Indications of Laparoscopically Assisted Vaginal Hysterectomy
Indications of Laparoscopically Assisted Vaginal Hysterectomy (LAVH) are traditionally contraindications of vaginal hysterectomy.
Indications include:
• Previous pelvic surgery
• Endometriosis
• Previous CS
• Pelvic pain
• Suspected adnexal pathology
• Uterine myoma
• Ectopic pregnancy
• Acute or chronic pelvic inflammatory disease
• Minimum uterine mobility and limited vaginal access.
If a vaginal hysterectomy can be performed in the first place, there would be no point in adding the costs and complications of laparoscopy. Its greatest benefit is the potential to convert what would have been an abdominal hysterectomy into a vaginal hysterectomy. An abdominal hysterectomy requires both a vaginal incision and a four to six-inch-long incision in the abdomen, which is associated with greater postoperative discomfort and a longer recovery period than for a vaginal procedure. Another advantage of the LAVH may be the removal of the tubes and ovaries which on occasion may not be easily removed with a vaginal hysterectomy. The most common medical reasons for performing hysterectomies include uterine fibroids (30%), abnormal uterine bleeding (20%), endometriosis (20%), genital prolapse (15%) and chronic pelvic pain (10%). For most of these conditions, other treatments should first be considered, and hysterectomy should be reserved as a last resort. Laparoscopically assisted vaginal hysterectomy (LAVH) results in a significantly shorter hospital stay, with a much more rapid return to normal activities than total laparoscopic hysterectomy. The drug requirement to control pain and the level of pain patients experienced were also significantly less. Blood loss was not different for the two procedures. Postoperative recovery times and pain levels were assessed in 37 patients with a primary complaint of pelvic pain and diagnoses of fibroid uterus, adenomyosis, and severe endometriosis who underwent LAVH. Women reported an activity level of 8.7 on a scale of 1 to 10 (10 no limits on activity) by postoperative day 14. In another study, those undergoing abdominal hysterectomy had a mean uterine weight of 418 g compared with 150 g for those undergoing LAVH. The hospital stays after abdominal hysterectomy was 4.5 days and after LAVH 2.5 days. An important public policy issue now confronts us. As it is currently performed, LAVH is more expensive than TAH. The issue is whether the benefits of shorter convalescence and faster return to the workforce, shorter hospitalization, and less need for narcotics for postoperative pain outweigh the disadvantage of the higher cost. If total health care system costs are evaluated, the short-term disability costs of 2 weeks of recovery after laparoscopic hysterectomy should be compared with disability costs of 6 to 8 weeks of recovery after abdominal hysterectomy. For LAVH to be economically viable compared with TAH, savings in disability costs, and the increased contribution to the gross domestic product must offset the increased health care costs. In the current system, insurance companies and hospitals do not share in these benefits, only the costs. The economic impact of laparoscopic surgery must take into account both the cost to the hospital and insurance payers and these productivity and social issues. Insurance is based on a risk pool whereby the cost of a premium is based on the cost of treatment, not the ability of the subscriber to return to work. An economic and social cost-benefit analysis must be performed before decisions are made to modify or judge a procedure that provides substantial benefits to the patient. Since its introduction in 1989, continued improvement of techniques will likely progress rapidly so that LAVH will be performed on an outpatient basis for many women, and will result in shorter recovery time. Thus, the increased operating room time of approximately 46 minutes is significantly outweighed by the benefits available with the widespread application of this procedure.
Postoperative pain levels
 Wilcoxon’s signed-rank test.
Wilcoxon’s signed-rank test.
Ten-point activity scale: 1 = no pain, 10 = unbearable pain. S = significant at p < 0.005; NS = not significant at p <0.01
Postoperative activity levels

Wilcoxon’s signed-rank test.
Ten-point activity scale: 1 = extremely limited activity, 10 = no limits on activity
S = significant at p < 0.005; NS = not significant at p < 0.01
Classification
Garry and Reich Classification
• Type 1 Diagnostic lap + VH
• Type 2 lap vault suspension after VH
• Type 3 LAVH
• Type 4 LH (lap ligation of a uterine artery)
• Type 5 TLH
• Type 6 LSH (lap supracervical hysterectomy)
• Type 7 LHL (lap hysterectomy with lymphadenectomy)
• Type 8 LHL + O (as above + omentectomy)
• Type 9 RLH (radical lap hysterectomy)
Preoperative Measures
Patients are evaluated the same as that of any major surgery. Routine preoperative tests include a complete blood count with differential, serum electrolyte, bleeding time, and urinalysis. More comprehensive blood studies include thrombin time, partial thrombin time, ECG, chest X-ray, and endometrial biopsy. Mechanical and antibiotic bowel preparation is advised. Peglac powder 1 sachet with water a night prior to surgery is advised.
Patient Position
The patient should be in steep Trendelenburgs and lithotomy position. One assistant should remain between the legs of the patient to do uterine manipulation whenever required.

Pervaginal examination should be routine
Position of Surgical Team
Surgeon stand left to the patient, the camera assistant should be left to the surgeon. The second assistant should be the opposite side of the body of the patient. One more assistant is required between the legs to handle the uterine manipulator.
Surgical team position in LAVH
Port Position
A 10 mm umbilical port for the camera should be along the inferior crease. Two 5 mm ports should be placed at 5 cm away from umbilicus on either side. Sometime, an accessory port at the right or left iliac region may be needed according to need. The port position should be in accordance with the baseball diamond concept. If the left side of the tube has to be operated, one port should be in the right iliac fossa and another below left hypochondrium.

Port position for LAVH
Operative Technique
It is important throughout the procedure to be able to manipulate the uterus for optimal observation. Different types of uterine manipulators are available. Depending on the laparoscopic procedure, digital examination, probes, and sponge stick applicators are used in the cul-de-sac for the identification of structures during laparoscopy. The direction and location of both ureters should be identified as much as possible.

Laparoscopically assisted vaginal hysterectomy (LAVH) using bipolar
If adnexectomy is planned, following electrodesiccation and cutting of the round ligaments, 2 to 3 cm of the uterus, the infundibulopelvic ligament is desiccated and cut, taking progressive bites of tissue starting at pelvic brim and moving towards the round ligament. If the endoscopic linear stapler is used the adnexae is grasped with forceps, it is retracted medially and caudally to stretch and outline the infundibulopelvic ligament, which is grasped and secured with the stapler. The stapler is not fired until the contained tissue is identified and the ureter safety is confirmed. Once transected the staple line should be examined closely for any possible injury and hemostasis. Following infundibulopelvic ligament transaction the adnexae and uterine fundus are retracted in the opposite direction and the tissue of the upper broad ligament, including the round ligament, is grasped, secured and cut. The multifire GIA stapler can clamp and cut tissue efficiently. The device places six rows of small titanium staples and cuts the tissue in between, leaving three rows of staples on either side of the transected pedicle. This device leaves essentially bloodless pedicles. However, the instrument is disposable and expensive.

Successive desiccation and dissection
If the adnexae is planned to preserve, the round ligament is desiccated and cut approximately 2 cm from the uterus. The anterior leaf of the broad ligament is opened towards the vesicouterine fold and bladder flap is developed. The anterior leaf of the broad ligament is grasped with forceps, elevated, and dissected from the anterior lower uterine segment. The utero-ovarian ligament proximal tube and mesosalpinx are progressively dissected and the cut and the posterior leaf of the broad ligament is opened. Similarly, the round ligament fallopian tube and utero-ovarian ligament are grasped closed to their insertion into the uterus with an endoscopic linear stapler, then secured stapled and cut. The distal end of the stapler or bipolar forceps must be kept free of the bladder and ureter.
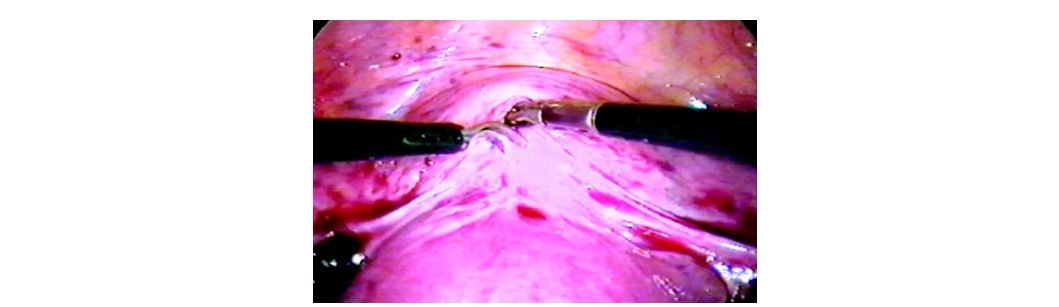
Dissection of bladder peritoneum
The ureterovesical junction is identified, grasped, and elevated with forceps while being cut with scissors. The bladder pillars are identified as desiccated and cut. The bladder can be completely freed from the uterus by pushing downward with the tip of a blunt probe along the vesicocervical plane until the anterior cul-de-sac is exposed completely. In patients with severe anterior cul-de-sac endometriosis, previous CS or adhesions, sharp dissection can be performed. Injecting 5 ml of indigo caramine in the patient’s bladder helps to detect bladder trauma. After dissecting the bladder from the uterus, the uterine vessels are identified desiccated and cut to free the lateral border of the uterus. If sutures, clips or linear staplers are used, it is important to fully skeletonize the vessel. As the uterine vessel is grasped and cut, the safety and position of the ureter should be checked. Ureter injury can be completely nullified if a ureteric catheter is introduced before the procedure. Cardinal ligament dissection must be carefully done as ureter and uterine artery falls just lateral to that. The linear stapler can be used only if the parametrium has been dissected with ample margins. Once the ureter is displaced laterally, the cardinal ligament tissue closest to the cervix is electrodesiccated and transacted. Alternatively, the linear stapler can be applied both on the uterine vessels and cardinal ligament.

Successive clamping and desiccation of uterine pedical through the vaginal route; (A) Valsaleum holding cervix; (B) Application of ligaSure clamp over left uterosacral; (C) Application of ligaSure over the right uterine stump; (D) Application of ligaSure over the left uterine stump

Opening of anterior and posterior leaf broad ligament
Colpotomy
A folded gauze in sponge forceps is used to mark the fornix. The vaginal wall is tented and transacted horizontally with a hook electrode.

Steps of colpotomy
Once the dissection is extended to the lower uterine segment or to the level of the cardinal ligament, the laparoscopic portion is temporarily terminated. Three vaginally speculum is used to get proper access for the vaginal part of LAVH. Once the uterus is removed, the vaginal vault is closed to ensure support of the vault; the vaginal angles are attached to the uterosacral and cardinal ligaments with 2-0 vicryl. Any co-existing cystocele or rectocele is repaired. A very large fibroid uterus should be debulked by morcellation for removal vaginally. It can be combined with laparoscopic adnexal surgery, e.g. ovariectomy or adhesiolysis. Once the vaginal surgery is completed again laparoscopic inspection of the pelvis is done.

Closure of vault by extracorporeal knot
Indications of Laparoscopically Assisted Vaginal Hysterectomy (LAVH) are traditionally contraindications of vaginal hysterectomy.
Indications include:
• Previous pelvic surgery
• Endometriosis
• Previous CS
• Pelvic pain
• Suspected adnexal pathology
• Uterine myoma
• Ectopic pregnancy
• Acute or chronic pelvic inflammatory disease
• Minimum uterine mobility and limited vaginal access.
If a vaginal hysterectomy can be performed in the first place, there would be no point in adding the costs and complications of laparoscopy. Its greatest benefit is the potential to convert what would have been an abdominal hysterectomy into a vaginal hysterectomy. An abdominal hysterectomy requires both a vaginal incision and a four to six-inch-long incision in the abdomen, which is associated with greater postoperative discomfort and a longer recovery period than for a vaginal procedure. Another advantage of the LAVH may be the removal of the tubes and ovaries which on occasion may not be easily removed with a vaginal hysterectomy. The most common medical reasons for performing hysterectomies include uterine fibroids (30%), abnormal uterine bleeding (20%), endometriosis (20%), genital prolapse (15%) and chronic pelvic pain (10%). For most of these conditions, other treatments should first be considered, and hysterectomy should be reserved as a last resort. Laparoscopically assisted vaginal hysterectomy (LAVH) results in a significantly shorter hospital stay, with a much more rapid return to normal activities than total laparoscopic hysterectomy. The drug requirement to control pain and the level of pain patients experienced were also significantly less. Blood loss was not different for the two procedures. Postoperative recovery times and pain levels were assessed in 37 patients with a primary complaint of pelvic pain and diagnoses of fibroid uterus, adenomyosis, and severe endometriosis who underwent LAVH. Women reported an activity level of 8.7 on a scale of 1 to 10 (10 no limits on activity) by postoperative day 14. In another study, those undergoing abdominal hysterectomy had a mean uterine weight of 418 g compared with 150 g for those undergoing LAVH. The hospital stays after abdominal hysterectomy was 4.5 days and after LAVH 2.5 days. An important public policy issue now confronts us. As it is currently performed, LAVH is more expensive than TAH. The issue is whether the benefits of shorter convalescence and faster return to the workforce, shorter hospitalization, and less need for narcotics for postoperative pain outweigh the disadvantage of the higher cost. If total health care system costs are evaluated, the short-term disability costs of 2 weeks of recovery after laparoscopic hysterectomy should be compared with disability costs of 6 to 8 weeks of recovery after abdominal hysterectomy. For LAVH to be economically viable compared with TAH, savings in disability costs, and the increased contribution to the gross domestic product must offset the increased health care costs. In the current system, insurance companies and hospitals do not share in these benefits, only the costs. The economic impact of laparoscopic surgery must take into account both the cost to the hospital and insurance payers and these productivity and social issues. Insurance is based on a risk pool whereby the cost of a premium is based on the cost of treatment, not the ability of the subscriber to return to work. An economic and social cost-benefit analysis must be performed before decisions are made to modify or judge a procedure that provides substantial benefits to the patient. Since its introduction in 1989, continued improvement of techniques will likely progress rapidly so that LAVH will be performed on an outpatient basis for many women, and will result in shorter recovery time. Thus, the increased operating room time of approximately 46 minutes is significantly outweighed by the benefits available with the widespread application of this procedure.
Postoperative pain levels
 Wilcoxon’s signed-rank test.
Wilcoxon’s signed-rank test. Ten-point activity scale: 1 = no pain, 10 = unbearable pain. S = significant at p < 0.005; NS = not significant at p <0.01
Postoperative activity levels

Wilcoxon’s signed-rank test.
Ten-point activity scale: 1 = extremely limited activity, 10 = no limits on activity
S = significant at p < 0.005; NS = not significant at p < 0.01
Classification
Garry and Reich Classification
• Type 1 Diagnostic lap + VH
• Type 2 lap vault suspension after VH
• Type 3 LAVH
• Type 4 LH (lap ligation of a uterine artery)
• Type 5 TLH
• Type 6 LSH (lap supracervical hysterectomy)
• Type 7 LHL (lap hysterectomy with lymphadenectomy)
• Type 8 LHL + O (as above + omentectomy)
• Type 9 RLH (radical lap hysterectomy)
Preoperative Measures
Patients are evaluated the same as that of any major surgery. Routine preoperative tests include a complete blood count with differential, serum electrolyte, bleeding time, and urinalysis. More comprehensive blood studies include thrombin time, partial thrombin time, ECG, chest X-ray, and endometrial biopsy. Mechanical and antibiotic bowel preparation is advised. Peglac powder 1 sachet with water a night prior to surgery is advised.
Patient Position
The patient should be in steep Trendelenburgs and lithotomy position. One assistant should remain between the legs of the patient to do uterine manipulation whenever required.

Pervaginal examination should be routine
Position of Surgical Team
Surgeon stand left to the patient, the camera assistant should be left to the surgeon. The second assistant should be the opposite side of the body of the patient. One more assistant is required between the legs to handle the uterine manipulator.
Surgical team position in LAVH
Port Position
A 10 mm umbilical port for the camera should be along the inferior crease. Two 5 mm ports should be placed at 5 cm away from umbilicus on either side. Sometime, an accessory port at the right or left iliac region may be needed according to need. The port position should be in accordance with the baseball diamond concept. If the left side of the tube has to be operated, one port should be in the right iliac fossa and another below left hypochondrium.

Port position for LAVH
Operative Technique
It is important throughout the procedure to be able to manipulate the uterus for optimal observation. Different types of uterine manipulators are available. Depending on the laparoscopic procedure, digital examination, probes, and sponge stick applicators are used in the cul-de-sac for the identification of structures during laparoscopy. The direction and location of both ureters should be identified as much as possible.

Laparoscopically assisted vaginal hysterectomy (LAVH) using bipolar
If adnexectomy is planned, following electrodesiccation and cutting of the round ligaments, 2 to 3 cm of the uterus, the infundibulopelvic ligament is desiccated and cut, taking progressive bites of tissue starting at pelvic brim and moving towards the round ligament. If the endoscopic linear stapler is used the adnexae is grasped with forceps, it is retracted medially and caudally to stretch and outline the infundibulopelvic ligament, which is grasped and secured with the stapler. The stapler is not fired until the contained tissue is identified and the ureter safety is confirmed. Once transected the staple line should be examined closely for any possible injury and hemostasis. Following infundibulopelvic ligament transaction the adnexae and uterine fundus are retracted in the opposite direction and the tissue of the upper broad ligament, including the round ligament, is grasped, secured and cut. The multifire GIA stapler can clamp and cut tissue efficiently. The device places six rows of small titanium staples and cuts the tissue in between, leaving three rows of staples on either side of the transected pedicle. This device leaves essentially bloodless pedicles. However, the instrument is disposable and expensive.

Successive desiccation and dissection
If the adnexae is planned to preserve, the round ligament is desiccated and cut approximately 2 cm from the uterus. The anterior leaf of the broad ligament is opened towards the vesicouterine fold and bladder flap is developed. The anterior leaf of the broad ligament is grasped with forceps, elevated, and dissected from the anterior lower uterine segment. The utero-ovarian ligament proximal tube and mesosalpinx are progressively dissected and the cut and the posterior leaf of the broad ligament is opened. Similarly, the round ligament fallopian tube and utero-ovarian ligament are grasped closed to their insertion into the uterus with an endoscopic linear stapler, then secured stapled and cut. The distal end of the stapler or bipolar forceps must be kept free of the bladder and ureter.
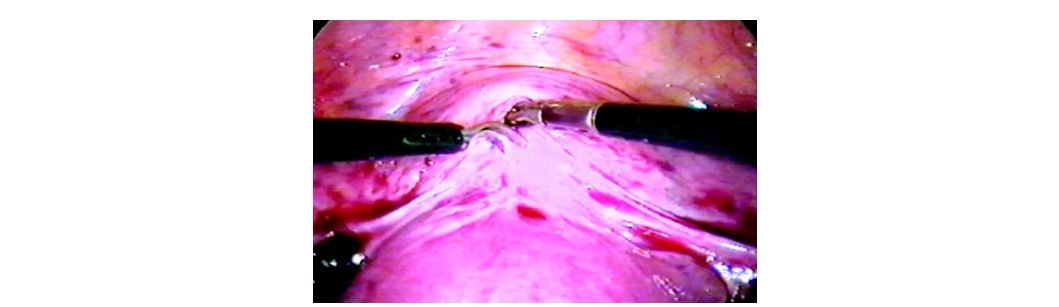
Dissection of bladder peritoneum
The ureterovesical junction is identified, grasped, and elevated with forceps while being cut with scissors. The bladder pillars are identified as desiccated and cut. The bladder can be completely freed from the uterus by pushing downward with the tip of a blunt probe along the vesicocervical plane until the anterior cul-de-sac is exposed completely. In patients with severe anterior cul-de-sac endometriosis, previous CS or adhesions, sharp dissection can be performed. Injecting 5 ml of indigo caramine in the patient’s bladder helps to detect bladder trauma. After dissecting the bladder from the uterus, the uterine vessels are identified desiccated and cut to free the lateral border of the uterus. If sutures, clips or linear staplers are used, it is important to fully skeletonize the vessel. As the uterine vessel is grasped and cut, the safety and position of the ureter should be checked. Ureter injury can be completely nullified if a ureteric catheter is introduced before the procedure. Cardinal ligament dissection must be carefully done as ureter and uterine artery falls just lateral to that. The linear stapler can be used only if the parametrium has been dissected with ample margins. Once the ureter is displaced laterally, the cardinal ligament tissue closest to the cervix is electrodesiccated and transacted. Alternatively, the linear stapler can be applied both on the uterine vessels and cardinal ligament.

Successive clamping and desiccation of uterine pedical through the vaginal route; (A) Valsaleum holding cervix; (B) Application of ligaSure clamp over left uterosacral; (C) Application of ligaSure over the right uterine stump; (D) Application of ligaSure over the left uterine stump

Opening of anterior and posterior leaf broad ligament
Colpotomy
A folded gauze in sponge forceps is used to mark the fornix. The vaginal wall is tented and transacted horizontally with a hook electrode.

Steps of colpotomy
Once the dissection is extended to the lower uterine segment or to the level of the cardinal ligament, the laparoscopic portion is temporarily terminated. Three vaginally speculum is used to get proper access for the vaginal part of LAVH. Once the uterus is removed, the vaginal vault is closed to ensure support of the vault; the vaginal angles are attached to the uterosacral and cardinal ligaments with 2-0 vicryl. Any co-existing cystocele or rectocele is repaired. A very large fibroid uterus should be debulked by morcellation for removal vaginally. It can be combined with laparoscopic adnexal surgery, e.g. ovariectomy or adhesiolysis. Once the vaginal surgery is completed again laparoscopic inspection of the pelvis is done.

Closure of vault by extracorporeal knot





