Laparoscopic CBD Exploration
Laparoscopic exploration of the common bile duct is performed either for the diagnosis or the treatment of common bile duct (CBD) stones. CBD stones demonstrated by laparoscopic intraoperative cholangiography, or laparoscopic ultrasonography are extracted either through the cystic duct or through choledochotomy. An alternative for the treatment of CBD stones is to perform an endoscopic sphincterotomy either before, during, or after laparoscopic cholecystectomy.
The main advantages of intraoperative cholangiography during cholecystectomy are:
• Detection of common bile duct stone
• Reduction of the incidence of residual common bile duct stone
• Delineation of the biliary anatomical variations at risk for bile duct injury.
An intraoperative cholangiogram is a highly sensitive tool for detecting choledocholithiasis, with an overall accuracy of 95 percent. Routine intraoperative cholangiography can diagnose unsuspected common bile duct stone in 1 to 14 percent (average 5%) of patients without indications for ductal exploration.
Intraoperative Cholangiography (IOC)
Techniques of Cholangiography
Cholangiograms obtained during laparoscopy are usually performed after catheterization of the cystic duct through a cholangioclamp (Storz Endoscopy, USA), or inserting a catheter through a hollow gasket needle pinned through the abdominal wall along the right subcostal margin. Difficulties in catheterization of the small cystic duct have led to consider cholecystocholangiography by direct puncture of the gallbladder as an alternative to cystic duct cholangiography. Cystic duct cholangiography is clearly better than cholecystocholangiography, and fluoroscopic imaging should be the standard for IOC. Until now, no specific clinically significant complications directly attributable to laparoscopic IOC have been reported. Expected success rates for laparoscopic IOC are in a 90 to 100 percent range. The inability to cannulate a narrow cystic duct is the main cause of failure. When performed after clipping (but not cutting) the anatomical structures identified by careful dissection such as the cystic artery and the cystic duct, a correctly interpreted IOC allows the detection of the most frequently reported cause of CBD injury, i.e. mistaken identification of a narrow main bile duct in place of the cystic duct.
Laparoscopic Ultrasonography (LUS)
Several studies on LUS have been published and conclusions of these studies favor LUS as compared to IOC. LUS is performed with a higher success rate, in less time, with better specificity, but with less precision with regard to the delineation of biliary tree anatomy. LUS is of little, if any, help in the diagnosis or prevention of bile duct injuries. While detection of smaller stones by LUS should increase its sensitivity, most of these stones are reputed to be flushed out through the sphincter and therefore the question arises if such small stones require any treatment at all. The specificity of LUS is higher (less false positives) than of IOC. When IOC and LUS were combined, there is a chance of less than 1 percent of false-positives. The question that comes to mind is whether LUS should be a screening test, and IOC performed only in case of doubt, or should IOC be the screening test, and LUS used only when IOC is of doubtful value? IOC performs better than LUS to delineate the entire biliary tree, from the intrahepatic tree to the pancreatic portion of the CBD. Injection of saline into the biliary tree enhanced the images obtained by LUS, especially in the distal portion of the bile duct.
Criteria for Routine Intraoperative Cholangiography
Preoperative Factors
• Failed endoscopic retrograde cholangiography + /- sphincterotomy
• Ultrasonographic findings
• Common bile duct size (> 6 mm)
• Choledocholithiasis
• History of jaundice or pancreatitis
• Elevated bilirubin, alkaline phosphatase, transaminases.
Intraoperative Factors
• Unclear anatomy
• Conversion to open cholecystectomy
• Dilated cystic duct over 4 mm.
Laparoscopic Extraction of Common Bile Duct Stones
Once detected during laparoscopic IOC, laparoscopic extraction of CBD stones is a logical extension of the procedure. Laparoscopic exploration of the CBD can be performed either through the cystic duct or by laparoscopic choledochotomy. A critical evaluation of the retrospective and prospective series on laparoscopic CBD exploration published since 1989 shows that both procedures are feasible and safe. Any comparisons between the two techniques would be fallacious because of their obviously different indications. Nonetheless, whenever feasible, laparoscopic transcystic CBD exploration best fulfills the expectancy of a mini-invasive approach. Laparoscopic management of CBD stones is considered technically difficult and demanding, requiring advanced laparoscopic skills as well as expensive endoscopic and radiological equipment. Endoscopic sphincterotomy is commonly proposed preoperatively as the alternative to surgery for CBD stones. Endoscopic sphincterotomy is indicated in patients with severe cholangitis for urgent drainage of infected bile, and in patients with retained stones after cholecystectomy. In open conventional surgery, controlled studies have not shown that ES, performed prior to surgery in patients with CBD stones in situ, was superior to single-step surgical management.
In case of preoperative diagnosis of common bile duct stone, options for management include:
• Preoperative ERCP and endoscopic sphincterotomy followed by laparoscopic cholecystectomy
• Conventional open common bile duct exploration
• Laparoscopic common bile duct exploration.
Today, most of the laparoscopic surgeons prefer the ‘‘single-stage’’ laparoscopic approach to choledocholithiasis. None of the randomized trials published to date concluded the superiority of endoscopic treatment alone or associated with surgery as compared to first-line surgical treatment. Immediate postoperative mortality was 2.6 percent in the endoscopic group as opposed to 1 percent in the surgical group. In a global analysis, the rate of major and minor complications was respectively 8 and 10 percent after endoscopy followed by surgery, and 8 and 15 percent after surgery alone.
Study of European Association for Endoscopic Surgery (EAES)
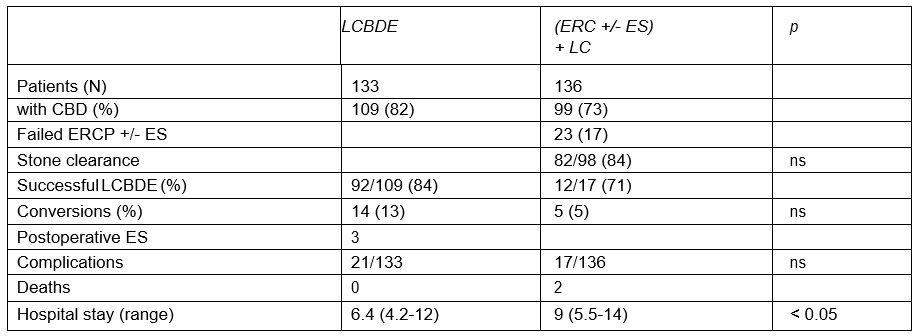
ERCP: Endoscopic retrograde cholangiopancreatography
Choledocholithiasis is found in approximately 10 to 20 percent of patients who undergo open cholecystectomies. In the era of laparoscopic cholecystectomies, the prevalence of CBD stones averages 6 percent (range; 3–10%). The incidence of choledocholithiasis increases over the age of 60. To achieve a maximal benefit to risk ratio, radiological investigations of the CBD should be restricted to patients with high suspicion of CBD stones, as determined by preoperative predictive scoring. Diagnostic and therapeutic choices in cholelithiasis must be considered conjointly. Data gathered from randomized trials have demonstrated that endoscopic sphincterotomy, as an additional procedure to surgery, does not improve the clinical results in patients fit for primary single-stage surgical treatment, whether performed laparoscopically or not. Discussions regarding the optimal way to treat patients with demonstrated CBD stones could lead to endless debate. Due to marginal differences between the endoscopic and surgical techniques, the number of patients needed to show any significant difference in terms of morbidity, mortality, or clearance rates would be enormous and therefore unrealistic. Cholangitis, jaundice, and CBD stones, as demonstrated on percutaneous ultrasonography, are the only reliable preoperative indicators available with the predictive value of CBD stones better than 50 percent. Severe cholangitis is an unquestionable indication for urgent endoscopic drainage, regardless of whether the CBD can be cleared of associated stones or not. The notorious insufficiencies of all other preoperative indicators for CBD stones should lead to a requiem for preoperative invasive diagnostic procedures, both in terms of risk, benefits, and costs.
All surgeons undertaking laparoscopic cholecystectomy must be able to perform an IOC. When IOC demonstrates CBD stones, appropriate treatment is decided according to available equipment and skills. Transcystic clearance of CBD stones is successful in at least two of three patients. In case of large (more than 20 mm) stones or other potential difficulties as regards postoperative endoscopic sphincterotomy such as a periampullary diverticulum, conversion to open surgery is indicated in the case of failed laparoscopic CBD exploration. In other cases, the available data do not allow any formal conclusions regarding the alternative between advanced laparoscopic biliary explorations and postoperative endoscopic sphincterotomy. The potential risk of reoperation in the case of failed postoperative endoscopic sphincterotomy might be more theoretical than practical. In one decision analysis, assessing different approaches to using ERC in patients undergoing laparoscopic cholecystectomy, postoperative ERC was associated with fewer costs and morbidity, but laparoscopic CBD exploration was not considered in the study design. Last, before embarking on a more invasive laparoscopic CBD exploration policy for small stones, irretrievable by the transcystic approach, surgeons must remember that asymptomatic migration does exist, even if the definitive fate of small CBD stones remains unknown at the present time. The potential security afforded by temporary biliary drainage still has to be balanced with its unavoidable morbidity.
Procedure
Patient Position
The patient is operated in the supine position with a steep head- up and left tilt. This typical positioning of laparoscopic choledochotomy should be achieved once the pneumoperitoneum has been established.
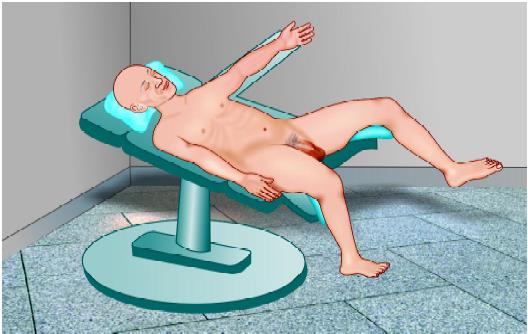
Patient position for laparoscopic choledochotomy
Port Position
The standard 4-port configuration for laparoscopic cholecystectomy is used. A fifth-port should be used later between the right midclavicular and epigastric port just below the subcostal margin for inserting the choledochoscope. The fundus of the gallbladder should be retracted towards the right shoulder and the Hartmann’s pouch should be retracted anterolaterally towards the right anterior superior iliac spine. Dissection began onto the neck of the gallbladder and continued proximally until the junction of the gallbladder with the cystic duct is clearly defined. Dissection should be continued proximally onto the cystic duct until there was an adequate length to perform cholangiogram. The cystic duct should be milked towards the gallbladder to dislodge any cystic duct stone into the gallbladder. Single titanium clip should be applied on the gallbladder side of the cystic duct to prevent any back slippage of a gallstone into the CBD and to prevent biliary spillage into the operative field.
A small nick in the cystic duct should be given with the help of hook scissors or microscissors. Intraoperative cholangiogram should be performed using a ureteric catheter (4-5 Fr) or an infant feeding tube (no 5-6), which is passed through the cystic duct into the CBD. After the insertion of the catheter, a titanium clip should be applied loosely to prevent any back leakage of the contrast medium. Digital C-arm fluoroscopy provided the real-time imaging of the biliary tree. In cases where the cystic duct could not be cannulated, the contrast was directly injected into the CBD through a 24 Fr lumbar puncture needle percutaneously. On cholangiogram, the surgeon must look for any filling defect—its size, site, number of bile duct stones, and free passage of contrast into the duodenum and for any anatomical variation of the biliary tree.
Transcystic or transcholedochal approach to remove CBD stones should be decided on the following factors. Common bile duct stone should be extracted with the help of Dormia basket/balloon catheter, irrigation/suctioning, or by simply manipulating bile duct using blunt forceps. After retrieving the stones, the cystic duct stump was closed with clips or extracorporeal knots and the gallbladder was removed in the usual manner.
For transcholedochal exploration after opening up of the Calot’s triangle, the anterior surface of the CBD should be dissected carefully and choledochotomy should be performed by a longitudinal incision with the help of endoscopic knife just below the insertion of the cystic duct into the bile duct. Before giving incision with knife mild coagulation of the serosal surface of CBD can help to prevent oozing. The single large stone can be retrieved by spontaneous evacuation while incising the bile duct, blunt instrumental pressure with atraumatic forceps can facilitate its easy removal.
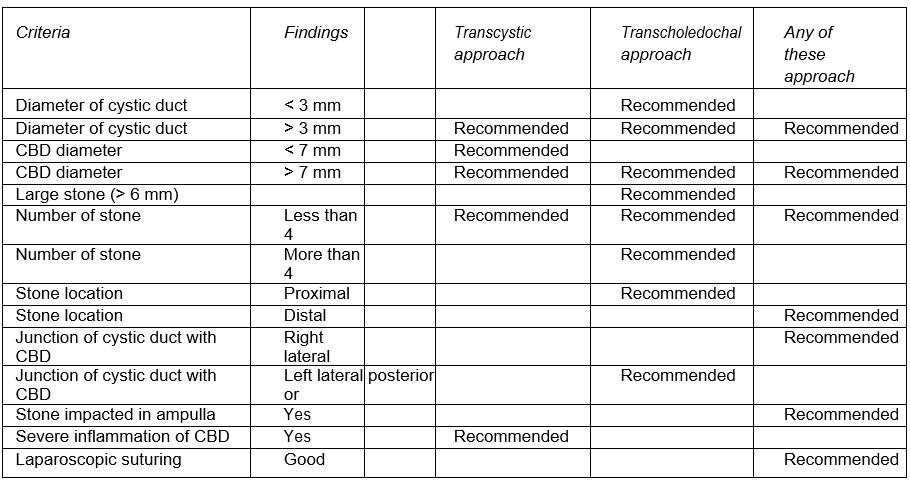
Transcystic versus transcholedochal approach for removal of CBD stone
In the case of multiple stones, Dormia basket, Fogarty balloon catheter, or irrigation and suction can be used to remove the stone. Completion cholangiography or choledochoscopy must be performed to assess any remaining stone. Some surgeon uses 5.5 Fr bronchoscope for this purpose but ideally, choledochoscope will give more flexibility.
Once all the stone is removed choledochotomy should be closed over a T tube with interrupted vicryl suture. In the case of single stone primary closure of CBD after assessing the clearance of the CBD can be tried. After bile duct closure, cholecystectomy should be performed in the usual manner. An intrahepatic nasogastric tube drain should be used routinely is this surgery which is usually removed on days 3 to 4 as the output decreased below 30 ml/day.
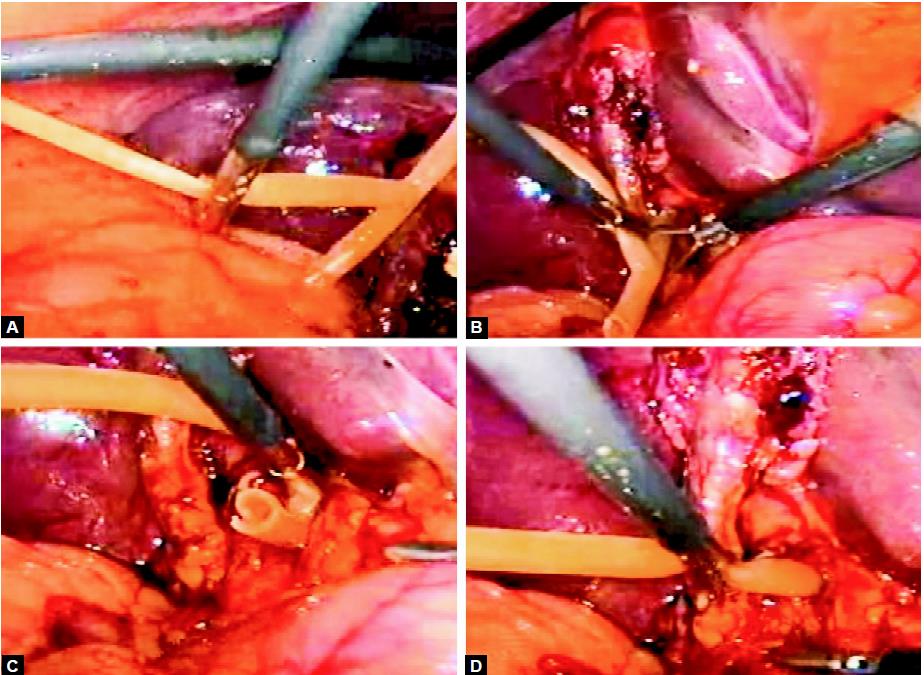
Introduction of T tube
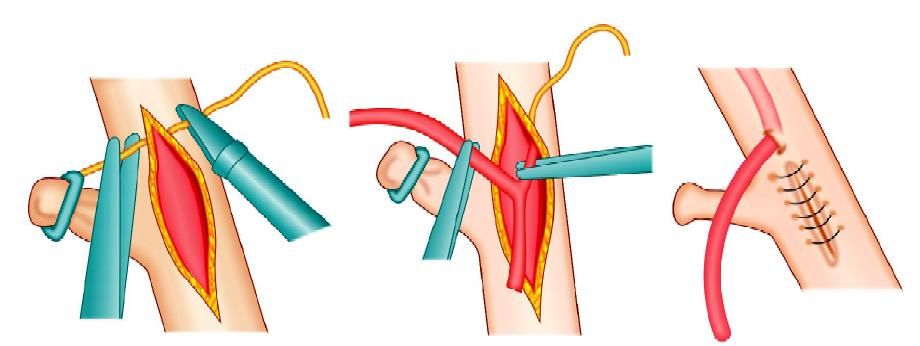
Diagrammatic representation of T tube fixation with an intracorporeal interrupted surgeons knot


