Laparoscopic Adhesiolysis
Peritoneal adhesion is a common cause of bowel obstruction, pelvic pain, and infertility. Proper technique of adhesiolysis is important and operating surgeons should have a clear concept of the mechanism of adhesion formation. Normal fibrinolytic activity prevents fibrinous attachments for 72 to 96 hours after surgery and mesothelial repair occurs within 5 days of trauma. Within these 5 days, a single cell layer of new peritoneum covers the injured raw area, replacing fibrinous exudates. However, if the fibrinous activity of the peritoneum is suppressed, fibroblasts will migrate, proliferate, and form fibrous adhesion. Collagen is deposited and neovascular formation starts.
The most important factors which suppress fibrinolytic activity and promote adhesion formation are:
• Port wound just above the target of dissection
• Tissue ischemia
• Drying of serosal surfaces
• Excessive suturing omental patches
• Traction of the peritoneum
• Blood clots, stones or dead tissue retained inside
• Prolonged operation
• Visceral injury
• Infection
• Delayed postoperative mobilization of the patient
• Postoperative pain due to inadequate analgesia.
Contradictions
• Hemodynamic instability
• Uncorrected coagulopathy
• Severe cardiopulmonary disease
• Abdominal wall infection
• Multiple previous upper abdominal procedures
• Late pregnancy.
Patient Position
The anesthetized patient is placed on the operating table with the legs straight or lithotomy position if female. The lithotomy position will allow the gynecologists and assistant to work simultaneously and uterine manipulation would be possible. The thighs must not be flexed onto the abdominal wall as they would be in the full lithotomy position used for other open surgical gynecological procedures. The operating table is tilted head up or down by approximately 15° depending on the main area of examination. Compression bandage may be used on the leg during the operation to prevent thromboembolism especially if the patient is in a lithotomy position.
Position of the Surgical Team
Before starting diagnostic laparoscopy the best guess is made about the quadrant in which adhesion is more likely to be found. The surgeon should stand opposite to this quadrant to allow a direct view into this quadrant. If the pathology is more likely in the pelvic cavity the surgeon stands on the left side of the patient. The first assistant, whose main task is to position the video camera, is also on the patient’s left side. The instrument trolley is placed on the patient’s left, allowing the scrub nurse to assist with placing the appropriate instruments in the operating ports. Television monitors are positioned on either side of the top end of the operating table at a suitable height for surgeon, anesthetists, as well as assistant to see the procedure.
Port Position
For the adhesiolysis of gynecological purposes, generally, one optical port in umbilicus and two 5 mm port in left and right iliac fossa should be introduced according to the baseball diamond concept after visualizing the target of dissection. The Port should be in a position to provide an elevation angle of 30° and a manipulation angle of 60°, which is ergonomically better. Some gynecologists use a suprapubic port, with suprapubic port, the elevation angle of the instrument, and tubal structure is 90° and hence lifting up of ovary and tube may be difficult without grasping it.
A three-port approach should be used if there is any difficulty in manipulation with two ports especially in case of extensive adhesion.
• 10 mm umbilical (optical)
• 5 mm suprapubic
• 5 mm right hypochondrium.
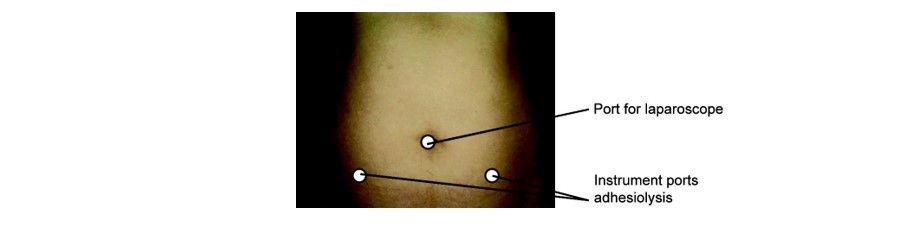
Three ports for pelvic adhesiolysis
A 30° telescope is employed in most instances, as this facilitates easier inspection of the deeper peritoneal cavity and abdominal organs. The secondary ports are inserted under laparoscopic vision. The selected site on the abdominal wall is identified by finger indentation of the parietal peritoneum. The open technique for trocar insertion is recommended if extensive adhesion is suspected. At the time of laparoscopic adhesiolysis, the surgeon should try to be very gentle with the tubal structure and bowel so that re adhesion will not form and stricture of the tube will not occur. Viewing of lateral pelvic organs is helped by the manipulation of mobile structure with a second port introduced through the left iliac fossa port.
Laparoscopic Adhesiolysis
Animal studies have proved that laparoscopy leads to less adhesion formation compared to open surgery. The less adhesion formation after laparoscopic surgery is because retraction is not used much, packing of the abdominal cavity is not required that can damage peritoneum. In laparoscopic surgery, there is less chance of drying of tissue because the inside environment is cut off from outside. Also, excellent visualization and magnification result in less tissue injury and adhesion. In laparoscopy, port wound and wound at the target of dissection are far away from each other so the chances of adhesion are less to the peritoneum because for adhesion both the layer which tends to adhere should be in contact. At least three ports should be used to perform laparoscopic adhesiolysis. After access and introduction of a telescope, two other ports should be introduced according to the baseball diamond concept keeping in mind, the center of adhesion as a target of dissection. If the adhesion is thin and avascular, it is easily lysed and the chances of recurrence are not much. In contrast, if adhesion is thick and highly vascular it is difficult to separate. Theses adhesion requires the use of energy (Ultrasonic dissector, Unipolar, or Bipolar). After achieving hemostasis sharp dissection with scissors are necessary. An atraumatic grasper is introduced to hold the adhesion or involved organ. It should be stretched gently and boundaries of adhesion are identified. The avascular area is chosen with the close-up magnified view of the telescope. The opposite trocar on the side of the surgeon is used for scissors and adhesion should be cut close to the affected organ. Vascular adhesions should be coagulated using an electrosurgical instrument preferably, bipolar. Scissors should be used only if flimsy avascular adhesion is found. Thick vascular adhesion first should be tried with blunt dissection, otherwise, it must be coagulated before being cut. A suction irrigation instrument is good if blunt dissection is thought.
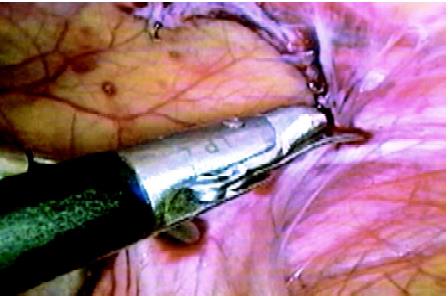
Sharp dissection with scissors if the bowel is involved
Bowel injury is common during enteroclysis and patients who have a history of the previous laparotomy should undergo bowel preparation. If injury results enterorrhaphy can be accomplished with one layer closure using vicryl. Details of intracorporeal suturing can be found in the chapter of laparoscopic suturing and knotting. After adhesiolysis, some fluid can be left inside to prevent a recurrence. Steroids and antihistamines were tried but are used infrequently because of adverse effects delayed wound healing and high-risk of dehiscence. High molecular weight dextran was tried to prevent re-adhesion because it is absorbed over a period of 7 to 10 days. Its osmotic effect draws the fluid into the peritoneal cavity and so the mobile peritoneal organ floats reducing adherence between intraperitoneal organs. Although the study in animals has demonstrated reduced postoperative adhesion, it is not fully confirmed for its efficacy. The adhesion barrier membrane was also tried. These absorbable membrane separate peritoneal membrane from adhered organ and thus prevent fibrous bands from binding different structures. Two such materials are Interceed and Gore-Tex. Interceed is an absorbable fabric of oxidized regenerated cellulose, and Gore-Tex is a nonabsorbable, nonreactive surgical membrane. Animal studies have demonstrated good results using these membranes.
Peritoneal adhesion is a common cause of bowel obstruction, pelvic pain, and infertility. Proper technique of adhesiolysis is important and operating surgeons should have a clear concept of the mechanism of adhesion formation. Normal fibrinolytic activity prevents fibrinous attachments for 72 to 96 hours after surgery and mesothelial repair occurs within 5 days of trauma. Within these 5 days, a single cell layer of new peritoneum covers the injured raw area, replacing fibrinous exudates. However, if the fibrinous activity of the peritoneum is suppressed, fibroblasts will migrate, proliferate, and form fibrous adhesion. Collagen is deposited and neovascular formation starts.
The most important factors which suppress fibrinolytic activity and promote adhesion formation are:
• Port wound just above the target of dissection
• Tissue ischemia
• Drying of serosal surfaces
• Excessive suturing omental patches
• Traction of the peritoneum
• Blood clots, stones or dead tissue retained inside
• Prolonged operation
• Visceral injury
• Infection
• Delayed postoperative mobilization of the patient
• Postoperative pain due to inadequate analgesia.
Contradictions
• Hemodynamic instability
• Uncorrected coagulopathy
• Severe cardiopulmonary disease
• Abdominal wall infection
• Multiple previous upper abdominal procedures
• Late pregnancy.
Patient Position
The anesthetized patient is placed on the operating table with the legs straight or lithotomy position if female. The lithotomy position will allow the gynecologists and assistant to work simultaneously and uterine manipulation would be possible. The thighs must not be flexed onto the abdominal wall as they would be in the full lithotomy position used for other open surgical gynecological procedures. The operating table is tilted head up or down by approximately 15° depending on the main area of examination. Compression bandage may be used on the leg during the operation to prevent thromboembolism especially if the patient is in a lithotomy position.
Position of the Surgical Team
Before starting diagnostic laparoscopy the best guess is made about the quadrant in which adhesion is more likely to be found. The surgeon should stand opposite to this quadrant to allow a direct view into this quadrant. If the pathology is more likely in the pelvic cavity the surgeon stands on the left side of the patient. The first assistant, whose main task is to position the video camera, is also on the patient’s left side. The instrument trolley is placed on the patient’s left, allowing the scrub nurse to assist with placing the appropriate instruments in the operating ports. Television monitors are positioned on either side of the top end of the operating table at a suitable height for surgeon, anesthetists, as well as assistant to see the procedure.
Port Position
For the adhesiolysis of gynecological purposes, generally, one optical port in umbilicus and two 5 mm port in left and right iliac fossa should be introduced according to the baseball diamond concept after visualizing the target of dissection. The Port should be in a position to provide an elevation angle of 30° and a manipulation angle of 60°, which is ergonomically better. Some gynecologists use a suprapubic port, with suprapubic port, the elevation angle of the instrument, and tubal structure is 90° and hence lifting up of ovary and tube may be difficult without grasping it.
A three-port approach should be used if there is any difficulty in manipulation with two ports especially in case of extensive adhesion.
• 10 mm umbilical (optical)
• 5 mm suprapubic
• 5 mm right hypochondrium.
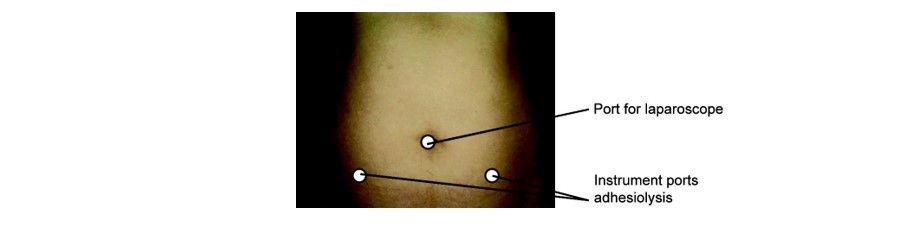
Three ports for pelvic adhesiolysis
A 30° telescope is employed in most instances, as this facilitates easier inspection of the deeper peritoneal cavity and abdominal organs. The secondary ports are inserted under laparoscopic vision. The selected site on the abdominal wall is identified by finger indentation of the parietal peritoneum. The open technique for trocar insertion is recommended if extensive adhesion is suspected. At the time of laparoscopic adhesiolysis, the surgeon should try to be very gentle with the tubal structure and bowel so that re adhesion will not form and stricture of the tube will not occur. Viewing of lateral pelvic organs is helped by the manipulation of mobile structure with a second port introduced through the left iliac fossa port.
Laparoscopic Adhesiolysis
Animal studies have proved that laparoscopy leads to less adhesion formation compared to open surgery. The less adhesion formation after laparoscopic surgery is because retraction is not used much, packing of the abdominal cavity is not required that can damage peritoneum. In laparoscopic surgery, there is less chance of drying of tissue because the inside environment is cut off from outside. Also, excellent visualization and magnification result in less tissue injury and adhesion. In laparoscopy, port wound and wound at the target of dissection are far away from each other so the chances of adhesion are less to the peritoneum because for adhesion both the layer which tends to adhere should be in contact. At least three ports should be used to perform laparoscopic adhesiolysis. After access and introduction of a telescope, two other ports should be introduced according to the baseball diamond concept keeping in mind, the center of adhesion as a target of dissection. If the adhesion is thin and avascular, it is easily lysed and the chances of recurrence are not much. In contrast, if adhesion is thick and highly vascular it is difficult to separate. Theses adhesion requires the use of energy (Ultrasonic dissector, Unipolar, or Bipolar). After achieving hemostasis sharp dissection with scissors are necessary. An atraumatic grasper is introduced to hold the adhesion or involved organ. It should be stretched gently and boundaries of adhesion are identified. The avascular area is chosen with the close-up magnified view of the telescope. The opposite trocar on the side of the surgeon is used for scissors and adhesion should be cut close to the affected organ. Vascular adhesions should be coagulated using an electrosurgical instrument preferably, bipolar. Scissors should be used only if flimsy avascular adhesion is found. Thick vascular adhesion first should be tried with blunt dissection, otherwise, it must be coagulated before being cut. A suction irrigation instrument is good if blunt dissection is thought.
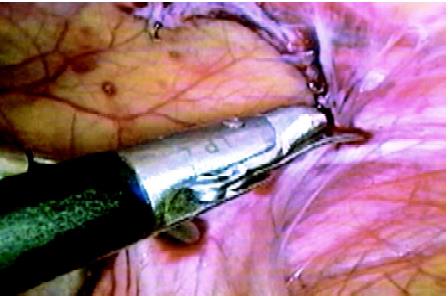
Sharp dissection with scissors if the bowel is involved
Bowel injury is common during enteroclysis and patients who have a history of the previous laparotomy should undergo bowel preparation. If injury results enterorrhaphy can be accomplished with one layer closure using vicryl. Details of intracorporeal suturing can be found in the chapter of laparoscopic suturing and knotting. After adhesiolysis, some fluid can be left inside to prevent a recurrence. Steroids and antihistamines were tried but are used infrequently because of adverse effects delayed wound healing and high-risk of dehiscence. High molecular weight dextran was tried to prevent re-adhesion because it is absorbed over a period of 7 to 10 days. Its osmotic effect draws the fluid into the peritoneal cavity and so the mobile peritoneal organ floats reducing adherence between intraperitoneal organs. Although the study in animals has demonstrated reduced postoperative adhesion, it is not fully confirmed for its efficacy. The adhesion barrier membrane was also tried. These absorbable membrane separate peritoneal membrane from adhered organ and thus prevent fibrous bands from binding different structures. Two such materials are Interceed and Gore-Tex. Interceed is an absorbable fabric of oxidized regenerated cellulose, and Gore-Tex is a nonabsorbable, nonreactive surgical membrane. Animal studies have demonstrated good results using these membranes.


