Laparoscopic Management of Ectopic Pregnancy
Laparoscopy is one of the major advancements for the tubal and uterine disease. Surgical procedures for managing benign adnexal masses include aspiration, fenestration, ovarian cystectomy, unilateral or bilateral salpingo-oophorectomy, and laparoscopically-assisted vaginal hysterectomy (LAVH) with or without unilateral or bilateral salpingo-oophorectomy.
Ectopic Pregnancy
The risk of ectopic pregnancy is higher in white women. It increases three to four times in women between the age of 35 and 44 compared to those from 15 to 24. About 64 percent of ectopic pregnancies occur in the ampulla where fertilization occurs. The recent increase in the incidence of ectopic pregnancy has been attributed to a greater incidence of sexually transmitted disease, delayed childbearing, previous sexual organ surgical interference, and successful clinical detection. Any condition that prevents or retards the migration of fertilized ovum to the uterine cavity could predispose a woman to an ectopic gestation.
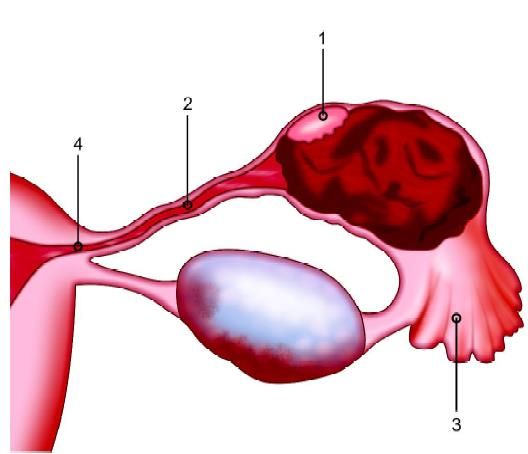
Tubal pregnancy: (1) The ampulla; (2) The isthmus (3) The infundibulum; (4) The intramural junctions
Ectopic pregnancy usually occurs 99 percent of cases in the uterine tube. It can be found in:
• The ampulla (64%)
• The isthmus (25%)
• The infundibulum (9%)
• The intramural junction (2%)
• Ovarian (0.5%)
• Cervical (0.4%)
• Abdominal (0.1%)
• Intraligamental (0.05%).
Major contributing factors and associated relative risks for ectopic pregnancy are:
• Current use of an intrauterine device (11.5%)
• Use of clomiphene citrate (10%)
• Prior tubal surgery (5.6%)
• Pelvic inflammatory disease (4.0%)
• Infertility (2.9%)
• Induced abortion (2.5%)
• Adhesions (2.4%)
• Abdominal surgery (2.3%)
• T-shaped uterus (2%)
• Myoma (1.7%)
• Progestin-only contraceptives (1.6%).
If laparoscopy is planned, the location, the size, and the nature of the tubal pregnancy are ascertained. If the bleeding has ceased or can be arrested adequately, rupture tubal pregnancies can be treated successfully endoscopically. Once bleeding is controlled, the products of conception and blood clots are removed. If there is more than 1,500 cc hemoperitoneum, the laparoscopic approach is contraindicated. Heparinized saline should be used in cases of a large hematoma. Large ruptured ectopic requires extracorporeal knotting.
A 10 mm suction instrument is used to clean the abdominal cavity. Forced irrigation with normal saline should dislodge the clot and trophoblastic tissue from the serosa of the peritoneal organs with minimal injury to these structures.
For unruptured tubal pregnancy, the fallopian tubes are identified and mobilized to minimize bleeding, a 5 to 8 ml diluted solution containing five-unit vasopressin in 20 ml of saline is injected with a 20 gauge spinal or laparoscopic needle. It should be injected in the mesosalpinx just below the ectopic and over the antimesenteric surface of the tubal segment containing gestational products. The needle must not be inserted deep within a blood vessel because intravascular injection may precipitate acute arterial hypertension, bradycardia, and sometime it may be fatal.
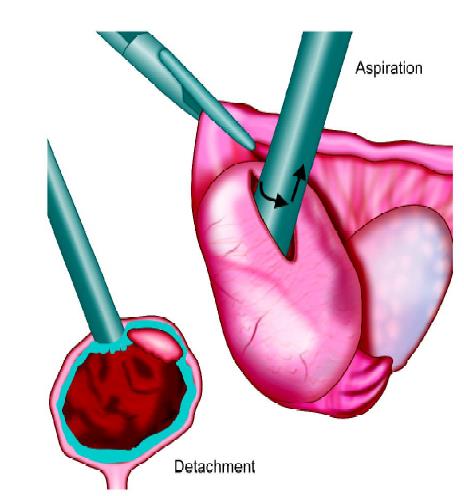
The suction of trophoblast for unruptured ectopic pregnancy
After stabilizing the tube by grasper in one hand and microelectrode in another, a linear incision is made on the antimesenteric surface extending one to two centimeters over the thinnest portion of the tube. The fine needle tip should be used in the cutting mode, and should barely touch the tissue surface. With electrosurgery, thermal damage may spread if large tips are used on large surface areas in contact with tissue. It is important to remain aware of the location of underlying or adjacent structures. If the gynecologists are not careful there may be a chance of adjacent visceral injury. The pregnancy usually should protrude through the incision and slowly slips out of the tube. It may be teased gently out using hydrodissection or laparoscopic atraumatic forceps. Sometimes forceful irrigation in the tubal opening can dislodge the gestation from implantation. As pregnancy is pulled out or extrudes from the tube, some of the product of conception can adhere to the implantation site by a ligamentous structure containing blood vessels. Using bipolar this structure should be coagulated before removing the tissue. Depending upon the size of the product of conception, ectopic is removed usually through a 10 mm trocar sleeve.
Resection of the tubal segment containing the gestation is preferable to salpingostomy for an isthmic pregnancy or a ruptured tube or if hemostasis is difficult to obtain. Segmental tubal resection is performed by the help of bipolar forceps or harmonic scalpel. Automatic stapling or suturing devices can be used for bloodless tubal resection. If the mesosalpinx bleeds, it should be cauterized by using bipolar forceps, particular attention given to the arcuate anastomosing branches of the ovarian and uterine arteries. Total salpingectomy is performed by progressively coagulating and cutting the mesosalpinx, beginning with the proximal portion to the fimbrial end. It is separated from the uterus using bipolar coagulation and scissors. The isolated segment containing the tubal pregnancy is removed intact or in sectioned part, through the 10 mm trocar sleeve. The product of conception can be placed in a plastic bag and removed. Multi fire stapling devices for salpingectomy require a 10 mm trocar. If the tissue is bulky and can not be accommodated through a cannula, endobag can be used for retrieval of tissue. Adhesion or other pathologic processes such as endometriosis can be treated simultaneously during the removal of ectopic pregnancy without significantly prolonging the operation. In one week the beta hCG should return to baseline, i.e. undetectable or very low.

Salpingectomy
If the pregnancy is interstitial it may be associated with traumatic rupture, hemorrhagic shock and there is a two-fold increase in maternal mortality over other tubal pregnancies. Delayed diagnosis and increased vascularity of this make the laparoscopic procedure difficult. Two to four percent of ectopic is interstitial. The anatomy of ectopic accommodates the growing gestation, accounting for its late recognition. Traditional management is better in these cases, i.e. salpingectomy with or without corneal resection, and in some difficult cases, hysterectomy may be necessary. Interstitial pregnancy can be suspected at the time of laparoscopy when the large and asymmetrical uterus is seen. Most patients are discharged within 48 hours. There is a higher fertility rate/intrauterine pregnancy rate in subsequent pregnancies with laparoscopic techniques.
Laparoscopic surgery is a good option for rupture ectopic and ruptured ectopic does not necessarily warrant a laparotomy. If the patient is hemodynamically stable and the initial laparoscopic examination indicates a moderate blood loss, it may be possible to control bleeding laparoscopically and perform any indicated procedures. If the patient is in stage II or stages III shock who has a large hemoperitoneum, laparotomy is the better choice. Managing ruptured ectopic pregnancies involves examining the pelvis, localizing the ectopic, aspirating blood and clots, localizing and controlling the bleeding points, and performing either salpingectomy or in rare situations, oophorectomy is performed concurrently.
Controlling bleeding is the most critical part of the procedure, and several methods can be attempted sequentially to achieve hemostasis:
• Identification of the bleeding point followed by careful bipolar electrodesiccation.
• Injection of vasopressin over the mesosalpinx.
• Electrodesiccation of the mesosalpinx.
• If bleeding does not stop by these means the partial or complete salpingectomy, depending on the portion of the tube involved and the patient’s desire for fertility.
After successfully managing the ectopic pregnancy laparoscopically, the patient can be discharged the second day. The patient should come again for a serum ft-hCG one week postoperatively to ascertain the resolution of the ectopic gestation. The ft-hCG level should be either undetectable or very low after one week of surgery. If it is above 20 mIU/ mL, a repeat blood test is ordered one to 2 weeks later when the ft-hCG should be undetectable.
Laparoscopy is one of the major advancements for the tubal and uterine disease. Surgical procedures for managing benign adnexal masses include aspiration, fenestration, ovarian cystectomy, unilateral or bilateral salpingo-oophorectomy, and laparoscopically-assisted vaginal hysterectomy (LAVH) with or without unilateral or bilateral salpingo-oophorectomy.
Ectopic Pregnancy
The risk of ectopic pregnancy is higher in white women. It increases three to four times in women between the age of 35 and 44 compared to those from 15 to 24. About 64 percent of ectopic pregnancies occur in the ampulla where fertilization occurs. The recent increase in the incidence of ectopic pregnancy has been attributed to a greater incidence of sexually transmitted disease, delayed childbearing, previous sexual organ surgical interference, and successful clinical detection. Any condition that prevents or retards the migration of fertilized ovum to the uterine cavity could predispose a woman to an ectopic gestation.
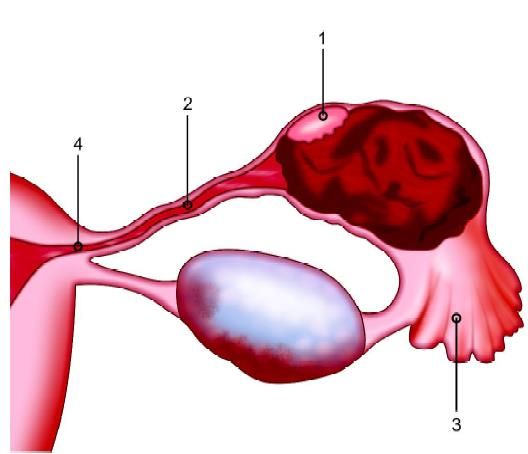
Tubal pregnancy: (1) The ampulla; (2) The isthmus (3) The infundibulum; (4) The intramural junctions
Ectopic pregnancy usually occurs 99 percent of cases in the uterine tube. It can be found in:
• The ampulla (64%)
• The isthmus (25%)
• The infundibulum (9%)
• The intramural junction (2%)
• Ovarian (0.5%)
• Cervical (0.4%)
• Abdominal (0.1%)
• Intraligamental (0.05%).
Major contributing factors and associated relative risks for ectopic pregnancy are:
• Current use of an intrauterine device (11.5%)
• Use of clomiphene citrate (10%)
• Prior tubal surgery (5.6%)
• Pelvic inflammatory disease (4.0%)
• Infertility (2.9%)
• Induced abortion (2.5%)
• Adhesions (2.4%)
• Abdominal surgery (2.3%)
• T-shaped uterus (2%)
• Myoma (1.7%)
• Progestin-only contraceptives (1.6%).
If laparoscopy is planned, the location, the size, and the nature of the tubal pregnancy are ascertained. If the bleeding has ceased or can be arrested adequately, rupture tubal pregnancies can be treated successfully endoscopically. Once bleeding is controlled, the products of conception and blood clots are removed. If there is more than 1,500 cc hemoperitoneum, the laparoscopic approach is contraindicated. Heparinized saline should be used in cases of a large hematoma. Large ruptured ectopic requires extracorporeal knotting.
A 10 mm suction instrument is used to clean the abdominal cavity. Forced irrigation with normal saline should dislodge the clot and trophoblastic tissue from the serosa of the peritoneal organs with minimal injury to these structures.
For unruptured tubal pregnancy, the fallopian tubes are identified and mobilized to minimize bleeding, a 5 to 8 ml diluted solution containing five-unit vasopressin in 20 ml of saline is injected with a 20 gauge spinal or laparoscopic needle. It should be injected in the mesosalpinx just below the ectopic and over the antimesenteric surface of the tubal segment containing gestational products. The needle must not be inserted deep within a blood vessel because intravascular injection may precipitate acute arterial hypertension, bradycardia, and sometime it may be fatal.
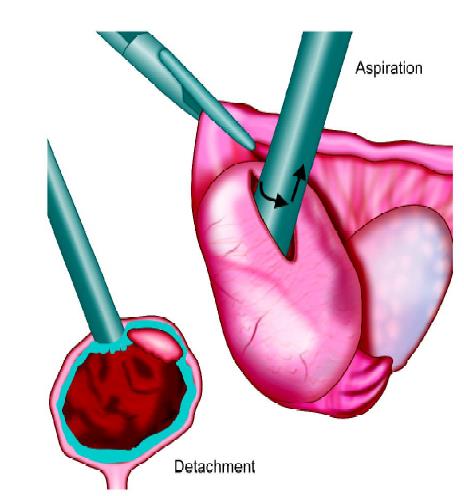
The suction of trophoblast for unruptured ectopic pregnancy
After stabilizing the tube by grasper in one hand and microelectrode in another, a linear incision is made on the antimesenteric surface extending one to two centimeters over the thinnest portion of the tube. The fine needle tip should be used in the cutting mode, and should barely touch the tissue surface. With electrosurgery, thermal damage may spread if large tips are used on large surface areas in contact with tissue. It is important to remain aware of the location of underlying or adjacent structures. If the gynecologists are not careful there may be a chance of adjacent visceral injury. The pregnancy usually should protrude through the incision and slowly slips out of the tube. It may be teased gently out using hydrodissection or laparoscopic atraumatic forceps. Sometimes forceful irrigation in the tubal opening can dislodge the gestation from implantation. As pregnancy is pulled out or extrudes from the tube, some of the product of conception can adhere to the implantation site by a ligamentous structure containing blood vessels. Using bipolar this structure should be coagulated before removing the tissue. Depending upon the size of the product of conception, ectopic is removed usually through a 10 mm trocar sleeve.
Resection of the tubal segment containing the gestation is preferable to salpingostomy for an isthmic pregnancy or a ruptured tube or if hemostasis is difficult to obtain. Segmental tubal resection is performed by the help of bipolar forceps or harmonic scalpel. Automatic stapling or suturing devices can be used for bloodless tubal resection. If the mesosalpinx bleeds, it should be cauterized by using bipolar forceps, particular attention given to the arcuate anastomosing branches of the ovarian and uterine arteries. Total salpingectomy is performed by progressively coagulating and cutting the mesosalpinx, beginning with the proximal portion to the fimbrial end. It is separated from the uterus using bipolar coagulation and scissors. The isolated segment containing the tubal pregnancy is removed intact or in sectioned part, through the 10 mm trocar sleeve. The product of conception can be placed in a plastic bag and removed. Multi fire stapling devices for salpingectomy require a 10 mm trocar. If the tissue is bulky and can not be accommodated through a cannula, endobag can be used for retrieval of tissue. Adhesion or other pathologic processes such as endometriosis can be treated simultaneously during the removal of ectopic pregnancy without significantly prolonging the operation. In one week the beta hCG should return to baseline, i.e. undetectable or very low.

Salpingectomy
If the pregnancy is interstitial it may be associated with traumatic rupture, hemorrhagic shock and there is a two-fold increase in maternal mortality over other tubal pregnancies. Delayed diagnosis and increased vascularity of this make the laparoscopic procedure difficult. Two to four percent of ectopic is interstitial. The anatomy of ectopic accommodates the growing gestation, accounting for its late recognition. Traditional management is better in these cases, i.e. salpingectomy with or without corneal resection, and in some difficult cases, hysterectomy may be necessary. Interstitial pregnancy can be suspected at the time of laparoscopy when the large and asymmetrical uterus is seen. Most patients are discharged within 48 hours. There is a higher fertility rate/intrauterine pregnancy rate in subsequent pregnancies with laparoscopic techniques.
Laparoscopic surgery is a good option for rupture ectopic and ruptured ectopic does not necessarily warrant a laparotomy. If the patient is hemodynamically stable and the initial laparoscopic examination indicates a moderate blood loss, it may be possible to control bleeding laparoscopically and perform any indicated procedures. If the patient is in stage II or stages III shock who has a large hemoperitoneum, laparotomy is the better choice. Managing ruptured ectopic pregnancies involves examining the pelvis, localizing the ectopic, aspirating blood and clots, localizing and controlling the bleeding points, and performing either salpingectomy or in rare situations, oophorectomy is performed concurrently.
Controlling bleeding is the most critical part of the procedure, and several methods can be attempted sequentially to achieve hemostasis:
• Identification of the bleeding point followed by careful bipolar electrodesiccation.
• Injection of vasopressin over the mesosalpinx.
• Electrodesiccation of the mesosalpinx.
• If bleeding does not stop by these means the partial or complete salpingectomy, depending on the portion of the tube involved and the patient’s desire for fertility.
After successfully managing the ectopic pregnancy laparoscopically, the patient can be discharged the second day. The patient should come again for a serum ft-hCG one week postoperatively to ascertain the resolution of the ectopic gestation. The ft-hCG level should be either undetectable or very low after one week of surgery. If it is above 20 mIU/ mL, a repeat blood test is ordered one to 2 weeks later when the ft-hCG should be undetectable.





