Laparoscopic Cholecystectomy During Pregnancy
The uses of laparoscopic cholecystectomy in pregnant women have been slow to gain wide acceptance for two reasons: one is the potential for mechanical problems related to the pregnant uterus and the other is fear of fetal injury resulting from instrumentation or the pneumoperitoneum. Laparoscopic cholecystectomy in the past was considered relatively contraindicated during pregnancy due to the potentially adverse side effects on the fetus. However, when complications arise, surgical intervention becomes mandatory. This intervention should be ideally performed during the second trimester of pregnancy where the operative risks are considered to be the lowest.
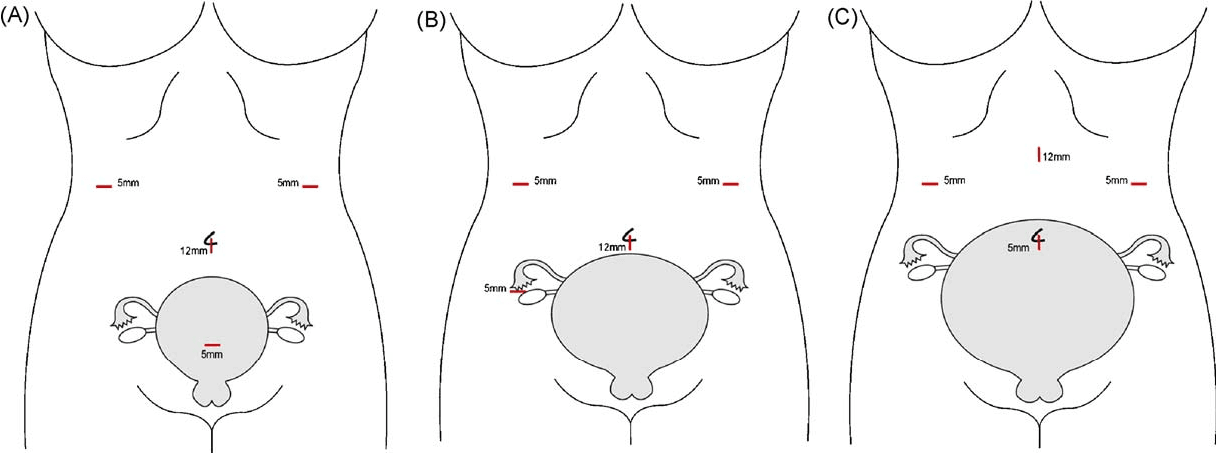
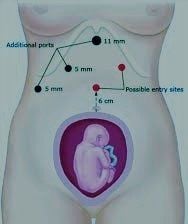
Laparoscopic cholecystectomy during pregnancy has been reported in many series of randomized controlled trials, with no specific complications related to the laparoscopic approach. If the site of initial abdominal access is adjusted according to fundal height and the abdominal wall is elevated during insertion, both the Hassan technique and Veress needle have been safely and effectively used.
Laparoscopic Cholecystectomy and Trimester of Pregnancy
Traditionally, the recommendation for Laparoscopic Cholecystectomy procedures during pregnancy has been to avoid surgery during the first and third trimesters to minimize the risk of spontaneous abortion and preterm labor, respectively. This has led some laparoscopic surgeon to suggest delaying Laparoscopic Cholecystectomy until the second trimester and that the gestational age limit for successful completion of laparoscopic surgery during pregnancy should be 26 to 28 weeks.
According to the SAGES guideline, these recommendations are not supported by good quality evidence; recent literature has demonstrated that pregnant patients may undergo laparoscopic surgery safely during any trimester without an increased risk to the mother or fetus.
When the pregnant patient is placed in a supine position, the gravid uterus places pressure on the inferior vena cava resulting in decreased venous return to the heart. This decrease in venous return leads to a reduction in cardiac output with concomitant maternal hypotension and decreased placental perfusion during surgery.
Delaying laparoscopic cholecystectomy until after delivery leads to high rates of recurrent symptoms, emergency department visits, and recurrent hospitalizations. Given the low risk of laparoscopic cholecystectomy to the pregnant woman and fetus, the procedure should be considered for all gravid women with symptomatic gallstones.
Postoperative Care
Most of the patients can be discharged the next day of surgery. The patient who has urinary retention, prolonged nausea, more pain, or difficulty in walking can be discharged after bowel sound. Three doses of broad-spectrum antibiotics should be administered.
The first dose infused one hour before surgery, second and third should be administered on consecutive days. Few patients may complain of pain over the tip of the shoulder after laparoscopic surgery. This is due to the irritation of diaphragm from CO2. Tramadol hydrochloride is advised in these patients. Most of the patients are able to resume there normal day-to-day activity within 48 to 72 hours after surgery. Generally, the patient can return to their sedentary work within a week.





