of the ovary may be left in the pedicle, predisposing the patient to ovarian remnant syndrome.
Aside from the cost, the linear stapling device has several other drawbacks. It should be introduced through a 12 mm trocar. Insertion of a bigger trocar can lead to injury of the inferior epigastric artery and predispose the patient to a postoperative hernia. The linear stapler instrument is bulky and the operator must be careful to its proximity to the ureter, bowel, and bladder. If the correct size staple is not selected the staples may dislodge and bleeding may start.
Salpingo-oophorectomy
If complete salpingo-oophorectomy is planned, the ovary and tube can be approached either from the infundibulopelvic or utero-ovarian ligament. Filmy adhesion limiting the mobilization of ovary should be dissected first. If an ovarian cyst is found it should be aspirated and deflated, making removal of the ovary easier. The preferred approach is dissection should begin with the infundibulo ligament because it is easier and this approach is essential if prior hysterectomy is performed. The lateral approach is essential if the hemostasis from the ovarian vessel is thought. The ovary is held with a grasping forceps and the infundibulopelvic ligament is put under traction by pulling it up and medially. The infundibulopelvic ligament is desiccated with bipolar forceps and cut with scissors from lateral to medial. It is important to use appropriate traction away from the lateral pelvic wall to prevent excessive coagulation and damage to the lateral pelvic structures like ureter or vessels in the triangle of doom. Laparoscopic linear stapling and cutting device can also be used for salpingo-oophorectomy in selected cases. Laparoscopic extracorporeal Roeader’s or Meltzer's knot can also be applied. A pretied loop is easy to use but pedicle should not be wide. In cases of the wide pedicel, a window can be created in the midpoint of infundibulopelvic ligament and extracorporeal knot for continuous structure should be applied.

Dissection at the level of the infundibulopelvic ligament
Dysgenic Gonads
Sometime dysgenic gonads can be found at the time of laparoscopy and require gonadectomy to prevent gonadoblastoma. The laparoscopic removal technique of dysgenic gonad is the same as removing an ovary with adhesion to the lateral pelvic wall. In these difficult cases, hydro dissection is of utmost importance.
An oophorectomy is a procedure to remove one or both of a woman's ovaries. A unilateral oophorectomy removes one ovary; a bilateral oophorectomy removes both.
Indications of Oophorectomy
The most common indications for oophorectomy are:
• Persistent localized pain despite previous lysis of adhesions or ablation of endometriosis
• Residual ovary syndrome
• Dysgenetic gonads
• Ovarian cysts greater than 5 cm
• Tubo-ovarian abscess
• Prophylactic therapy for advanced breast cancer
• Early ovarian cancer in young women.
Contradictions
• Hemodynamic instability
• Uncorrected coagulopathy
• Severe cardiopulmonary disease
• Abdominal wall infection
• Multiple previous upper abdominal procedures
• Late pregnancy.

Laparoscopic Oophorectomy
Operative Procedure
The port position is shown in the image below. A properly placed uterine manipulator is important to get a good exposure of ovary and tube. It is sometimes difficult to immobilize the ovary because of its smooth surface and finer texture. In case of difficulty in immobilizing the ovary, the uterine- ovarian ligament can be grasped by one of the atraumatic graspers to lift and isolate the ovary or the ovary can be wedged against the pelvic sidewall using the flattened edges of the opened or closed forceps. It is important to remember that overly aggressive manipulation can cause lacerations in the capsule, follicles, or cysts and result in bleeding. Before starting the procedure, it is important to observe the course of the ureter as it crosses the external iliac artery near the bifurcation of the common iliac artery at the pelvic brim. The left ureter can be more difficult to find because it is often covered by the base of the sigmoid mesocolon.
If the ureter is difficult to identify transperitoneal it must be identified by a retroperitoneal approach. If the previous hysterectomy is done it is better to insert a vaginal probe or sponge stick through the vagina so that the surgeon can maintain orientation, particularly with procedures involving extensive adhesions. Many times anatomic landmarks are distorted by adhesions, endometriosis, or prior surgical extirpation. In those cases, dissection should be started from the most normal area, and then it should proceed toward the more distorted parts of the operative field. Attention should be given that a complete ovary must be removed to prevent ovarian remnant syndrome or tumor development in a dysgenetic gonad. At the end of the procedure, the operative field is inspected and any clots are removed with a suction-irrigator or grasping forceps. Pedicles are inspected underwater and with decreased pneumoperitoneum and any bleeding if present can be controlled with bipolar electrocoagulation.
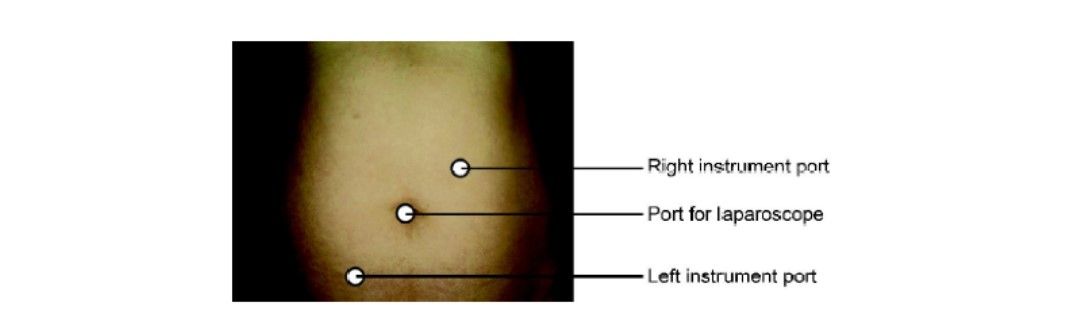
Port position for laparoscopic left oophorectomy
Dissection of the Infundibulopelvic Ligament
Three techniques have been described for managing the infundibulopelvic ligament:
• Bipolar electrodesiccation
• Suture ligation with pretied loop
• Stapling.
Patient cost for the linear stapler is approximately Rs 4500 and Rs 250 for each pretied ligature. Considering these expenses bipolar electrosurgery is the most economical way of dissection and it is preferable for hemostasis of the infundibulopelvic ligament. Endoloop cannot be applied in the presence of adhesions and distorted anatomy. Sometimes it is difficult to place endoloop sutures on a large bunch of pedicles such as the mesovarium and infundibulopelvic ligament. If an extracorporeal slip knot is applied over a wide pedicle, the slipknot can loosen under the tension of the large pedicle. It may increase the risk of intraoperative hemorrhage. If the stump is large a piece of the ovary may be left in the pedicle, predisposing the patient to ovarian remnant syndrome.
Aside from the cost, the linear stapling device has several other drawbacks. It should be introduced through a 12 mm trocar. Insertion of a bigger trocar can lead to injury of the inferior epigastric artery and predispose the patient to a postoperative hernia. The linear stapler instrument is bulky and the operator must be careful to its proximity to the ureter, bowel, and bladder. If the correct size staple is not selected the staples may dislodge and bleeding may start.
Salpingo-oophorectomy
If complete salpingo-oophorectomy is planned, the ovary and tube can be approached either from the infundibulopelvic or utero-ovarian ligament. Filmy adhesion limiting the mobilization of ovary should be dissected first. If an ovarian cyst is found it should be aspirated and deflated, making removal of the ovary easier. The preferred approach is dissection should begin with the infundibulo ligament because it is easier and this approach is essential if prior hysterectomy is performed. The lateral approach is essential if the hemostasis from the ovarian vessel is thought. The ovary is held with a grasping forceps and the infundibulopelvic ligament is put under traction by pulling it up and medially. The infundibulopelvic ligament is desiccated with bipolar forceps and cut with scissors from lateral to medial. It is important to use appropriate traction away from the lateral pelvic wall to prevent excessive coagulation and damage to the lateral pelvic structures like ureter or vessels in the triangle of doom. Laparoscopic linear stapling and cutting device can also be used for salpingo-oophorectomy in selected cases. Laparoscopic extracorporeal Roeader’s or Meltzer's knot can also be applied. A pretied loop is easy to use but pedicle should not be wide. In cases of the wide pedicel, a window can be created in the midpoint of infundibulopelvic ligament and extracorporeal knot for continuous structure should be applied.

Dissection at the level of the infundibulopelvic ligament
Dysgenic Gonads
Sometime dysgenic gonads can be found at the time of laparoscopy and require gonadectomy to prevent gonadoblastoma. The laparoscopic removal technique of dysgenic gonad is the same as removing an ovary with adhesion to the lateral pelvic wall. In these difficult cases, hydro dissection is of utmost importance.





