Laparoscopic Management of Hepaticopancreatic Diseases
The indications and preparation for laparoscopic liver surgery remain the same as in open hepatic surgery. Visualization is excellent with the laparoscope, and the addition of laparoscopic ultrasound has been shown to help intraoperative plans in 66 percent of cases when compared to laparoscopic exploration alone. The ability of visual inspection laparoscopy to assess resectability as opposed to inoperability remains relatively low. It can be improved by extended laparoscopy combined with laparoscopic contact ultrasonography. The technique of extended laparoscopy consists of a full inspection of the peritoneal cavity, liver with contact laparoscopic ultrasound scanning, entry and inspection of lesser sac, an examination of porta hepatis, duodenum, transverse mesocolon, and coeliac and portal vessels. This procedure thus entails extensive dissection and is used to assess operability in patients with pancreatic cancer, hepatic neoplasms, and gastroesophageal cancers where it often entails lymph node sampling. Laparoscopic hepatic surgery, while technically difficult, can be performed safely with good results with careful patient selection. Attention to the etiology of the lesion and its location is essential. Ideal candidates have a large solitary cyst or asymptomatic benign mass located superficially, laterally, or far enough from the pedicle to allow direct clamping of the liver or access to the hilum to perform a Pringle maneuver should bleeding occur.
Contraindications to this technique include patients with cirrhosis, hepatocellular carcinoma, or posterior or centrally located lesions. While we have utilized this approach for solitary small metastatic disease, hydatid disease, hepatic abscess, and polycystic liver disease (PCLD), these should be viewed with a great deal of circumspection. Problems exist to varying degrees should any of these lesions be spilled. Port site recurrences remain a concern when using laparoscopy in any patient with cancer. This is of special concern when considering pairing this approach with cryoablation. With echinococcal cysts, the risk of spillage is also obvious, though less problematic with calcified cysts. If one does use a laparoscopic approach for hydatid disease, we recommend a cholangiogram to rule out a connection with the biliary system. While fenestration of polycystic liver disease has been described both by open and laparoscopic approaches, transcystic fenestration of deeper cysts makes the control of bleeding difficult.
Laparoscopic liver surgery provides advantages over open surgery for the liver since the Chevron incision is completely avoided and the surgery is performed through tiny incisions. As a consequence, the duration of stay in the hospital, the amount and duration of postoperative discomfort, and the length of recovery are much shorter after the laparoscopic procedure compared to open surgery. To safely perform liver surgery laparoscopically, the surgeon must be both an accomplished laparoscopist and a hepatic surgeon. Few surgeons, however, are as comfortable with open hepatic surgery as they are with the gallbladder, hernia, appendix, or stomach. Furthermore, only a limited number of lesions, depending upon their location and etiology, can be approached by laparoscopy. The most commonly performed procedures are symptomatic solitary hepatic cyst, symptomatic polycystic liver disease, hydatid cyst, focal nodular hyperplasia, adenoma, abscess, metastatic breast cancer, and calcified gallbladder.
The technique of Laparoscopic Management of Hydatid Cystic Liver
The procedure is performed with the patient under general anesthesia with oro or nasogastric decompression and a pneumoperitoneum of 12 to 14 mm Hg.
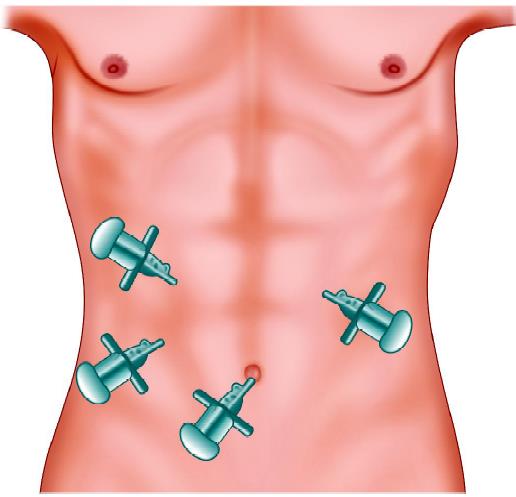
Port position of the hydatid cyst of the left lobe
The patients can be placed in the ‘‘French’’ position, modified lithotomy with minimal flexion of the hips, and the primary surgeon positioned between the legs. The first assistant stands on the patient’s left side and the scrub nurse between them. For fenestrations, use a four-trocar configuration. A 10 mm port at the umbilicus house the 30° telescope. A 5 mm trocar placed just below the xiphoid process to the right or the left of the falciform ligament, depending on the location of the cyst. This port is used to expose the liver, often using an irrigation aspiration probe. Two other 5 mm or 10 mm ports, in the right and left flank, allows the surgeon to puncture the cyst dome, aspirate its contents, and excise the cyst wall in a careful sequential fashion to facilitate hemostasis. For more extensive procedures, a strong light source (300 W xenon) and high- quality 30° scopes are required. To perform resections safely with a minimum of wasted motion, the four-hand technique is used by many surgeons. This uses four to six trocars and allows for the primary surgeon to expose and dissect the liver while the second surgeon obtains control and transects the blood vessels and bile ducts.
The procedure entails the same components as in open hepatic surgery. First, the patient is explored, both visually and ultrasonographically. Mobilization of the liver and hilar dissection are performed as necessary to obtain vascular control. Division and ligation of the round ligament followed by freeing of the falciform and the right or left triangular ligaments allow access to perform thorough exploration, dissection, and hemostasis. A gauge soaked with 3 percent saline is kept around the cyst to prevent contamination by spillage. A spiral needle is used to administer 10 percent saline inside the cyst. Dissection is begun by scoring Glisson’s capsule with the high-frequency electrosurgery. Parenchymal dissection can be performed using the ultrasonic dissector. After extraction, the germinal layer is placed in an impermeable specimen bag for removal. Cholangiography is very useful to detect possible bile leaks. The raw surface of the liver is then inspected, coagulated, and covered with fibrin glue. The specimen is extracted either by partial morcellation, dilatation at the umbilicus, enlarging another port site, or by a small McBurney or subcostal incision.

Gauge piece introduced soaked with 3% saline
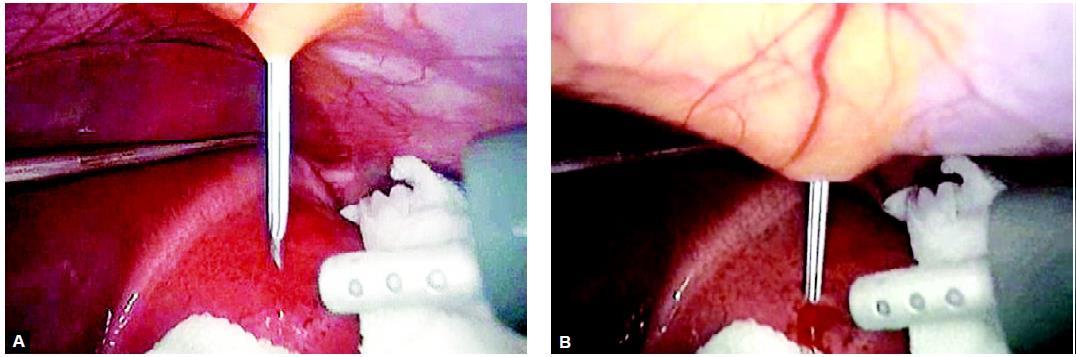
Instillation of hypertonic saline inside the cyst through a percutaneous spinal needle
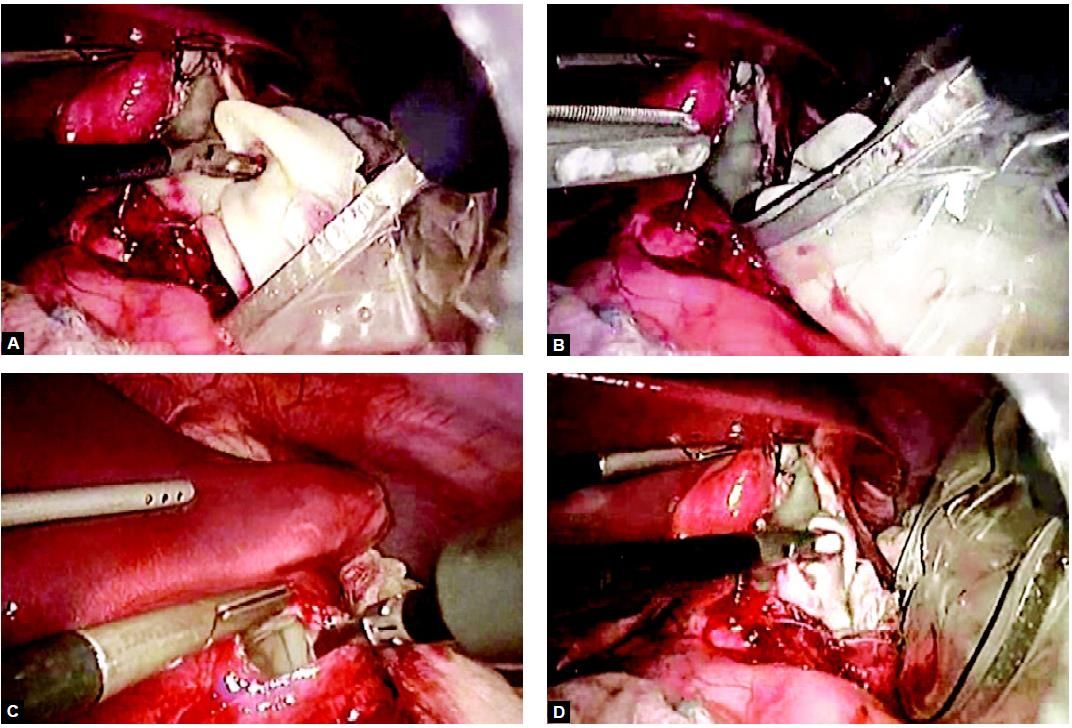
Opening of the cystic wall and extraction of the germinal layer

Removal of a cyst with the help of endobag
The indications and preparation for laparoscopic liver surgery remain the same as in open hepatic surgery. Visualization is excellent with the laparoscope, and the addition of laparoscopic ultrasound has been shown to help intraoperative plans in 66 percent of cases when compared to laparoscopic exploration alone. The ability of visual inspection laparoscopy to assess resectability as opposed to inoperability remains relatively low. It can be improved by extended laparoscopy combined with laparoscopic contact ultrasonography. The technique of extended laparoscopy consists of a full inspection of the peritoneal cavity, liver with contact laparoscopic ultrasound scanning, entry and inspection of lesser sac, an examination of porta hepatis, duodenum, transverse mesocolon, and coeliac and portal vessels. This procedure thus entails extensive dissection and is used to assess operability in patients with pancreatic cancer, hepatic neoplasms, and gastroesophageal cancers where it often entails lymph node sampling. Laparoscopic hepatic surgery, while technically difficult, can be performed safely with good results with careful patient selection. Attention to the etiology of the lesion and its location is essential. Ideal candidates have a large solitary cyst or asymptomatic benign mass located superficially, laterally, or far enough from the pedicle to allow direct clamping of the liver or access to the hilum to perform a Pringle maneuver should bleeding occur.
Contraindications to this technique include patients with cirrhosis, hepatocellular carcinoma, or posterior or centrally located lesions. While we have utilized this approach for solitary small metastatic disease, hydatid disease, hepatic abscess, and polycystic liver disease (PCLD), these should be viewed with a great deal of circumspection. Problems exist to varying degrees should any of these lesions be spilled. Port site recurrences remain a concern when using laparoscopy in any patient with cancer. This is of special concern when considering pairing this approach with cryoablation. With echinococcal cysts, the risk of spillage is also obvious, though less problematic with calcified cysts. If one does use a laparoscopic approach for hydatid disease, we recommend a cholangiogram to rule out a connection with the biliary system. While fenestration of polycystic liver disease has been described both by open and laparoscopic approaches, transcystic fenestration of deeper cysts makes the control of bleeding difficult.
Laparoscopic liver surgery provides advantages over open surgery for the liver since the Chevron incision is completely avoided and the surgery is performed through tiny incisions. As a consequence, the duration of stay in the hospital, the amount and duration of postoperative discomfort, and the length of recovery are much shorter after the laparoscopic procedure compared to open surgery. To safely perform liver surgery laparoscopically, the surgeon must be both an accomplished laparoscopist and a hepatic surgeon. Few surgeons, however, are as comfortable with open hepatic surgery as they are with the gallbladder, hernia, appendix, or stomach. Furthermore, only a limited number of lesions, depending upon their location and etiology, can be approached by laparoscopy. The most commonly performed procedures are symptomatic solitary hepatic cyst, symptomatic polycystic liver disease, hydatid cyst, focal nodular hyperplasia, adenoma, abscess, metastatic breast cancer, and calcified gallbladder.
The technique of Laparoscopic Management of Hydatid Cystic Liver
The procedure is performed with the patient under general anesthesia with oro or nasogastric decompression and a pneumoperitoneum of 12 to 14 mm Hg.
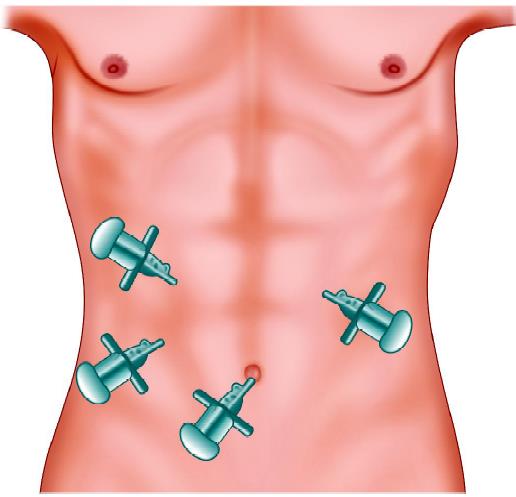
Port position of the hydatid cyst of the left lobe
The patients can be placed in the ‘‘French’’ position, modified lithotomy with minimal flexion of the hips, and the primary surgeon positioned between the legs. The first assistant stands on the patient’s left side and the scrub nurse between them. For fenestrations, use a four-trocar configuration. A 10 mm port at the umbilicus house the 30° telescope. A 5 mm trocar placed just below the xiphoid process to the right or the left of the falciform ligament, depending on the location of the cyst. This port is used to expose the liver, often using an irrigation aspiration probe. Two other 5 mm or 10 mm ports, in the right and left flank, allows the surgeon to puncture the cyst dome, aspirate its contents, and excise the cyst wall in a careful sequential fashion to facilitate hemostasis. For more extensive procedures, a strong light source (300 W xenon) and high- quality 30° scopes are required. To perform resections safely with a minimum of wasted motion, the four-hand technique is used by many surgeons. This uses four to six trocars and allows for the primary surgeon to expose and dissect the liver while the second surgeon obtains control and transects the blood vessels and bile ducts.
The procedure entails the same components as in open hepatic surgery. First, the patient is explored, both visually and ultrasonographically. Mobilization of the liver and hilar dissection are performed as necessary to obtain vascular control. Division and ligation of the round ligament followed by freeing of the falciform and the right or left triangular ligaments allow access to perform thorough exploration, dissection, and hemostasis. A gauge soaked with 3 percent saline is kept around the cyst to prevent contamination by spillage. A spiral needle is used to administer 10 percent saline inside the cyst. Dissection is begun by scoring Glisson’s capsule with the high-frequency electrosurgery. Parenchymal dissection can be performed using the ultrasonic dissector. After extraction, the germinal layer is placed in an impermeable specimen bag for removal. Cholangiography is very useful to detect possible bile leaks. The raw surface of the liver is then inspected, coagulated, and covered with fibrin glue. The specimen is extracted either by partial morcellation, dilatation at the umbilicus, enlarging another port site, or by a small McBurney or subcostal incision.

Gauge piece introduced soaked with 3% saline
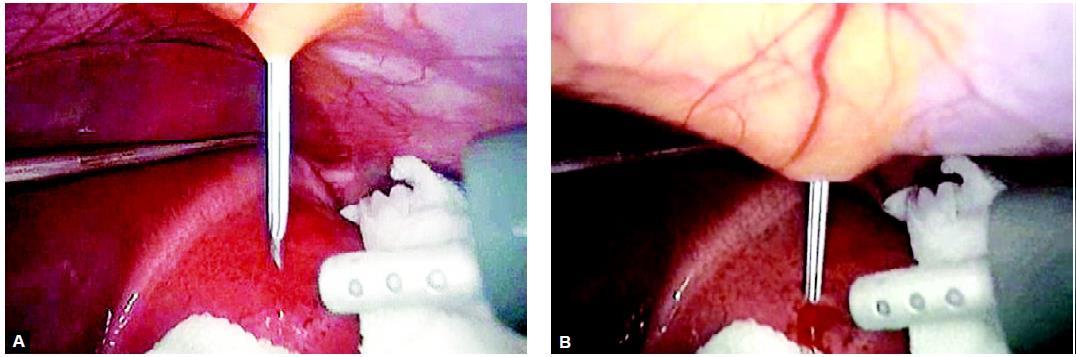
Instillation of hypertonic saline inside the cyst through a percutaneous spinal needle
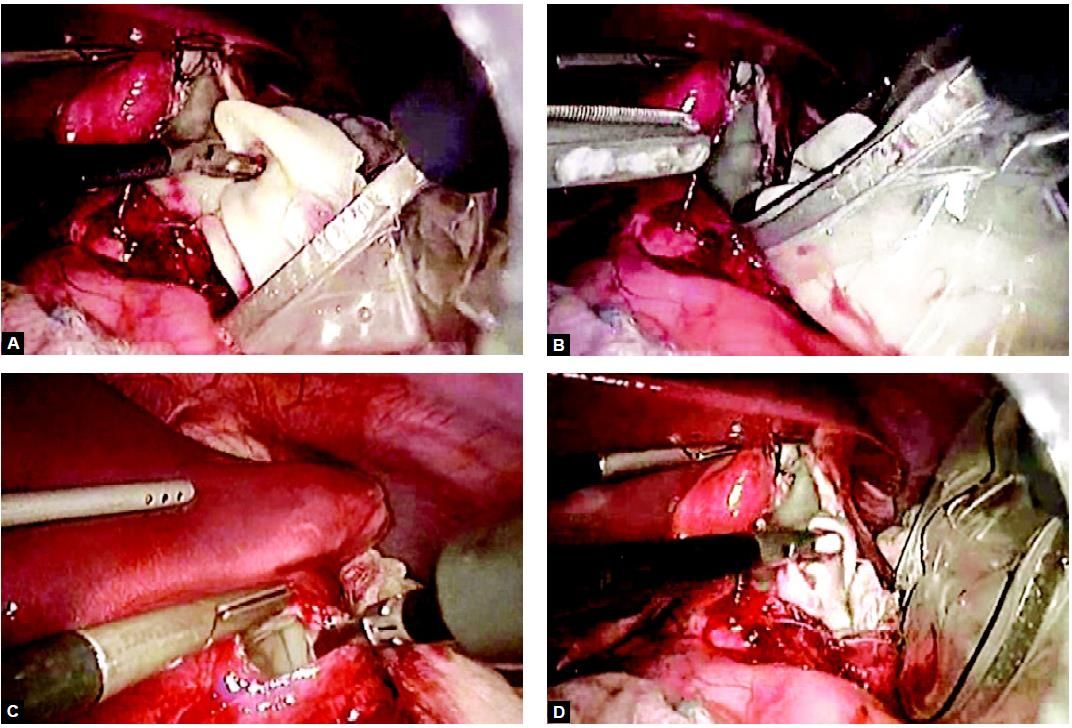
Opening of the cystic wall and extraction of the germinal layer

Removal of a cyst with the help of endobag


