Laparoscopic Anatomy of Inguinal Hernia
In the lower abdomen, there are five peritoneal folds or ligaments which are seen through the laparoscope in the umbilicus. These ligaments are generally overlooked at the time of open surgery.
One Median Umbilical Ligament
In the midline, there is a median umbilical ligament extends from the mid of urinary bladder up to the umbilicus. The median umbilical ligament is obliterated urachus.

Diagrammatic representation of ligaments
Two Medial Umbilical Ligament One on Either Side
The paired medial umbilical ligament is an obliterated umbilical artery except where the superior vesical arteries are found in the pelvic portion. The medial umbilical ligaments are the most prominent fold of the peritoneum. Sometimes, it hangs down and obscures the vision of the lateral pelvic wall. These ligaments are important landmarks for the lateral extent of the urinary bladder.
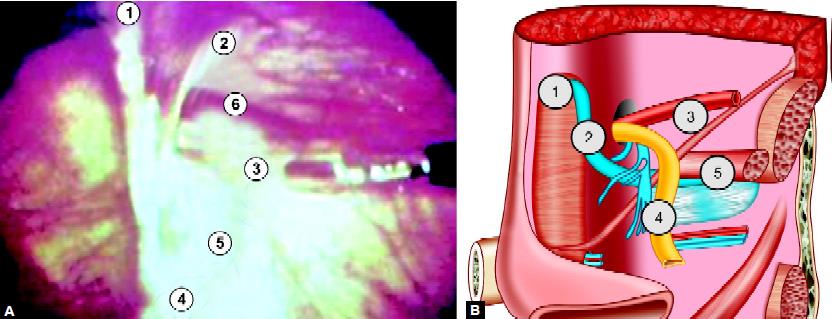
Important landmarks in laparoscopic hernia repair: (1) Medial umbilical ligament; (2) Inferior epigastric vessels; (3) Spermatic vessels; (4) Vas deferens; (5) External iliac vessels in “Triangle of doom”; (6) Indirect defect
Two Lateral Umbilical Ligaments
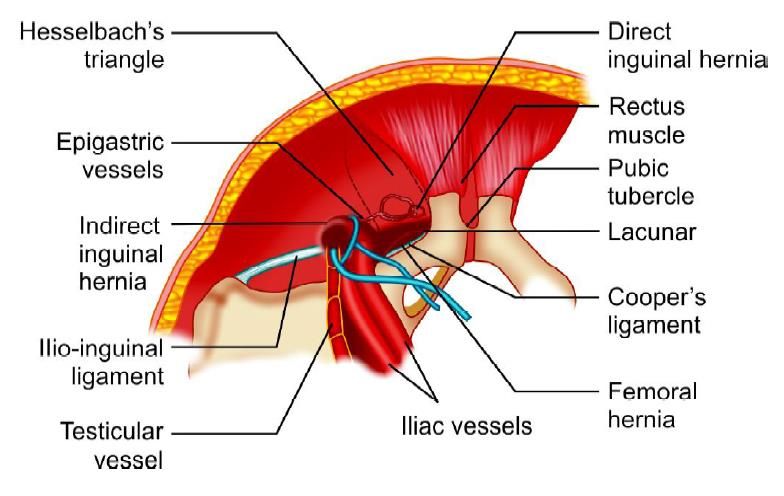
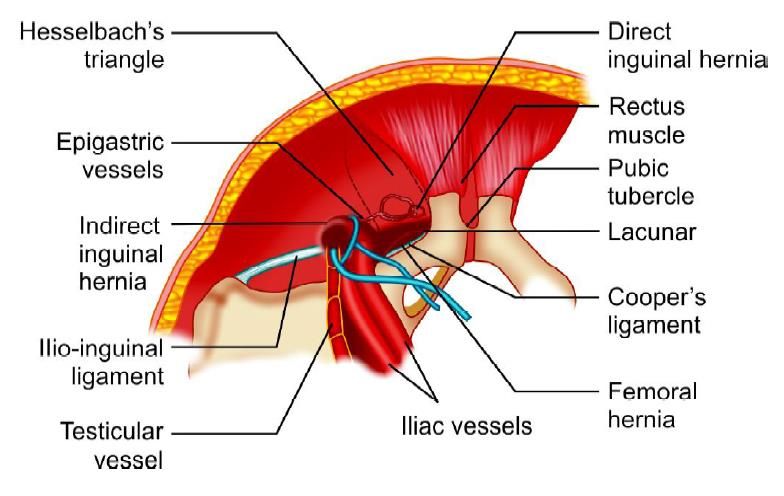
Lateral to the medial umbilical ligament, the less prominent paired lateral umbilical fold contains the inferior epigastric vessels. The inferior epigastric artery is a lateral border of Hesselbach's triangle and hence is a useful landmark for differentiating between direct and indirect hernia. Any defect lateral to the lateral umbilical ligament is an indirect hernia and medial to it is a direct inguinal hernia.
The femoral hernia is below and slightly medial to the lateral inguinal fossa, separated from it by the medial end of the iliopubic tract internally and the inguinal ligament externally. Important landmarks for extraperitoneal hernia dissection include the musculoaponeurotic layers of the abdominal wall, the bladder, Cooper’s ligament, and the iliopubic tract. The inferior epigastric artery and vein, the gonadal vessels and vas deferens should also be recognized. The space of Retzius lies between the vesicoumbilical fascia posteriorly and the posterior rectus sheath and pubic bone, anteriorly. This is the space first entered in the extraperitoneal repair of a hernia.
Three dangerous areas where stapling and electrosurgery should be avoided:
Triangle of Doom
The triangle of doom is defined by vas deferens medially, spermatic vessels laterally, and external iliac vessels inferiorly. This triangle contains external iliac artery and vessels, the deep circumflex iliac vein, the genital branch of the genitofemoral nerve and hidden by fascia, the femoral nerve. The staple should not be applied in this triangle otherwise; chances of mortality are there if these great vessels are injured.
Triangle of Doom
Triangle of Pain
Triangle of pain is defined as spermatic vessel medially, the iliopubic tract laterally and inferiorly the inferior edge of a skin incision. This triangle contains a lateral femoral cutaneous nerve and anterior femoral cutaneous nerve of the thigh. The staple in this area should be less because nerve entrapment can cause neuralgia.
Circle of Death
This is also called as corona Mortis and refers to vascular ring form by the anastomosis of an aberrant obturator artery with the normal obturator artery arising from a branch of the internal iliac artery. At the time of laparoscopic hernia, if this vessel is torn, both ends of the vessel can bleed profusely, because both arise from a major artery. The surgeon should remember these anatomic landmarks and the point of mesh fixation should be selected superiorly, laterally, and medially.
Indications of Laparoscopic Repair of Hernia
The indications for performing a laparoscopic hernia repair are essentially the same as repairing the hernia conventionally. There are, however, certain situations where laparoscopic hernia repair may offer definite benefits over conventional surgery to the patients. These include:
• Bilateral inguinal hernias
• Recurrent inguinal hernias.
In recurrent hernia, the surgery failure rate is as high as 25 to 30 percent, if again repaired by open surgery. The distorted anatomy after repeated surgery makes it more prone to recurrence and other complications like ischemic orchitis. In recurrent hernia, the laparoscopic approach offers repair through the inner healthy tissues with clear anatomical planes and thus, a lower failure rate. In laparoscopic bilateral repair with three ports technique, there is simultaneous access to both sides without any additional trocar placement. Even in patients with clinically unilateral defects after entering inside the abdominal cavity, there is 20 to 50 percent incidence of a contralateral asymptomatic hernia being found which can be repaired, simultaneously, without any additional morbidity of the patient.
Contraindications of Laparoscopic Repair of Hernia
• Nonreducible incarcerated inguinal hernia
• Prior laparoscopic herniorrhaphy
• Massive scrotal hernia
• Prior pelvic lymph node resection
• Prior groin irradiation.
Advantages of Laparoscopic Approach
• Tension-free repair that reinforces the entire myo-pectineal orifice
• Less tissue dissection and disruption of tissue planes
• Three ports are adequate for all type of hernias
• Less pain postoperatively
• Low intraoperatively and postoperative complications
• Early return to work.
Disadvantages of Open Method
• Requires 4 to 6 inches of incision at the groin
• Generally very painful, because of muscle spasm
• Considerable postoperative swelling of tissues in the groin, around the wound.
• Requires cutting through the skin, fat, and good muscles in order to gain access for repair, which in itself causes damage.
• Frequent complications of wound hematomas, wound infection, scrotal hematomas, and neuroma.
• Usually takes 6 to 8 weeks for recovery.
• Sometimes long-term disability may follow, e.g. neuralgia, neuroma, and testicular ischemia.
• Whether a flat mesh or a plug is used from the front, they do not hold themselves in place; what holds them in place are stitched, so the strength of the repair still depends on the stitches, not so much on the mesh or plug.
• Bilateral inguinal hernias require 2 incisions, doubling the pain; or 2 operations.
• Recurrent inguinal hernias are very difficult to operate open and more liable to complications.
• The size of the mesh used in open methods is limited by the natural fusion of muscles.
• All meshes and plugs shrink with time, and this works against all open methods.
Any method of repair must achieve 2 fundamental goals, removal of the sac from the defect and durable closure of the defect. In addition, the ideal method should achieve these with the least invasion, pain, or disturbance of normal anatomy. Laparoscopic repair in expert hands is now quite safe and effective and is an excellent alternative for patients with an inguinal hernia. It is the confusion that laparoscopic repair is more complex and is not widely available. The public needs to be educated as to its advantages. All surgeons agree that for bilateral or recurrent inguinal hernias, laparoscopic repair is unquestionably the method of choice. The argument against its use for unilateral or primary inguinal hernias is unfounded if it is the best for bilateral or recurrent hernias.
Types of Laparoscopic Hernia Repair
Many techniques were used to repair hernia like:
• Simple closure of the internal rings
• Plug and patch repair
• Intraperitoneal Onlay mesh repair
• Transabdominal preperitoneal mesh repair (TAPP)
• Total extraperitoneal repair (TEP).
The technique of transabdominal preperitoneal repair was first described by Arregui in 1991. In the transabdominal preperitoneal (TAPP) repair, the peritoneal cavity is entered, the peritoneum is dissected from the myopectineal orifice, mesh prosthesis is secured, and the peritoneal defect is closed. This technique has been criticized for exposing intraabdominal organs to potential complications, including small bowel injury and obstruction. The totally extraperitoneal (TEP) repair maintains peritoneal integrity, theoretically eliminating these risks while allowing direct visualization of the groin anatomy, which is critical for a successful repair. The TEP hernioplasty follows the basic principles of the open preperitoneal giant mesh repair, as first described by Stoppa in 1975 for the repair of bilateral hernias.
Patient Selection
The general anesthesia and the pneumoperitoneum required as part of the laparoscopic procedure do increase the risk in certain groups of patients. Most surgeons would not recommend laparoscopic hernia repair in those with pre-existing disease conditions. Patients with cardiac diseases and COPD should not be considered a good candidate for laparoscopy. The laparoscopic hernia repair may also be more difficult in patients who have had previous lower abdominal surgery. The elderly may also be at increased risk for complications with general anesthesia combined with pneumoperitoneum. If the patient is young or the hernia small, it does not matter how the hernia is repaired. Many surgeons agree that for bilateral or recurrent inguinal hernias, laparoscopic repair is unquestionably the method of choice. Laparoscopic surgery is not recommended for big irreducible and incarcerated hernia. Hernia repair like many other laparoscopic procedures should not be performed under local anesthesia. A small direct hernia can be performed under spinal anesthesia if TEP is planned but best anesthesia for laparoscopic hernia repair is GA.
In the lower abdomen, there are five peritoneal folds or ligaments which are seen through the laparoscope in the umbilicus. These ligaments are generally overlooked at the time of open surgery.
One Median Umbilical Ligament
In the midline, there is a median umbilical ligament extends from the mid of urinary bladder up to the umbilicus. The median umbilical ligament is obliterated urachus.

Diagrammatic representation of ligaments
Two Medial Umbilical Ligament One on Either Side
The paired medial umbilical ligament is an obliterated umbilical artery except where the superior vesical arteries are found in the pelvic portion. The medial umbilical ligaments are the most prominent fold of the peritoneum. Sometimes, it hangs down and obscures the vision of the lateral pelvic wall. These ligaments are important landmarks for the lateral extent of the urinary bladder.
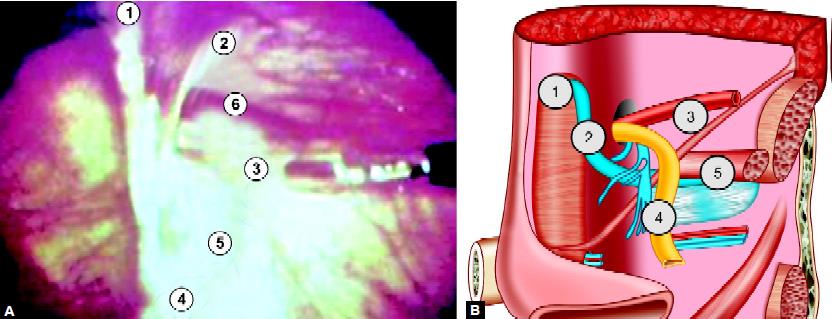
Important landmarks in laparoscopic hernia repair: (1) Medial umbilical ligament; (2) Inferior epigastric vessels; (3) Spermatic vessels; (4) Vas deferens; (5) External iliac vessels in “Triangle of doom”; (6) Indirect defect
Two Lateral Umbilical Ligaments
Lateral to the medial umbilical ligament, the less prominent paired lateral umbilical fold contains the inferior epigastric vessels. The inferior epigastric artery is a lateral border of Hesselbach's triangle and hence is a useful landmark for differentiating between direct and indirect hernia. Any defect lateral to the lateral umbilical ligament is an indirect hernia and medial to it is a direct inguinal hernia.
The femoral hernia is below and slightly medial to the lateral inguinal fossa, separated from it by the medial end of the iliopubic tract internally and the inguinal ligament externally. Important landmarks for extraperitoneal hernia dissection include the musculoaponeurotic layers of the abdominal wall, the bladder, Cooper’s ligament, and the iliopubic tract. The inferior epigastric artery and vein, the gonadal vessels and vas deferens should also be recognized. The space of Retzius lies between the vesicoumbilical fascia posteriorly and the posterior rectus sheath and pubic bone, anteriorly. This is the space first entered in the extraperitoneal repair of a hernia.
Three dangerous areas where stapling and electrosurgery should be avoided:
Triangle of Doom
The triangle of doom is defined by vas deferens medially, spermatic vessels laterally, and external iliac vessels inferiorly. This triangle contains external iliac artery and vessels, the deep circumflex iliac vein, the genital branch of the genitofemoral nerve and hidden by fascia, the femoral nerve. The staple should not be applied in this triangle otherwise; chances of mortality are there if these great vessels are injured.
Triangle of Doom
Triangle of Pain
Triangle of pain is defined as spermatic vessel medially, the iliopubic tract laterally and inferiorly the inferior edge of a skin incision. This triangle contains a lateral femoral cutaneous nerve and anterior femoral cutaneous nerve of the thigh. The staple in this area should be less because nerve entrapment can cause neuralgia.
Circle of Death
This is also called as corona Mortis and refers to vascular ring form by the anastomosis of an aberrant obturator artery with the normal obturator artery arising from a branch of the internal iliac artery. At the time of laparoscopic hernia, if this vessel is torn, both ends of the vessel can bleed profusely, because both arise from a major artery. The surgeon should remember these anatomic landmarks and the point of mesh fixation should be selected superiorly, laterally, and medially.
Indications of Laparoscopic Repair of Hernia
The indications for performing a laparoscopic hernia repair are essentially the same as repairing the hernia conventionally. There are, however, certain situations where laparoscopic hernia repair may offer definite benefits over conventional surgery to the patients. These include:
• Bilateral inguinal hernias
• Recurrent inguinal hernias.
In recurrent hernia, the surgery failure rate is as high as 25 to 30 percent, if again repaired by open surgery. The distorted anatomy after repeated surgery makes it more prone to recurrence and other complications like ischemic orchitis. In recurrent hernia, the laparoscopic approach offers repair through the inner healthy tissues with clear anatomical planes and thus, a lower failure rate. In laparoscopic bilateral repair with three ports technique, there is simultaneous access to both sides without any additional trocar placement. Even in patients with clinically unilateral defects after entering inside the abdominal cavity, there is 20 to 50 percent incidence of a contralateral asymptomatic hernia being found which can be repaired, simultaneously, without any additional morbidity of the patient.
Contraindications of Laparoscopic Repair of Hernia
• Nonreducible incarcerated inguinal hernia
• Prior laparoscopic herniorrhaphy
• Massive scrotal hernia
• Prior pelvic lymph node resection
• Prior groin irradiation.
Advantages of Laparoscopic Approach
• Tension-free repair that reinforces the entire myo-pectineal orifice
• Less tissue dissection and disruption of tissue planes
• Three ports are adequate for all type of hernias
• Less pain postoperatively
• Low intraoperatively and postoperative complications
• Early return to work.
Disadvantages of Open Method
• Requires 4 to 6 inches of incision at the groin
• Generally very painful, because of muscle spasm
• Considerable postoperative swelling of tissues in the groin, around the wound.
• Requires cutting through the skin, fat, and good muscles in order to gain access for repair, which in itself causes damage.
• Frequent complications of wound hematomas, wound infection, scrotal hematomas, and neuroma.
• Usually takes 6 to 8 weeks for recovery.
• Sometimes long-term disability may follow, e.g. neuralgia, neuroma, and testicular ischemia.
• Whether a flat mesh or a plug is used from the front, they do not hold themselves in place; what holds them in place are stitched, so the strength of the repair still depends on the stitches, not so much on the mesh or plug.
• Bilateral inguinal hernias require 2 incisions, doubling the pain; or 2 operations.
• Recurrent inguinal hernias are very difficult to operate open and more liable to complications.
• The size of the mesh used in open methods is limited by the natural fusion of muscles.
• All meshes and plugs shrink with time, and this works against all open methods.
Any method of repair must achieve 2 fundamental goals, removal of the sac from the defect and durable closure of the defect. In addition, the ideal method should achieve these with the least invasion, pain, or disturbance of normal anatomy. Laparoscopic repair in expert hands is now quite safe and effective and is an excellent alternative for patients with an inguinal hernia. It is the confusion that laparoscopic repair is more complex and is not widely available. The public needs to be educated as to its advantages. All surgeons agree that for bilateral or recurrent inguinal hernias, laparoscopic repair is unquestionably the method of choice. The argument against its use for unilateral or primary inguinal hernias is unfounded if it is the best for bilateral or recurrent hernias.
Types of Laparoscopic Hernia Repair
Many techniques were used to repair hernia like:
• Simple closure of the internal rings
• Plug and patch repair
• Intraperitoneal Onlay mesh repair
• Transabdominal preperitoneal mesh repair (TAPP)
• Total extraperitoneal repair (TEP).
The technique of transabdominal preperitoneal repair was first described by Arregui in 1991. In the transabdominal preperitoneal (TAPP) repair, the peritoneal cavity is entered, the peritoneum is dissected from the myopectineal orifice, mesh prosthesis is secured, and the peritoneal defect is closed. This technique has been criticized for exposing intraabdominal organs to potential complications, including small bowel injury and obstruction. The totally extraperitoneal (TEP) repair maintains peritoneal integrity, theoretically eliminating these risks while allowing direct visualization of the groin anatomy, which is critical for a successful repair. The TEP hernioplasty follows the basic principles of the open preperitoneal giant mesh repair, as first described by Stoppa in 1975 for the repair of bilateral hernias.
Patient Selection
The general anesthesia and the pneumoperitoneum required as part of the laparoscopic procedure do increase the risk in certain groups of patients. Most surgeons would not recommend laparoscopic hernia repair in those with pre-existing disease conditions. Patients with cardiac diseases and COPD should not be considered a good candidate for laparoscopy. The laparoscopic hernia repair may also be more difficult in patients who have had previous lower abdominal surgery. The elderly may also be at increased risk for complications with general anesthesia combined with pneumoperitoneum. If the patient is young or the hernia small, it does not matter how the hernia is repaired. Many surgeons agree that for bilateral or recurrent inguinal hernias, laparoscopic repair is unquestionably the method of choice. Laparoscopic surgery is not recommended for big irreducible and incarcerated hernia. Hernia repair like many other laparoscopic procedures should not be performed under local anesthesia. A small direct hernia can be performed under spinal anesthesia if TEP is planned but best anesthesia for laparoscopic hernia repair is GA.





