Laparoscopic Low Anterior Resection
Two surgical procedures with curative intent are available to patients with rectal cancer:
1. Lower anterior resection and
2. Abdominoperineal resection
Lower anterior resection may improve quality of life and functional status. Lower anterior resection, formally known as anterior resection of the rectum and anterior excision of the rectum or simply anterior resection is a common surgery for rectal cancer. It is commonly abbreviated as LAR. LAR is generally the preferred treatment for rectal cancer insofar as this is surgically feasible. Laparoscopic low anterior resection for rectal cancer has gained wide acceptance among general surgeons. HALS LAR is also having equal acceptance mainly due to the technical difficulties encountered during pelvic dissection.
Patient Positioning
The patient is placed supine on the operating table. After induction of general anesthesia and insertion of an orogastric tube and Foley catheter, the legs are placed in stirrups. The arms are tucked at the patient's side and the beanbag is aspirated. The abdomen is prepared with an antiseptic solution and draped routinely.

Patient position for low anterior resection
Position of Surgical Team
The primary monitor is placed on the left side of the patient at approximately the level of the hip. The operating nurse is placed between the patient's legs. There should be sufficient space to allow the surgeon to move from either side of the patient to between the patient's legs, if necessary. The primary operating surgeon stands on the right side of the patient with the assistant standing on the patient's left and moving to the right side, caudad to the surgeon, once ports have been inserted. A 30-degree telescope is used.
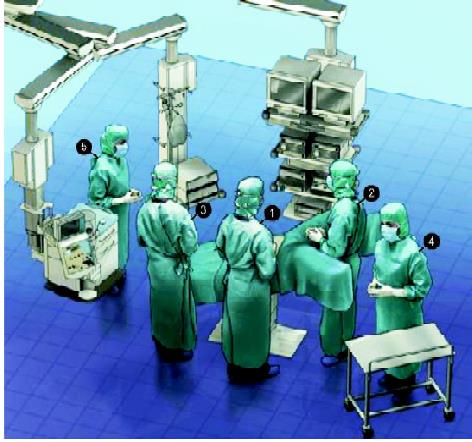
Position of the surgical team for LAR
Port Position
The primary optical port is introduced sub umbilical using a modified Hasson approach. Having confirmed entry into the peritoneal cavity, a purse-string suture is placed around the sub umbilical fascial defect. The abdomen to be insufflated with CO2 to a pressure of 12 mm Hg. The telescope is inserted into the abdomen and an initial diagnostic laparoscopy is performed, carefully evaluating the liver, small bowel, and peritoneal surfaces. A 12 mm port is inserted in the right lower quadrant approximately 2 to 3 cm medial and superior to the anterior superior iliac spine. It is carefully inserted lateral to the inferior epigastric vessels, paying attention to keep the tract of the port going as perpendicular as possible through the abdominal wall. A 5 mm port is then inserted in the right upper quadrant at least a hand's breadth superior to the lower quadrant port. A left lower quadrant 5 mm port is inserted. A 5 mm left upper quadrant port is also inserted to aid splenic flexure mobilization. Again, all of these remaining ports are kept lateral to the epigastric vessels. This may be ensured by diligence to anatomic port site selection and using the laparoscope to transilluminate the abdominal wall before making the port site incision to identify any obvious superficial vessels.
The assistant now moves to the patient's left side, standing caudad to the surgeon. The patient is rotated with the left side up and right side down, to approximately 15 to 20 degrees tilt, and often as far as the table can go. This helps to move the small bowel over to the right side of the abdomen. The patient is then placed in the Trendelenburg position. This again helps gravitational migration of the small bowel away from the operative field. The surgeon then inserts two atraumatic bowel clamps through the two right-sided abdominal ports. The greater omentum is reflected over the transverse colon so that it comes to lie on the stomach. If there is no space in the upper part of the abdomen, one must confirm that the orogastric tube is adequately decompressing the stomach. The small bowel is moved to the patient's right side allowing visualization of the medial aspect of the rectosigmoid mesentery. This may necessitate the use of the assistant's 5 mm atraumatic bowel clamp through the left lower quadrant to tent the sigmoid mesentery cephalad.
Defining and Dividing the Inferior Mesenteric Pedicle
An atraumatic bowel clamp is placed on the rectosigmoid mesentery at the level of the sacral promontory, approximately halfway between the bowel wall and the promontory itself. This area is then stretched up toward the left lower quadrant port, stretching the inferior mesenteric vessels away from the retroperitoneum. In most cases, this demonstrates a groove between the right or medial side of the inferior mesenteric pedicle and the retroperitoneum. Electro-surgery or harmonic is used to open the peritoneum along this line, opening the plane cranially up to the origin of the inferior mesenteric artery, and caudally up to the sacral promontory. Blunt dissection is then used to lift the vessels away from the retroperitoneum and presacral autonomic nerves. The ureter is then looked for under the inferior mesenteric artery. If the ureter cannot be seen, and the dissection is in the correct plane, the ureter should be just deep to the parietal peritoneum, and just medial to the gonadal vessels. Care must be taken not to dissect too deep and injure the iliac vessels.
If the ureter cannot be found, it has usually been elevated on the back of the inferior mesenteric pedicle, and one needs to stay very close to the vessel not only to find the ureter but also to protect the autonomic nerves. If the ureter still cannot be found, the dissection needs to come in a cranial direction, which is usually into clean tissue allowing it to be found. If this fails, a lateral approach can be performed. This usually gives a fresh perspective to the tissues, and the ureter can often be found quite easily. In very rare cases, the ureter still may not be found. The ureteric stent should be used and it helps in easy identification of ureter and prevents it to get injured. It is good not to proceed if the ureter cannot be defined. The dissection is continued up to the origin of the inferior mesenteric artery, which is carefully defined and divided using a high ligation, above the left colic artery. A clamp is placed on the origin of the vessel to control it if clips or other energy sources do not adequately control the vessel. Endogia stapler can also be used for easy division of the vessel.
Having divided the vessels at the origin of the artery, the plane between the descending colon mesentery and the retroperitoneum is developed laterally, out toward the lateral attachment of the colon, and superiorly, dissecting the bowel off the anterior surface of the Gerota's fascia up toward the splenic flexure. This makes the inferior vein quite obvious and this vessel can also be divided just inferior to the pancreas. This allows increased reach for a coloanal anastomosis with or without neorectal reservoir.
Mobilization of the Lateral Attachments of the Rectosigmoid and Descending Colon
The surgeon now grasps the rectosigmoid junction with his left-hand instrument and draws it to the patient's right side. This allows the lateral attachments of the sigmoid colon to be seen and divided using electrosurgery or harmonic. Bruising from the prior retroperitoneal mobilization of the colon can usually be seen in this area. Once this layer of peritoneum has been opened, one immediately enters into the space opened by the retroperitoneal dissection. Dissection now continues up along the white line of Toldt, toward the splenic flexure. As the dissection continues, the surgeon's left-hand instrument needs to be gradually moved up along the descending colon to keep the lateral attachments under tension. In this way, the lateral and any remaining posterior attachments are free, making the left colon and sigmoid a midline structure. Elevating the descending colon and drawing it medially is useful, as this keeps small bowel loops out of the way of the dissecting instrument and facilitates the dissection. In some patients, particularly very obese or otherwise large patients, it is difficult to reach high enough through the right lower quadrant port. For this reason, the surgeon's right-hand instrument is moved to the left lower quadrant port site. This permits greater reach along the descending colon.
Mobilization of the Splenic Flexure
Complete lateral mobilization of the left colon up to the splenic flexure is performed as an initial step. The descending colon is pulled medially using an atraumatic bowel clamp in the right lower quadrant port and the scissors are placed in the left iliac fossa port. A 5 mm left upper quadrant port may be necessary, particularly in those with a very high splenic flexure, or in very tall or obese individuals. The lateral attachments of the left colon are divided and the colon is dissected off the Gerota's fascia over the left kidney.
Once the lateral attachments of the colon have been freed, it is necessary to move medially and enter the lesser sac. Some surgeons prefer to perform this as an initial step before lateral mobilization. To enter the lesser sac, the patient is tilted to a slight reverse Trendelenburg position. An atraumatic bowel clamp is inserted through the right upper quadrant port. If the left upper quadrant port is available this is also used. The assistant holds up the greater omentum, toward its left side, like a cape. The surgeon grasps the transverse colon toward the left side using a grasper in the right lower quadrant port to aid the identification of the avascular plane between the greater omentum and the transverse mesocolon. Harmonic scalpel or monopolar scissors can be used through the left lower quadrant port to dissect this plane and enter the lesser sac. The surgeon usually moves to stand between the patient's legs for this part of the procedure. This dissection is continued toward the splenic flexure. Following separation of the omentum off the left side of the transverse colon, connection to the lateral dissection allows the splenic flexure to be fully mobilized. The colon at the flexure is retracted caudally and medially, and any remaining restraining attachments are divided.
Rectal Mobilization
The patient is returned to the Trendelenburg position, and the small bowel is reflected cranially. Atraumatic bowel clamps inserted through the left-sided ports are used to elevate the rectosigmoid colon out of the pelvis and away from the retroperitoneum and sacral promontory, to enable entry into the presacral space. The posterior aspect of the mesorectum can be identified and the mesorectal plane dissected with diathermy, preserving the hypogastric nerves as they pass down into the pelvis, anterior to the sacrum. Dissection continues down the presacral space in this avascular plane toward the pelvic floor.
Attention is now switched to the peritoneum on the right side of the rectum. This is divided into the level of the seminal vesicles or rectovaginal septum. This is repeated on the peritoneum on the left side of the rectum. This facilitates further posterior dissection along the back of the mesorectum to the pelvic floor, to a level inferior to the lower edge of the mesorectum, just posterior to the anal canal. For a low anterior resection, it is necessary to perform a total mesorectal excision and hence the rectum must be dissected down to the muscle tube of the rectum below the inferior extent of the mesorectum. In many cases, particularly in those who are obese or men with a narrow pelvis, some or all of the anterior and lateral dissection must be completed to get adequate visualization, to complete the posterior dissection.
An atraumatic bowel clamp through the left iliac fossa port is used to retract the peritoneum anterior to the rectum forward. The peritoneal dissection is continued from the free edge of the lateral peritoneal dissection, anteriorly. Lateral dissection is continued on both sides of the rectum and is extended anterior to the rectum, posterior to Denonvillier's fascia, separating the posterior vaginal wall from the anterior wall of the rectum or down to the level of the prostate in men. The difficulty of dissection will vary depending on the body habitus of the patient, the diameter of the pelvis, and the size of the tumor. Occasionally, rectal mobilization can be very difficult to perform laparoscopically. In some cases, it may need to be completed in an open manner through a small Pfannenstiel incision.
Division of Rectum
The lower rectum may be divided with a stapler either laparoscopically or by open surgery, depending on the ease of access related to the size of the pelvis. A rotaculator laparoscopic stapler may be used to divide the muscle tube of the rectum below the level of the mesorectum. The stapler is inserted through the right lower quadrant incision, and two firings of the stapler are usually required to divide the rectum. There is no residual mesorectum to divide at this level. A digital examination is performed to confirm the location of the distal staple line, and if there is any doubt about the adequacy of the distal margin, a rigid proctoscopy is performed.
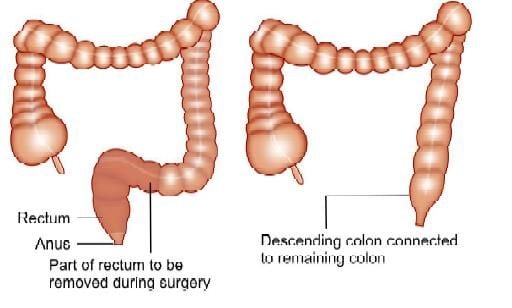
Low anterior resection
It is sometimes impossible to divide the rectum laparoscopically as the angulation of the endovascular stapler is limited to 45 degrees, necessitating the open division of the rectum. In some patients, getting an assistant to push up on the perineum with their hand may lift the pelvic floor enough to get the first cartridge of the stapler low enough. In some cases, placing a suprapubic port allows easier access with the stapler to allow the division of the rectum. Some patients are either too obese or have a very narrow pelvis or a long anal canal, and the stapler cannot be passed low enough. Two options exist. One is to perform a transanal intersphincteric dissection, remove the specimen, and then perform a handsewn coloanal anastomosis. The second is to perform a short Pfannenstiel incision, which allows a linear 30 mm stapler to be positioned and the rectum divided.
Extraction and Anastomosis
The specimen can be extracted either through a Pfannenstiel incision or a left iliac fossa incision; in both incisions, a wound protector is used in cases with a polyp or cancer to reduce the risk of tumor implantation in the wound. The left colon mesentery is divided with cautery. The left colon is divided and the specimen is removed. Pulsatile mesenteric bleeding is confirmed and the vessels ligated with 0 polyglycolate suture ties. Depending on the preference of the operating surgeon, a colonic pouch or coloplasty may be performed. A 2/0 Prolene purse-string suture is inserted into the distal end of the left colon or pouch, the anvil of a circular stapling gun inserted, and the purse-string suture is tied tightly. If a Pfannenstiel incision has been made, the coloanal anastomosis can be performed under direct vision and open manipulation following the insertion of a circular stapling gun into the rectal stump. If a left iliac fossa incision has been used, the colon is returned to the abdomen and the incision closed, the pneumoperitoneum recreated, and the anastomosis is formed laparoscopically. The anastomosis can be leak-tested by filling the pelvis with saline and inflating the neorectum using a proctoscope or bulb syringe.
Two surgical procedures with curative intent are available to patients with rectal cancer:
1. Lower anterior resection and
2. Abdominoperineal resection
Lower anterior resection may improve quality of life and functional status. Lower anterior resection, formally known as anterior resection of the rectum and anterior excision of the rectum or simply anterior resection is a common surgery for rectal cancer. It is commonly abbreviated as LAR. LAR is generally the preferred treatment for rectal cancer insofar as this is surgically feasible. Laparoscopic low anterior resection for rectal cancer has gained wide acceptance among general surgeons. HALS LAR is also having equal acceptance mainly due to the technical difficulties encountered during pelvic dissection.
Patient Positioning
The patient is placed supine on the operating table. After induction of general anesthesia and insertion of an orogastric tube and Foley catheter, the legs are placed in stirrups. The arms are tucked at the patient's side and the beanbag is aspirated. The abdomen is prepared with an antiseptic solution and draped routinely.

Patient position for low anterior resection
Position of Surgical Team
The primary monitor is placed on the left side of the patient at approximately the level of the hip. The operating nurse is placed between the patient's legs. There should be sufficient space to allow the surgeon to move from either side of the patient to between the patient's legs, if necessary. The primary operating surgeon stands on the right side of the patient with the assistant standing on the patient's left and moving to the right side, caudad to the surgeon, once ports have been inserted. A 30-degree telescope is used.
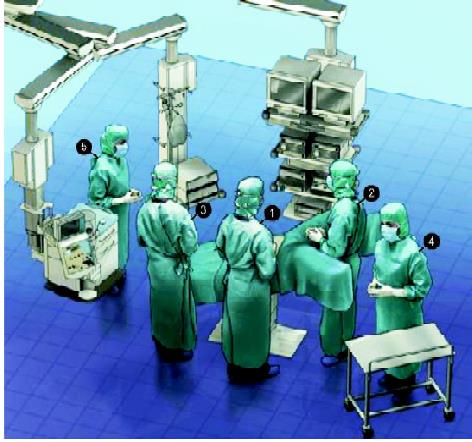
Position of the surgical team for LAR
Port Position
The primary optical port is introduced sub umbilical using a modified Hasson approach. Having confirmed entry into the peritoneal cavity, a purse-string suture is placed around the sub umbilical fascial defect. The abdomen to be insufflated with CO2 to a pressure of 12 mm Hg. The telescope is inserted into the abdomen and an initial diagnostic laparoscopy is performed, carefully evaluating the liver, small bowel, and peritoneal surfaces. A 12 mm port is inserted in the right lower quadrant approximately 2 to 3 cm medial and superior to the anterior superior iliac spine. It is carefully inserted lateral to the inferior epigastric vessels, paying attention to keep the tract of the port going as perpendicular as possible through the abdominal wall. A 5 mm port is then inserted in the right upper quadrant at least a hand's breadth superior to the lower quadrant port. A left lower quadrant 5 mm port is inserted. A 5 mm left upper quadrant port is also inserted to aid splenic flexure mobilization. Again, all of these remaining ports are kept lateral to the epigastric vessels. This may be ensured by diligence to anatomic port site selection and using the laparoscope to transilluminate the abdominal wall before making the port site incision to identify any obvious superficial vessels.
The assistant now moves to the patient's left side, standing caudad to the surgeon. The patient is rotated with the left side up and right side down, to approximately 15 to 20 degrees tilt, and often as far as the table can go. This helps to move the small bowel over to the right side of the abdomen. The patient is then placed in the Trendelenburg position. This again helps gravitational migration of the small bowel away from the operative field. The surgeon then inserts two atraumatic bowel clamps through the two right-sided abdominal ports. The greater omentum is reflected over the transverse colon so that it comes to lie on the stomach. If there is no space in the upper part of the abdomen, one must confirm that the orogastric tube is adequately decompressing the stomach. The small bowel is moved to the patient's right side allowing visualization of the medial aspect of the rectosigmoid mesentery. This may necessitate the use of the assistant's 5 mm atraumatic bowel clamp through the left lower quadrant to tent the sigmoid mesentery cephalad.
Defining and Dividing the Inferior Mesenteric Pedicle
An atraumatic bowel clamp is placed on the rectosigmoid mesentery at the level of the sacral promontory, approximately halfway between the bowel wall and the promontory itself. This area is then stretched up toward the left lower quadrant port, stretching the inferior mesenteric vessels away from the retroperitoneum. In most cases, this demonstrates a groove between the right or medial side of the inferior mesenteric pedicle and the retroperitoneum. Electro-surgery or harmonic is used to open the peritoneum along this line, opening the plane cranially up to the origin of the inferior mesenteric artery, and caudally up to the sacral promontory. Blunt dissection is then used to lift the vessels away from the retroperitoneum and presacral autonomic nerves. The ureter is then looked for under the inferior mesenteric artery. If the ureter cannot be seen, and the dissection is in the correct plane, the ureter should be just deep to the parietal peritoneum, and just medial to the gonadal vessels. Care must be taken not to dissect too deep and injure the iliac vessels.
If the ureter cannot be found, it has usually been elevated on the back of the inferior mesenteric pedicle, and one needs to stay very close to the vessel not only to find the ureter but also to protect the autonomic nerves. If the ureter still cannot be found, the dissection needs to come in a cranial direction, which is usually into clean tissue allowing it to be found. If this fails, a lateral approach can be performed. This usually gives a fresh perspective to the tissues, and the ureter can often be found quite easily. In very rare cases, the ureter still may not be found. The ureteric stent should be used and it helps in easy identification of ureter and prevents it to get injured. It is good not to proceed if the ureter cannot be defined. The dissection is continued up to the origin of the inferior mesenteric artery, which is carefully defined and divided using a high ligation, above the left colic artery. A clamp is placed on the origin of the vessel to control it if clips or other energy sources do not adequately control the vessel. Endogia stapler can also be used for easy division of the vessel.
Having divided the vessels at the origin of the artery, the plane between the descending colon mesentery and the retroperitoneum is developed laterally, out toward the lateral attachment of the colon, and superiorly, dissecting the bowel off the anterior surface of the Gerota's fascia up toward the splenic flexure. This makes the inferior vein quite obvious and this vessel can also be divided just inferior to the pancreas. This allows increased reach for a coloanal anastomosis with or without neorectal reservoir.
Mobilization of the Lateral Attachments of the Rectosigmoid and Descending Colon
The surgeon now grasps the rectosigmoid junction with his left-hand instrument and draws it to the patient's right side. This allows the lateral attachments of the sigmoid colon to be seen and divided using electrosurgery or harmonic. Bruising from the prior retroperitoneal mobilization of the colon can usually be seen in this area. Once this layer of peritoneum has been opened, one immediately enters into the space opened by the retroperitoneal dissection. Dissection now continues up along the white line of Toldt, toward the splenic flexure. As the dissection continues, the surgeon's left-hand instrument needs to be gradually moved up along the descending colon to keep the lateral attachments under tension. In this way, the lateral and any remaining posterior attachments are free, making the left colon and sigmoid a midline structure. Elevating the descending colon and drawing it medially is useful, as this keeps small bowel loops out of the way of the dissecting instrument and facilitates the dissection. In some patients, particularly very obese or otherwise large patients, it is difficult to reach high enough through the right lower quadrant port. For this reason, the surgeon's right-hand instrument is moved to the left lower quadrant port site. This permits greater reach along the descending colon.
Mobilization of the Splenic Flexure
Complete lateral mobilization of the left colon up to the splenic flexure is performed as an initial step. The descending colon is pulled medially using an atraumatic bowel clamp in the right lower quadrant port and the scissors are placed in the left iliac fossa port. A 5 mm left upper quadrant port may be necessary, particularly in those with a very high splenic flexure, or in very tall or obese individuals. The lateral attachments of the left colon are divided and the colon is dissected off the Gerota's fascia over the left kidney.
Once the lateral attachments of the colon have been freed, it is necessary to move medially and enter the lesser sac. Some surgeons prefer to perform this as an initial step before lateral mobilization. To enter the lesser sac, the patient is tilted to a slight reverse Trendelenburg position. An atraumatic bowel clamp is inserted through the right upper quadrant port. If the left upper quadrant port is available this is also used. The assistant holds up the greater omentum, toward its left side, like a cape. The surgeon grasps the transverse colon toward the left side using a grasper in the right lower quadrant port to aid the identification of the avascular plane between the greater omentum and the transverse mesocolon. Harmonic scalpel or monopolar scissors can be used through the left lower quadrant port to dissect this plane and enter the lesser sac. The surgeon usually moves to stand between the patient's legs for this part of the procedure. This dissection is continued toward the splenic flexure. Following separation of the omentum off the left side of the transverse colon, connection to the lateral dissection allows the splenic flexure to be fully mobilized. The colon at the flexure is retracted caudally and medially, and any remaining restraining attachments are divided.
Rectal Mobilization
The patient is returned to the Trendelenburg position, and the small bowel is reflected cranially. Atraumatic bowel clamps inserted through the left-sided ports are used to elevate the rectosigmoid colon out of the pelvis and away from the retroperitoneum and sacral promontory, to enable entry into the presacral space. The posterior aspect of the mesorectum can be identified and the mesorectal plane dissected with diathermy, preserving the hypogastric nerves as they pass down into the pelvis, anterior to the sacrum. Dissection continues down the presacral space in this avascular plane toward the pelvic floor.
Attention is now switched to the peritoneum on the right side of the rectum. This is divided into the level of the seminal vesicles or rectovaginal septum. This is repeated on the peritoneum on the left side of the rectum. This facilitates further posterior dissection along the back of the mesorectum to the pelvic floor, to a level inferior to the lower edge of the mesorectum, just posterior to the anal canal. For a low anterior resection, it is necessary to perform a total mesorectal excision and hence the rectum must be dissected down to the muscle tube of the rectum below the inferior extent of the mesorectum. In many cases, particularly in those who are obese or men with a narrow pelvis, some or all of the anterior and lateral dissection must be completed to get adequate visualization, to complete the posterior dissection.
An atraumatic bowel clamp through the left iliac fossa port is used to retract the peritoneum anterior to the rectum forward. The peritoneal dissection is continued from the free edge of the lateral peritoneal dissection, anteriorly. Lateral dissection is continued on both sides of the rectum and is extended anterior to the rectum, posterior to Denonvillier's fascia, separating the posterior vaginal wall from the anterior wall of the rectum or down to the level of the prostate in men. The difficulty of dissection will vary depending on the body habitus of the patient, the diameter of the pelvis, and the size of the tumor. Occasionally, rectal mobilization can be very difficult to perform laparoscopically. In some cases, it may need to be completed in an open manner through a small Pfannenstiel incision.
Division of Rectum
The lower rectum may be divided with a stapler either laparoscopically or by open surgery, depending on the ease of access related to the size of the pelvis. A rotaculator laparoscopic stapler may be used to divide the muscle tube of the rectum below the level of the mesorectum. The stapler is inserted through the right lower quadrant incision, and two firings of the stapler are usually required to divide the rectum. There is no residual mesorectum to divide at this level. A digital examination is performed to confirm the location of the distal staple line, and if there is any doubt about the adequacy of the distal margin, a rigid proctoscopy is performed.
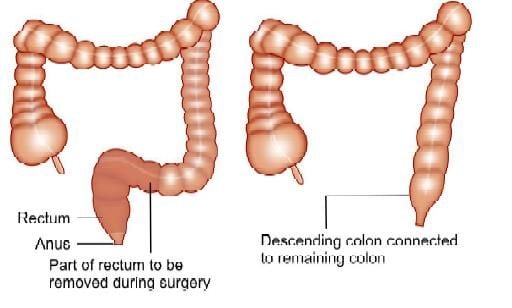
Low anterior resection
It is sometimes impossible to divide the rectum laparoscopically as the angulation of the endovascular stapler is limited to 45 degrees, necessitating the open division of the rectum. In some patients, getting an assistant to push up on the perineum with their hand may lift the pelvic floor enough to get the first cartridge of the stapler low enough. In some cases, placing a suprapubic port allows easier access with the stapler to allow the division of the rectum. Some patients are either too obese or have a very narrow pelvis or a long anal canal, and the stapler cannot be passed low enough. Two options exist. One is to perform a transanal intersphincteric dissection, remove the specimen, and then perform a handsewn coloanal anastomosis. The second is to perform a short Pfannenstiel incision, which allows a linear 30 mm stapler to be positioned and the rectum divided.
Extraction and Anastomosis
The specimen can be extracted either through a Pfannenstiel incision or a left iliac fossa incision; in both incisions, a wound protector is used in cases with a polyp or cancer to reduce the risk of tumor implantation in the wound. The left colon mesentery is divided with cautery. The left colon is divided and the specimen is removed. Pulsatile mesenteric bleeding is confirmed and the vessels ligated with 0 polyglycolate suture ties. Depending on the preference of the operating surgeon, a colonic pouch or coloplasty may be performed. A 2/0 Prolene purse-string suture is inserted into the distal end of the left colon or pouch, the anvil of a circular stapling gun inserted, and the purse-string suture is tied tightly. If a Pfannenstiel incision has been made, the coloanal anastomosis can be performed under direct vision and open manipulation following the insertion of a circular stapling gun into the rectal stump. If a left iliac fossa incision has been used, the colon is returned to the abdomen and the incision closed, the pneumoperitoneum recreated, and the anastomosis is formed laparoscopically. The anastomosis can be leak-tested by filling the pelvis with saline and inflating the neorectum using a proctoscope or bulb syringe.





